PREGNANT WOMEN IN STATE PRISONS AND LOCAL JAILS
Federal Assistance to Support Their Care
Report to Congressional Requesters
October 2024
GAO-25-106404
United States Government Accountability Office
View GAO‑25‑106404. For more information, contact Gretta L. Goodwin, 202-512-8777, GoodwinG@gao.gov
Highlights of GAO‑25‑106404, a report to congressional requesters
October 2024
Pregnant women in STATE PRISONS AND LOCAL JAILS
Federal Assistance to Support Their Care
Why GAO Did This Study
According to HHS, the U.S. has one of the highest maternal mortality rates among high-income nations, increasing rates of complications from pregnancy or childbirth, and persistent racial disparities in such outcomes. The U.S. also incarcerates women at the highest rate in the world, and the vast majority reside in state prisons or local jails.
GAO was asked to review maternal health care in state prisons and local jails. This report describes, among other issues, (1) available data on incarcerated pregnant women, (2) available federal support, and (3) challenges to providing care to this population and opportunities to enhance care.
GAO reviewed (1) existing available data on pregnant women incarcerated in state prisons and local jails, (2) federal grant information, and (3) relevant studies and peer reviewed articles. GAO also interviewed officials representing 9 state prisons and 9 local jails from a nongeneralizable sample of 12 states about maternal health care in their facilities. GAO visited prisons and jails in 3 states and interviewed 27 incarcerated pregnant and postpartum women about the care they received.
What GAO Found
Comprehensive national data on pregnant women incarcerated in state prisons and local jails do not exist. For example:
· Limited data reported by the Department of Justice (DOJ) indicates that about 4 percent of women in state prisons in 2016 and 5 percent of women in local jails in 2002 were pregnant at the time of admission. DOJ did not report on the demographics—such as race or ethnicity—or pregnancy outcomes of these women.
· The Department of Health and Human Services (HHS) collects near national-level data on maternal health and pregnancy outcomes, but none of these efforts have systematic indicators to identify incarcerated pregnant women.
· Additionally, officials representing selected state prisons and local jails told GAO that they collect some information on pregnant women, such as pregnancy status at admission. However, the data are limited due to challenges they face with collecting, analyzing, and reporting data.
However, DOJ currently has an effort underway to collect more data through a voluntary survey of state prisons and expects to issue a report in 2025. The survey will request the count of women tested for pregnancy at admission and the number of those tests that are positive, among other things.
According to HHS and DOJ officials, five HHS and 10 DOJ grant programs could be used to support maternal health care in state prisons and local jails during fiscal years 2018 through 2023, the most recent data available at the time of GAO’s review.
· The purposes of HHS’s five grant programs include providing health and education services to pregnant women and children, among other purposes. According to HHS officials, at least 23 of its grant awards were used to provide maternal health care in state prisons or local jails during this time. For example, one HHS grant recipient reported using grant funds to support its prison nursery, where eligible incarcerated mothers reside with their babies until the mother’s release from incarceration, up to 36 months.
· The primary purpose of DOJ’s 10 grant programs is to enhance substance use and other behavioral health treatments and improve reentry outcomes for people leaving prisons and jails. DOJ officials were not aware of, and GAO found no indication that, any of its grant funds were used to support maternal health care in state prisons and local jails.
Challenges and opportunities exist for providing maternal health care in state prisons and local jails. For example, officials representing three prisons reported and two peer reviewed articles GAO reviewed identified challenges with coordinating transportation for medical appointments for pregnant women that occur outside their facilities, which can delay or impede women’s access to maternal health care. Relevant literature also identified opportunities to address challenges, such as expanding program offerings to support pregnant women. Examples of such programs include mental health treatment, lactation, and mother-infant bonding programs.
Abbreviations
ACF Administration for Children and Families
ACOG American College of Obstetricians and Gynecologists
BJS Bureau of Justice Statistics
BOP Bureau of Prisons
COVID-19 Coronavirus Disease 2019
DOC Department of Corrections
DOJ Department of Justice
HHS Department of Health and Human Services
HRSA Health Resources and Services Administration
NGO nongovernmental organization
OJP Office of Justice Programs
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
October 2, 2024
Congressional Requesters
According to the Department of Health and Human Services (HHS), the U.S. is facing a maternal health crisis. The U.S. has one of the highest maternal mortality rates among high-income nations, increasing rates of complications from pregnancy or childbirth, and persistent racial disparities in such outcomes.[1] For example, we previously reported that HHS data indicate the maternal mortality rate among non-Hispanic Black or African American women was about 2.5 times greater than non-Hispanic White women in 2020 and 2021.[2]
In addition, according to the Institute for Crime & Justice Policy Research, the U.S. also incarcerates women at the highest rate in the world.[3] This includes around 168,800 women in federal and state prisons or local jails in 2022, according to the Department of Justice’s (DOJ) Bureau of Justice Statistics (BJS). The most recent available BJS data on pregnancy also indicates that about 4 percent of women in state prisons and about 5 percent of women in local jails reported being pregnant at the time of admission.[4] The vast majority of incarcerated individuals reside in state or local correctional facilities.[5]
The White House released the Blueprint for Addressing the Maternal Health Crisis (blueprint) in June 2022.[6] The blueprint identifies goals and actions the federal government is taking, or plans to undertake, to decrease rates of maternal mortality and morbidity; reduce disparities in maternal health outcomes, such as racial and socioeconomic disparities; and improve the overall experience of pregnancy, birth, and the postpartum period for women across the U.S.[7] The blueprint includes several federal efforts that could support maternal health care for incarcerated women, such as training and hiring doulas.[8]
We previously reviewed issues related to pregnant women in federal custody. In 2020, we issued a report on the care of pregnant women in Department of Homeland Security immigration detention facilities.[9] In 2021, we reported on pregnant women in DOJ custody.[10] Further, in 2021, 2022, and 2024 we reported on maternal morbidity and mortality, and disparities in maternal health outcomes, including racial and rural-urban disparities.[11]
You asked us to review issues related to maternal health care in state prisons and local jails. This report addresses the following questions:
1. What data are available on the characteristics of incarcerated pregnant women and pregnancy outcomes in state prisons and local jails?
2. What federal assistance can be used to support maternal health care in state prisons and local jails?
3. How do selected state prisons and local jails provide maternal health care for incarcerated pregnant women?
4. What are the identified and reported challenges and opportunities to providing maternal health care to incarcerated pregnant women?
To address all four questions, we interviewed officials representing nine state prisons and nine local jails from across 12 states about maternal health care in their facilities.[12] We selected this nongeneralizable sample of states based on several factors. For example, we included states with a range of state female incarceration rates that generally had higher numbers of women under the jurisdiction of state correctional authorities or incarcerated in local jails.[13]
We conducted semi-structured interviews with officials representing all selected facilities in which we asked about (1) the data they collect on pregnant women in their facilities, (2) their knowledge of available federal assistance to support maternal health care for this population, and (3) the provision of maternal health care in their facilities—including any challenges they may experience in providing this care. The information these officials provided was reported to us during interviews, in written responses, or in relevant documentation. We report perspectives from officials representing state prisons and local jails in the aggregate, due to the sensitivity of some of the information we received about pregnant women and maternal health care at these facilities. In addition, we conducted in-person visits to prisons and jails in three states between June and November 2023.[14] In the states where we visited prisons and jails in-person, we also conducted semi-structured interviews with 27 incarcerated pregnant and postpartum women. We asked officials from the facilities to identify women who were pregnant or postpartum at the time of our visits and to ask for volunteers to participate. We also asked, if possible, to meet with women that reflect the facility’s racial and ethnic diversity. We asked the women about their experiences related to the maternal health care and resources they received, among other topics.
To address the first and fourth questions, we conducted a literature review of studies, peer-reviewed articles from researchers, and articles from national entities published from January 2013 through April 2023. We conducted keyword searches in ProQuest, Dialog Healthcare Databases, Scopus, Ebsco, and PubMed and screened each article for relevance. For any studies, we reviewed the methodologies to ensure that they were sound and determined that they were sufficiently reliable for our purposes. Through this review, we identified 12 articles that included data on pregnant and postpartum women incarcerated in state prisons and local jails. We also identified 33 articles that discussed challenges, recommended standards, or programs related to providing maternal health care to incarcerated pregnant and postpartum women.
To address the first question about available data, we determined the extent of available federal data on pregnant women incarcerated in state prisons and local jails. To collect information from federal entities, we interviewed or received written responses from DOJ and HHS about the extent to which they collect data on this population. Further, we reviewed available reports from BJS that provided relevant data. Additionally, we reviewed datasets from HHS that include data on maternal health and pregnancy outcomes to determine to what extent, if any, we could identify incarcerated women in these datasets.[15]
To address the second question about available federal assistance, we reviewed federal grant information from DOJ and HHS and interviewed officials representing selected state prisons and local jails. As part of our review of grant programs that DOJ and HHS identified as relevant, we reviewed grant solicitations and information about awards used to support maternal health care in state prisons and local jails from fiscal years 2018 through 2023, the most recent data available at the time of our review. In our interviews with officials representing selected prisons and jails, we asked about their awareness of federal assistance to support maternal health care in their facilities and asked them to describe the types of federal assistance that would be useful. We also reviewed the efforts that DOJ and HHS are taking to respond to the blueprint by interviewing and collecting information from knowledgeable DOJ and HHS officials and reviewing the actions and goals for DOJ and HHS described in the blueprint.
Finally, to address the second and fourth questions on available federal assistance and challenges and opportunities to providing maternal health care in state prisons and local jails, we interviewed officials from five nongovernmental organizations.[16] We selected these entities because their work is related to maternal health care for incarcerated women.
For more information on our scope and methodology, see appendix I.
We conducted this performance audit from November 2022 to October 2024 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Operation and Oversight of State Prisons and Local Jails
According to BJS, there were approximately 1,200 state prisons and 3,100 local jails across the U.S. as of 2019.[17] Women resided in approximately 200 public state prisons and accounted for about 8 to 9 percent of the total state prison population.[18] Additionally, as of 2019, women accounted for up to 15 percent of the total local jail population.[19]
Prisons and jails incarcerate different populations. Prisons incarcerate individuals after they are convicted of a criminal offense and typically incarcerate those serving a sentence of more than 1 year. Jails incarcerate individuals before or after court adjudication and typically incarcerate those serving a sentence of 1 year or less. The operation and oversight of prisons and jails also differs. Prisons typically operate under the authority of state departments of corrections (DOCs). Oversight of jails varies by state. State DOCs or other state-level bodies may oversee jails or may have no oversight role.[20] Local jurisdictions, such as a sheriff’s office, usually operate and oversee local jails. A local jurisdiction may oversee multiple local jails. The federal government does not have a role in operating state prisons and local jails.
Trends in the Incarceration of Women in Prisons and Jails
The number of women incarcerated in prisons and jails is increasing, following a temporary period of decline during the COVID-19 pandemic.[21] BJS data indicate the number of women in prisons and jails increased from 2012 through 2019, decreased in 2020 during the pandemic, and has since increased again.[22] Specifically, in 2020, the number of women in state prisons decreased by 25 percent compared to 2019 pre-pandemic levels, while the number of women in local jails decreased by 37 percent. By 2022, the number of women in state prisons and local jails was at about 80 percent of the pre-pandemic levels.[23] See figure 1 for more information.
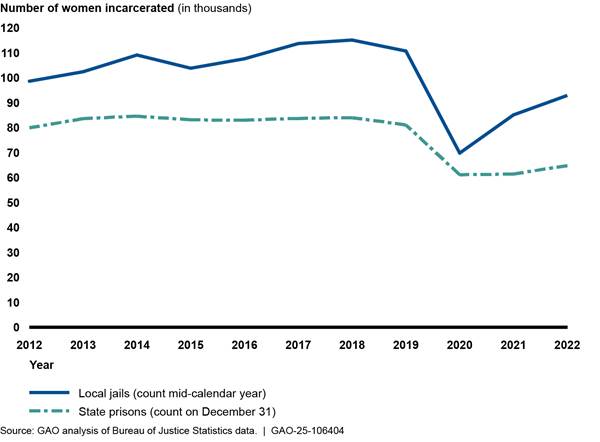
Additionally, BJS data indicate that women of different racial and ethnic groups are incarcerated in U.S. federal and state prisons at different rates. See the text box below for more information about how these rates differ.
|
Incarceration Rates for Women in Federal and State Prisons Varies by Racial and Ethnic Groups According to the Department of Justice’s Bureau of Justice Statistics (BJS) data, women of different racial and ethnic groups are incarcerated in state and federal prisons at different rates. BJS reported the following incarceration rates for women in 2022: •All women: 49 per 100,000 •White women: 40 per 100,000 •Black or African American women: 64 per 100,000 •Hispanic or Latina women: 49 per 100,000 •American Indian/Alaska Native women: 173 per 100,000 •Asian women: 5 per 100,000 •Women of two or more races (not specified): 269 per 100,000 |
Source: BJS data | GAO‑25‑106404
Supreme Court Rulings on Access to Health Care
The U.S. Supreme Court has ruled that incarcerated individuals have a constitutional right to adequate medical and mental health care. In 1976, the U.S. Supreme Court concluded that deliberate indifference to the serious medical needs of prisoners by prison personnel constitutes the unnecessary and wanton infliction of pain prohibited by the Eighth Amendment.[24] Similarly, in 2011, the U.S. Supreme Court held that adequate medical and mental health care must meet minimum constitutional requirements and meet prisoners’ basic health needs.[25] As such, incarcerated pregnant women, including those in state prisons and local jails, have a constitutional right to adequate medical and mental health care to support their pregnancies, deliveries, and postpartum period.
Standards and Guidance for the Care of Pregnant Women
Incarcerated pregnant women have a unique set of health and safety needs, such as access to prenatal care and maternal nutrition. Various professional organizations recommend standards and guidance for the care of pregnant women in correctional settings. These organizations include the American College of Obstetricians and Gynecologists, the American Correctional Association, and the National Commission on Correctional Health Care, among others.[26] Adherence to these standards and guidance is voluntary. Some of these professional organizations offer accreditation to correctional facilities that demonstrate they meet their recommended standards and guidance. However, there is no national requirement that facilities obtain and maintain accreditation. According to BJS officials, some jurisdictions or facilities may be required contractually or statutorily to adhere to accreditation standards and guidelines.
Federal Role
Multiple entities within DOJ and HHS have a role in maternal health care for incarcerated pregnant women:
· DOJ’s BJS collects, analyzes, publishes, and disseminates information on the operation of justice systems at all levels of government, including on state prisons and local jails. BJS also provides financial and technical support to state, local, and tribal governments to improve their statistical capabilities.
· DOJ’s Office of Justice Programs, the largest grantmaking component of DOJ, awards federal assistance through its many grant programs. Some of these grant programs can be used to support maternal health care, which we describe later in this report.
· DOJ’s Bureau of Prisons (BOP) is largely responsible for the custody and care of people incarcerated by the federal government.
· HHS agencies collect data on U.S. pregnancy and maternal health outcomes, including maternal morbidity and mortality. For example, HHS’s Centers for Disease Control and Prevention manages the Pregnancy Risk Assessment Monitoring System which collects data on maternal attitudes and experiences before, during, and shortly after pregnancy. The births in the jurisdictions participating in this effort represent approximately 81 percent of all live births in the U.S.
· HHS’s Health Resources and Services Administration and Administration for Children and Families, among other HHS agencies, also award federal assistance through their many grants programs to state, local, and tribal governments. Some of these grant programs can be used to support maternal health care, which we describe later in this report.
Comprehensive National Data on Incarcerated Pregnant Women Do Not Exist, but DOJ Has a Collection Effort Underway
DOJ and HHS Have Limited Information on the Population of Incarcerated Pregnant Women in State Prisons and Local Jails
DOJ’s BJS does not regularly collect comprehensive data on incarcerated pregnant women in state prisons and local jails—nor are state DOCs and jails typically required to provide data to BJS. In prior years, BJS conducted two separate periodic data collection efforts that provided limited information on pregnant women in prisons and jails. Most recently, BJS published the findings in reports issued in 2021 and 2006, respectively.[27] In 2021, BJS reported that as of 2016 about 4 percent of women in state prisons reported being pregnant at the time of admission. Of these women, 91 percent reported they received an obstetric exam and 50 percent reported they received some other form of prenatal care.[28] In 2006, BJS reported that as of 2002 about 5 percent of women in local jails reported being pregnant at the time of admission. Of these women, 48 percent reported they received an obstetric exam and 35 percent reported they received some other form of prenatal care.[29] Neither of these studies provides demographic characteristics, such as the race and ethnicity, of the incarcerated pregnant women in prisons and jails.[30]
Further, HHS does not collect comprehensive data on incarcerated pregnant women in any type of correctional facility—nor is it required to do so. HHS has five national or near national-level data collection efforts related to maternal health and pregnancy outcomes. These include HHS’s Healthcare Cost and Utilization Project, Pregnancy Risk Assessment Monitoring System, National Vital Statistics System, Pregnancy Mortality Surveillance System, and Maternal Mortality Review Information Application data collection efforts. These efforts, however, do not have systematic indicators to identify incarcerated pregnant women. According to HHS, while these efforts collect granular data on maternal health outcomes and pregnancy outcomes, none of them systematically identify whether the women are incarcerated in state prisons and local jails. For example, the Pregnancy Risk Assessment Monitoring System collects data on maternal attitudes and experiences, before, during, and shortly after pregnancy, but does not collect specific data on whether women were incarcerated in a state prison or local jail during their pregnancies or at the time of delivery.
BJS Has Efforts Underway to Collect More Comprehensive Data
DOJ’s BJS has efforts underway intended to collect more comprehensive data on incarcerated pregnant women through a voluntary survey of state prisons. In fiscal year 2021, Congress directed BJS to amend its ongoing data collection efforts with prisons and jails to include collecting statistics related to the health needs of incarcerated pregnant women in the criminal justice system.[31] This includes statistics on the number of pregnant women in custody, outcomes of pregnancies, the provision of pregnancy care and services, the health status of pregnant women, and any racial and ethnic disparities in maternal health at the federal, state, tribal, and local levels.
In response, BJS first conducted a maternal health feasibility study in 2021 and 2022 to determine the types of data it could collect from prisons and jails.[32] As part of this study, BJS interviewed BOP, 21 state DOCs, and 20 local jails. In its 2024 report about its findings from the feasibility study, BJS acknowledged that there has been little research or data to date on maternal health in carceral settings, and there is a need for better data on women who are pregnant, outcomes of their pregnancies, and postpartum recovery while incarcerated. Additionally, BJS stated that such data are necessary to assess and address the health needs of incarcerated women related to pregnancy and childbirth.
In the 2024 maternal health feasibility study report, BJS stated that it is feasible to collect some maternal health data from state prisons and local jails but noted challenges to this effort. For example, BJS reported that state prisons and local jails participate in surveys on a voluntary basis, so it must work to get support from the state prison systems and local jail facilities from which it wants to collect information. Additionally, BJS reported that prisons and jails face technical and resource challenges that increase the burden of participating in these surveys. For example, BJS said in its report that the most frequently cited technical challenge by facilities was related to the location and format of maternal health data, noting that some electronic files are not easily searchable. As a result, facilities reported to BJS they would need more resources, such as additional staff, to manually review individual files and compile maternal health data in a timely manner. BJS made five recommendations in the report to mitigate the challenges it identified.[33]
Following the feasibility study, BJS officials told us they will conduct a one-time voluntary survey of state DOCs, on behalf of prisons, to collect information on maternal health care and pregnancy outcomes in state prisons as of the end of calendar year 2023.[34] The survey will request the count of women tested for pregnancy at admission, the number of those tests that are positive, and the number of pregnancy outcomes by outcome type, among other things.[35] BJS officials told us that they expect to publish the findings from the survey in 2025.
According to BJS, these data collection efforts will likely face some limitations. For example, BJS does not anticipate being able to report on maternal health outcomes, including maternal mortality and morbidity. BJS does not anticipate being able to report on individual-level outcome data because its feasibility study found that doing so significantly increases the burden for facilities to respond. For example, according to BJS officials, some facilities told them that doing so would require them to obtain permission from these women to disclose their private information. BJS officials noted that BJS will consider engaging in additional work to better understand these limitations and work with facilities on ways to mitigate them.
All Selected Facilities Reported Collecting Information on Incarcerated Pregnant Women, but the Data Are Limited
Officials representing all nine state prisons and nine local jails we spoke with reported collecting some information on incarcerated pregnant women. Representatives from all of these facilities reported maintaining health data in electronic health records, and officials representing five of nine prisons and three of nine jails reported maintaining custody-relevant information in case management systems.[36] Officials from the prisons and jails we met with generally reported that they collect information about pregnant women during the intake process—such as pregnancy status at admission—and medical providers update electronic health records as they provide care—such as documenting an individual’s delivery date and delivery method.
Officials representing all nine of the prisons we met with said they share pregnancy information with their state DOC. However, none of the prisons, jails, and state or local DOCs we spoke with told us they routinely report this information to DOJ or HHS, nor, according to DOJ and HHS officials, are they generally required to do so.[37] Further, officials representing two of the nine prisons and four of the nine jails we met with share some information with professional organizations, such as the National Commission on Correctional Health Care, to obtain or maintain accreditation. As discussed earlier, these accreditation processes are voluntary, and not all facilities report to these entities.
Prison and jail officials we spoke to also reported challenges to collecting, analyzing, and reporting the data on incarcerated pregnant women. These challenges are related to the personal experiences of incarcerated women, privacy issues, and technology limitations. BJS reported similar challenges in its 2024 maternal health feasibility study report.
Officials’ Perspectives of Personal Experiences of Incarcerated Women
According to officials representing three of the nine prisons and four of the nine jails, it can be difficult to collect complete health information about the pregnant women due to some of the personal experiences of this population. For example, some of these women may not have had access to health care prior to incarceration—often due to lack of resources—and therefore may not have community health records that could provide information about a woman’s health history. According to officials representing four of the nine prisons and three of the nine jails, for some pregnant women, the care they receive while incarcerated may be their first encounter with quality health care during their pregnancy. For women who were able to access health care prior to incarceration, officials representing one prison reported that those community health records may be difficult to obtain. Additionally, officials representing two of the nine prisons and three of the nine jails told us that some women may be reluctant to share their health information or may not report accurate information to corrections staff and health care providers at the facilities.
Further, according to officials representing three of the nine jails, women are not typically incarcerated in jails for their entire pregnancies, which makes it difficult to collect information on pregnancy and maternal health outcomes. For example, officials at one jail told us that the average length of stay at their facility is 59 days, while officials at another jail said that the average length of stay at their facility is 193 days. As such, women may be incarcerated at different points of their pregnancies for different lengths of time.
Moreover, officials representing three of the nine prisons reported that when women are transferred from jails to prisons, their health records may not be transferred in a timely manner—or at all. According to officials representing seven of the eight state DOCs we spoke with, they have little to no authority over jail facilities in their state, and officials from one of these DOCs told us they may not receive medical records for women transferring from jails in a timely manner. In addition, local, rather than state, authorities typically operate jails, meaning individual jails may maintain their data differently.
Privacy Issues
The prison and jail officials we spoke with told us they generally collect data related to pregnancy in electronic health records, and these data are generally considered protected health information. For example, officials representing one of the nine prisons told us they must balance the privacy required for sensitive medical information with the need to share information with custody staff. To protect sensitive medical information, medical staff may not share all information about a woman’s pregnancy, such as the diagnosis of a high-risk factor, with custody staff. In addition, BJS reported in its maternal health feasibility study report that officials representing the prisons and jails it interviewed discussed privacy concerns related to the health data they can share.[38]
Technology Limitations
Officials representing two of the nine prisons and four of the nine jails reported that data systems sometimes do not connect to one another, or data cannot be easily extracted for analysis. For example, officials representing one of these prisons and three of these jails reported that hospital data systems may not share data with facility data systems, or facility custody data systems may not share data with facility health record data systems. Additionally, staff from some prisons and jails may have to manually extract data from individual health records to conduct analyses.
Selected Studies from 2013 through 2023 Provide Insights on Characteristics of Incarcerated Pregnant Women in State Prisons and Local Jails
We reviewed relevant literature about incarcerated pregnant women in state prisons and local jails, including 12 studies that provided limited information on this population. These 12 studies provided limited data on this population, including the number and prevalence of pregnancy in studied facilities, demographic characteristics of pregnant women, pregnancy outcomes, and maternal health outcomes. None of the studies described in these articles were nationally representative or generalizable. Table 1 provides information we collected from these articles about incarcerated pregnant and postpartum women in state prisons. For a list of all the articles we reviewed about pregnant women incarcerated in state prisons and local jails, see appendix II.
|
Demographics |
|
In a study of 58 women who gave birth and were participating in a pregnancy and parenting support group while incarcerated at one midwestern women’s state prison, 42 percent (23) were White, 13 percent (seven) were Black or African American, 26 percent (14) were American Indian, 2 percent (one) were Hispanic or Latina, 4 percent (two) were Asian, and 13 percent (seven) identified as having more than one racial-ethnic identity.a |
|
Of the 117 women who gave birth while incarcerated at one Minnesota state prison between 2007 and 2016, 57.7 percent (64) were White, 22.5 percent (25) were African American or Black, 14.4 percent (16) were American Indian or Alaska Native, 4.5 percent (five) were Asian, and 0.9 percent (one) were Native Hawaiian or Other Pacific Islander. Additionally, 93.7 percent (104) were non-Hispanic, and 6.3 percent (seven) were Hispanic or Latina.b |
|
Of the 179 pregnant women with opioid use disorder (OUD) incarcerated in a North Carolina state women’s prison from 2016 to 2018, 62.4 percent (111) of the women in the sample were Non-White, and 37.6 percent (67) were White.c |
|
Prevalence of pregnancy |
|
A total of 1,224 pregnant women were admitted to the 22 state prisons participating in the Pregnancy in Prisons Statistics (PIPS) study during a 12-month study period (2016—2017). Pregnant women represented 3.8 percent of admitted women to participating state prisons in December 2016.d |
|
Pregnancy outcomes |
|
Of the 1,224 pregnant women admitted to state prisons participating in the PIPS study, 742 pregnancies ended during custody. Of these, 92 percent (685) ended in live births, 1.2 percent (nine) in abortions, 6 percent (42) in miscarriages, 0.5 percent (four) in stillbirths, and 0.3 percent (two) in ectopic pregnancies.e Of the 685 live births in these state prisons, 68 percent (464) were vaginal deliveries and 32 percent (221) were Cesarean deliveries. Among live births, 6 percent (39) were preterm and 0.3 percent were very early preterm.f |
|
There were 348 women who gave birth while incarcerated in a subset of 11 state prisons participating in the PIPS study that reported 6 months of lactation frequency data.g |
|
Researchers identified records of 114 births for women incarcerated at a large midwestern state prison from May 2013 to December 2018.h |
|
In a study of 58 women who gave birth and were participating in a pregnancy and parenting support group while incarcerated at one midwestern women’s state prison, women in the sample delivered at 39.3 weeks gestation on average, with a range of 33.1 to 43.1 weeks.i |
|
Of the 117 recorded births of single infants that occurred among women aged 18 and over incarcerated at one Minnesota state prison between 2007 and 2016, 76.9 percent (90) delivered vaginally, and 23.1 percent (27) had Cesarean sections. Medical records indicated that 4.5 percent (five) of infants had a low birthweight, 6.0 percent (seven) of births were preterm, and 6.0 percent (seven) of infants were admitted to the neonatal intensive care unit.j |
|
Maternal health outcomes |
|
Researchers assessed depressive symptoms in 58 women who gave birth while in correctional custody and were participating in a pregnancy and parenting support group at one midwestern women’s state prison and found that 33 percent (19) exhibited minimal depression, 33 percent (19) exhibited mild depression, 21 percent (12) exhibited moderate depression, 10 percent (six) exhibited moderately severe depression, and 3 percent (2) exhibited severe depression. In addition, 9 percent (five) endorsed suicidal or self-injurious ideation at least once.k |
|
Health characteristics |
|
Twenty state prisons participated in a 6-month supplemental reporting period of the PIPS study. Among these prisons, 117 pregnant women with OUD were admitted. This represented 26 percent of the total 445 women admitted to these participating state prisons. Of the 117 pregnant women with OUD, 31 percent (36) underwent detoxification. Of these 36 women, 86 percent (31) underwent detoxification with medication. Of the 117 women, 69 percent (81) received medications for opioid use disorder (MOUD), which were initiated in custody or continued from the community.l |
|
Of the 179 pregnant women with OUD incarcerated in a North Carolina state women’s prison from 2016 to 2018, 16.2 percent (29) reported heroin use and 85.5 percent (153) used other opioids prior to incarceration. Additionally, 29.6 percent (53) of women had received MOUD prior to incarceration.m |
|
In a study of 58 women who gave birth and were participating in a pregnancy and parenting support group while incarcerated at one midwestern women’s state prison, 68 percent (32) had a previous mental health diagnosis.n |
Source: GAO analysis of cited studies. | GAO‑25‑106404
Note: Regarding the demographic information provided in these studies, the percentages do not account for differences in the sizes of the populations by race and ethnicity. Further, the studies may have used different terms and methods for analyzing race and ethnicity demographic data.
aMariann A. Howland et al., “Depressive Symptoms among Pregnant and Postpartum Women in Prison,” Journal of Midwifery & Women’s Health, vol. 66, no. 4 (2021): 494-502.
bRebecca Shlafer et al., “Maternal and Neonatal Outcomes Among Incarcerated Women Who Gave Birth in Custody,” Birth, vol. 48 (2021): 122-131. 58 of the 117 births recorded in this study occurred prior to 2013.
cAndrea K. Knittel et al., “Medications for Opioid Use Disorder in Pregnancy in a State Women’s Prison Facility,” Drug and Alcohol Dependence, vol. 214 (2020): 1-5.
dCamille Kramer et al., “Shackling and Pregnancy Care Policies in US Prisons and Jails,” Maternal and Child Health Journal, vol. 27 (2023): 186-196; Carolyn Sufrin, et al. “Abortion Access for Incarcerated People: Incidence of Abortion and Policies at U.S. Prisons and Jails,” Obstetrics & Gynecology, vol. 138, no. 3 (2021): 330-337; Carolyn Sufrin, et al. “Pregnancy Outcomes in US Prisons, 2016–2017” AJHP Open-Themed Research, vol. 109, no. 5 (2019): 799-805. Researchers associated with the Advocacy and Research on Reproductive Wellness of Incarcerated People research group at the John Hopkins School of Medicine conducted the PIPS study. PIPS includes data on pregnancy outcomes from 26 Department of Justice Bureau of Prisons facilities, 22 state prison systems, and six county jails. Study prisons included 86 percent of all women in Bureau of Prisons facilities and 53 percent of all women in state prisons in 2016. Participating prisons and jails reported aggregate data to researchers on a monthly basis for 1 year (2016 to 2017).
eSufrin et al., “Abortion Access for Incarcerated People: Incidence of Abortion and Policies at U.S. Prisons and Jails.”
fSufrin et al., “Pregnancy Outcomes in US Prisons, 2016-2017.”
gIfeyinwa V. Asiodu, Lauren Beal, and Carolyn Sufrin, “Breastfeeding in Incarcerated Settings in the United States: A National Survey of Frequency and Policies,” Breastfeeding Medicine, vol. 16, no. 9 (2021): 710-716. For 6 months, 11 state prisons completed an optional, supplemental, monthly reporting form for PIPS on the numbers of women who were lactating.
hVirginia E. Pendelton et al., “Caregiving Arrangement and Caregiver Well-being when Infants are Born to Mothers in Prison,” Journal of Child and Family Studies, vol. 31 (2022): 1894-1907.
iHowland et al., “Depressive Symptoms among Pregnant and Postpartum Women in Prison.” The average gestation period is about 40 weeks.
jShlafer et al., “Maternal and Neonatal Outcomes Among Incarcerated Women Who Gave Birth in Custody.”
kHowland et al., “Depressive Symptoms among Pregnant and Postpartum Women in Prison.” Researchers collected data as part of an ongoing evaluation of a prison-based pregnancy and parenting support program at one women’s state prison. At prenatal and postpartum visits with their doula, women completed a patient health questionnaire to measure their depressive symptom severity.
lCarolyn Sufrin et al., “Opioid Use Disorder Incidence and Treatment Among Incarcerated Pregnant People in the U.S.: Results from a National Surveillance Study,” Addiction, vol. 115, no.11 (2020): 2057-2065. For 6 months, 20 prisons completed an optional, supplemental monthly reporting form for PIPS on numbers of pregnant people with OUD admitted and their treatment. The prisons represented 38 percent of women in state prisons.
mKnittel et al., “Medications for Opioid Use Disorder in Pregnancy in a State Women’s Prison Facility.”
nHowland et al., “Depressive Symptoms among Pregnant and Postpartum Women in Prison.”
Additionally, table 2 provides information we collected from these articles about incarcerated pregnant and postpartum women in local jails.
|
Demographics |
|
In a study of 241 pregnant women incarcerated in one of seven jails in a southeastern state between August 1, 2012, and October 1, 2016, 46.5 percent (112) were White, 46.1 percent (111) were Black or African American, and 6.2 percent (15) were of another race. 22.4 percent (54) of the women reported being homeless during the past year.a |
|
Prevalence of pregnancy |
|
A total of 1,622 pregnant women were admitted to local jails participating in the Pregnancy in Prisons Statistics (PIPS) study during a 12-month study period (2016—2017). Pregnant women represented 3.2 percent of admitted women to participating jails in December 2016.b |
|
Pregnancy outcomes |
|
A total of 224 pregnancies in local jails participating in the PIPS study ended during custody. Of these, 64 percent (144) ended in live births, 18 percent (41) in miscarriages, 15 percent (33) in abortions, 1.8 percent (four) in ectopic pregnancies, and 0.9 percent (two) in still births. Of the 144 live births, 32 percent (46) were Cesarean deliveries and 8.3 percent (12) were preterm births.c |
|
There were 77 women who gave birth while incarcerated at a subset of five local jails participating in the PIPS study that reported 6 months of lactation frequency data and supported lactation.d |
|
Maternal health outcomes |
|
At all six participating local jails, there were no maternal deaths in the PIPS study.e |
|
Health characteristics |
|
Fifty pregnant women with opioid use disorder (OUD) were admitted to four local jails participating in optional, 6-month supplemental reporting about OUD for the PIPS study. This represented 14 percent of the total 353 women admitted to these participating local jails. Seventy-three percent (37) of the pregnant women with OUD received medications for opioid use disorder (MOUD).f |
|
In a study of 27 pregnant women incarcerated at a local jail facility in a large midwestern county, 48.2 percent of study participants self-reported a mental health concern. Study participants reported previously receiving mental health treatment for depression (40.7 percent), anxiety (22.2 percent), physical abuse (18.5 percent), schizophrenia (11.1 percent), bipolar disorder (7.4 percent), and trauma (3.7 percent). Additionally, 55.6 percent screened positive for substance use disorder, 44.4 percent received previous alcohol or drug treatment in their lifetime, and 18.5 percent received previous alcohol or drug treatment in the last year. Further, 55.5 percent of study participants reported co-occurring conditions; 25.9 percent of pregnant women screened reported potential challenges with physical health problems, mental health treatment history, and substance use problems.g |
|
In a study of 241 pregnant women incarcerated in one of seven jails in a southeastern state between August 1, 2012, and October 1, 2016, 40.2 percent (97) of the women reported receiving a mood or psychiatric disorder diagnosis. Additionally, 52.7 percent (127) of the women reported illegal drug use in the past 2 years, and 12.4 percent (30) reported methadone use in the past 6 months.h |
Source: GAO analysis of cited studies. | GAO‑25‑106404
Note: Regarding the demographic information provided in these studies, the percentages do not account for differences in the sizes of the populations by race and ethnicity. Further, the studies may have used different terms and methods for analyzing race and ethnicity demographic data.
aCaroline M. Kelsey, Morgan J. Thompson, and Danielle H. Dallaire, “Community-Based Service Requests and Utilization among Pregnant Women Incarcerated in Jail,” Psychological Services, vol. 17, no. 4 (2020): 393-404.
bCamille Kramer et al., “Shackling and Pregnancy Care Policies in US Prisons and Jails,” Maternal and Child Health Journal, vol. 27 (2023): 186-196; Carolyn Sufrin et al., “Abortion Access for Incarcerated People: Incidence of Abortion and Policies at U.S. Prisons and Jails,” Obstetrics & Gynecology, vol. 138, no. 3 (2021): 330-337. Researchers associated with the Advocacy and Research on Reproductive Wellness of Incarcerated People research group at the John Hopkins School of Medicine conducted PIPS study. PIPS includes data on pregnancy outcomes from 26 Department of Justice Bureau of Prisons facilities, 22 state prison systems, and six county jails. Study jails accounted for about five percent of all women in local jails in 2016. Participating prisons and jails reported aggregate data to researchers on a monthly basis for 1 year (2016 to 2017).
cKramer et al., “Shackling and Pregnancy Care Policies in US Prisons and Jails.”; Sufrin, et al., “Abortion Access for Incarcerated People: Incidence of Abortion and Policies at U.S. Prisons and Jails.”; Carolyn Sufrin, et al., “Pregnancy Prevalence and Outcomes in U.S. Jails,” Obstetrics & Gynecology, vol. 135, no. 5 (2020): 1177-1183.
dIfeyinwa V. Asiodu, Lauren Beal, and Carolyn Sufrin, “Breastfeeding in Incarcerated Settings in the United States: A National Survey of Frequency and Policies,” Breastfeeding Medicine, vol. 16, no. 9 (2021): 710-716. For 6 months, five local jails completed an optional, supplemental, monthly reporting form for PIPS on the numbers of women who were lactating.
eSufrin et al., “Pregnancy Prevalence and Outcomes in U.S. Jails.”
fCarolyn Sufrin et al., “Opioid Use Disorder Incidence and Treatment Among Incarcerated Pregnant People in the U.S.: Results from a National Surveillance Study,” Addiction, vol. 115, no. 11 (2020): 2057-2065. For 6 months, four prisons completed an optional, supplemental monthly reporting form for PIPS on numbers of pregnant people with OUD admitted and their treatment. The jails represented 2 percent of women in local jails.
gSusan J. Rose, and Thomas P. LeBel, “Confined to Obscurity: Health Challenges of Pregnant Women in Jail,” Health & Social Work, vol. 45, no. 3 (2020): 177-185. As part of a larger study of incarcerated mothers of minor children, women identified as pregnant were offered screening for substance use problems.
hKelsey, Thompson, and Dallaire, “Community-Based Service Requests and Utilization among Pregnant Women Incarcerated in Jail.”
HHS and DOJ Assistance Can Be Used to Support Maternal Health Care in State Prisons and Local Jails
Five HHS and Ten DOJ Grant Programs Could Be Used to Support Maternal Health Care
Both HHS and DOJ have grant programs that could be used to support maternal health care in state prisons and local jails. HHS has five such grant programs.[39] Officials from HHS’s Administration for Children and Families (ACF) and Health Resources and Services Administration (HRSA) told us that while their grant programs are not specifically designed for providing maternal health care in prisons and jails, award funds for five grant programs could be used for this purpose. For example, HRSA officials told us that recipients could use award funds from the Healthy Start Initiative program to enhance maternal health care in prisons and jails. The purpose of this program is to reduce rates of infant death, improve maternal health outcomes, and reduce racial and ethnic disparities. Appendix III provides more information about these five HHS grant programs.
DOJ’s Office of Justice Programs (OJP) has 10 grant programs that could be used to support maternal health care in state prisons and local jails. OJP officials told us that while these grant programs are not specifically designed for providing maternal health care in prisons and jails, award funds could be used for this purpose. For example, OJP officials told us that recipients could use award funds from the Comprehensive Opioid, Stimulant, and Substance Abuse Site-Based Program to enhance maternal health care in prisons and jails by planning, developing, and implementing comprehensive efforts that identify, respond to, treat, and support individuals impacted by the use and misuse of opioids, among other substances. Appendix III provides more information about these 10 DOJ grant programs.
In addition to available OJP grant programs, officials from OJP’s Bureau of Justice Assistance and BOP’s National Institute of Corrections told us they provide training and information resources online that may be useful to state prisons and local jails.[40] They can also provide technical assistance directly to prisons and jails upon request, such as guidance, assessment, and customized training.
Few State Prisons or Local Jails Received HHS or DOJ Federal Assistance
HHS officials told us some of its grant funds are being used to support maternal health care in state prisons and local jails. According to officials and grant documentation, at least 23 awards under the Healthy Start Initiative, Head Start and Early Head Start, and the Title V Maternal and Child Health Services Block Grant programs were used to support maternal health care in prisons and jails during fiscal years 2018 through 2023.[41] However, none of the 23 HHS grant recipients for fiscal years 2018 through 2023 were state departments of correction or prison or jail facilities. The recipients that used HHS award funds to provide services at these facilities were nongovernmental organizations or other government entities, such as state governments, child development agencies, and county departments of health. Examples of how recipients are using these grant programs are provided in the text box below. Appendix IV provides information about how HHS grant recipients are using all 23 grant awards to support maternal health care in prisons and jails.
|
Examples of Grant Award Funds Used to Support Maternal Health Care in State Prisons and Local Jails One Department of Health and Human Services (HHS) Healthy Start Initiative recipient is using grant funds to provide medical care in a local jail, along with county jail staff. Grant funds help support a portion of a family medicine doctor’s salary and a full-time medical assistant who ensure the jail complies with the recommended prenatal visit schedule. One HHS Early Head Start recipient reported using grant funds to support its prison nursery, where eligible incarcerated mothers reside with their babies until the mother’s release from incarceration, up to 36 months. As part of this program, incarcerated mothers receive targeted learning opportunities to assist in building their parenting skills. |
Source: HHS grant information. | GAO‑25‑106404
DOJ officials were not aware of any of its grant funds being used to support maternal health care in state prisons or local jails during fiscal years 2018 through 2023. Additionally, based on a key word search of DOJ’s grants management systems, we did not identify any grant recipient that utilized funds for maternal health care in state prisons or local jails. Further, as of May 2024, officials from the Bureau of Justice Assistance and the National Institute of Corrections said that they did not receive any requests for technical assistance related to maternal health care for incarcerated pregnant women during fiscal years 2018 through 2023.
In interviews with officials representing selected prisons and jails, we found that they generally were unaware of HHS and DOJ assistance that could be used to support maternal health care in their facilities. For example, officials representing five of the nine prisons and six of the nine jails we met with were unaware of any available federal grants. When asked about what types of federal assistance would be useful, officials from seven prisons and four jails described how they would potentially use financial assistance. Officials representing one prison and one jail said they would construct specialized housing for pregnant and postpartum women. Officials representing four prisons also said they would use funds to develop additional services for postpartum women, such as a nursery or breastfeeding program.
Two of the five grant programs HHS officials told us could be used to support maternal health care in prisons and jails—Healthy Start Initiative and Head Start and Early Head Start—use grant solicitations, also known as notices of funding opportunity.[42] We reviewed a sample of five available HHS grant solicitations, and none mentioned providing maternal health care in state prisons or local jails as an allowable use of funds.[43]
HRSA officials stated that they do not include information about how grant funds can be used to support maternal health care in state prisons and local jails in their grant information because they only include the required elements found in law. This prevents grant applicants from misinterpreting the authorized uses of the grant awards. HRSA grant recipients determine how to use the funds they receive based on state and community needs, and thus may choose to support services in state prisons and local jails. In addition to solicitations, HRSA makes information about its grant programs available on its public website and disseminates newsletters to interested parties, among other things.
Similarly, ACF officials noted that they do not include information about how grant funds can be used to support maternal health care in state prisons and local jails in their grant information because Head Start and Early Head Start programming can be delivered to a range of eligible families in a wide variety of settings. ACF officials also stated that they do not want to prescribe the physical location for the services or the children to be served. ACF officials noted that this allows organizations to design and implement programs that are the most responsive to the unique needs of the communities and populations they serve.
We reviewed available DOJ grant solicitations for the 10 grant programs that DOJ told us could be used to support maternal health care in prisons and jails. We found that from fiscal years 2018 through 2023, DOJ issued 39 solicitations for these 10 grant programs. Only four of the 39 solicitations mentioned that funds could be used to provide services to pregnant women in prisons or jails. This represented three of the 10 relevant grant programs. For example, the 2022 and 2023 solicitations for the Second Chance Act: Improving Substance Use Disorder Treatment and Recovery Outcomes for Adults in Reentry stated that grant funds can be used to provide family-based substance use disorder treatment programming for incarcerated pregnant and postpartum women in prisons.
According to OJP officials, the primary purpose of its 10 grant programs is to enhance substance use and other behavioral health treatments and improve reentry outcomes for people leaving prisons and jails. OJP officials stated that they do not include information about how grant funds can be used to support maternal health care in state prisons and local jails in most of their grant information, such as solicitations for these programs, because grant recipients may only use the funds in that manner if doing so helps them meet the primary purpose of these programs. In addition, it is possible that maternal health care would not be an allowable use of funds for these programs; for example, if the award recipient did not specify it would use award funds to provide maternal health care in its approved award budget.
Further, Bureau of Justice Assistance and National Institute of Corrections officials noted that they market and distribute existing technical assistance and resources on their public websites and in stakeholder listservs. Bureau of Justice Assistance officials told us that both grant recipients and nonrecipients may request technical assistance. They allocate funding to training and technical assistance providers, such as research organizations and consulting agencies, and scope responses to requests to manage available funds. Additionally, National Institute of Corrections officials told us they are not able to broadly announce new technical assistance for maternal health care because they do not have funding available to support responding to requests for new technical assistance. Rather, they review requests to determine trends and patterns related to state and local requests. Occasionally, National Institute of Corrections advertises targeted technical assistance on specific topics in high demand from state and local requests, as allowed by available funding.
In addition to available assistance for providing maternal health care to incarcerated pregnant women in state prisons and local jails, HHS and DOJ have both committed other resources to addressing the maternal health crisis in alignment with the White House blueprint, including for incarcerated women. For example, HHS issued a report to Congress in July 2024 that described its efforts to address the maternal health crisis, including developing a framework to assess its progress.[44] HRSA resources also continue to support the use of doulas, among other actions that could enhance maternal health care for incarcerated pregnant women.
Further, BJS is taking action to learn more about the number and characteristics of incarcerated pregnant women in prisons and jails. In its maternal health feasibility study report, BJS noted that collecting data on incarcerated pregnant women and learning more about the health services and accommodations provided is necessary to assess and address the health needs of incarcerated women related to pregnancy and childbirth.
Selected Prisons and Jails Reported Providing Care for Incarcerated Pregnant Women that Aligned with Guidance, State Laws, and Policies
Selected Prisons and Jails Reported Following Recommended Guidance to Provide Care for Incarcerated Pregnant Women
Officials representing eight of the nine prisons and eight of the nine jails we met with reported following guidance from one or more professional organizations on providing maternal health care to incarcerated women.[45] These organizations include the American College of Obstetricians and Gynecologists (ACOG), the American Correctional Association, and the National Commission on Correctional Health Care.
We also asked officials representing the nine prisons and nine jails we met with about the services and types of care that they provide for pregnant and postpartum women in their facilities, regardless of whether they reported following guidance from one or more professional organizations.[46] For example, we asked about pregnancy testing, postpartum care, and substance use disorder care. Figure 2 shows how many prisons and jails reported providing each service or type of care. See appendix V for additional information about the services that state prisons and local jails reported providing.
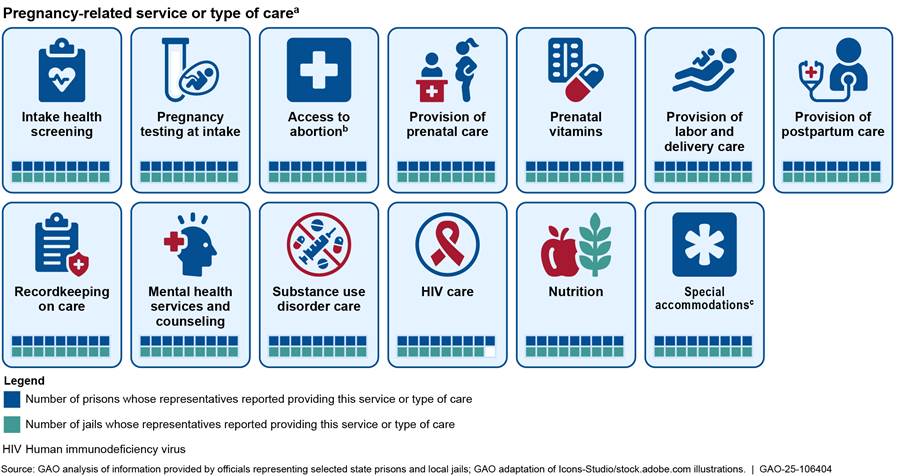
Note: We spoke with officials representing nine prisons and nine jails in a nongeneralizable sample of states to discuss maternal health care in their facilities. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as racial and ethnic data available for the population under the jurisdiction of state or federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities, among other factors. Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
aWe identified the type of service or care the nine prisons and nine jails we spoke with reported providing based on information obtained during interviews with officials representing these facilities or documentation from these facilities. If a facility is excluded from the count of prisons or jails providing a type of service or care, this does not necessarily mean that the facility does not provide that type of service or care. Instead, it may mean that officials did not mention that type of service or care to us, even though the facility they represent provides it. Additionally, we did not independently verify the availability or provision of services and types of care that officials or facility documentation identified as available.
bAccess to abortion services is based on what officials reported to us, which may mean that the facility provides access to abortion within the context of any applicable state laws. Officials made these statements as of the dates of our interviews, and state laws and facility policies may have changed following our interviews.
cSpecial accommodations may include housing (such as lower bunk assignments), adjusted work, activity, or programming assignments, and special clothing.
Although state prisons and local jails are not required to follow guidance from professional organizations, several of the services and types of care that officials described providing aligned with standards from ACOG’s 2021 committee opinion on reproductive health care for incarcerated pregnant, postpartum, and nonpregnant individuals.[47] For example, ACOG recommends assessing all women of child-bearing age for pregnancy, including by offering pregnancy testing, and officials representing all nine prisons and nine jails we met with reported providing pregnancy testing. Additionally, ACOG recommends the provision of medications for opioid use disorder for pregnant women with opioid use disorder.[48] Officials representing seven of nine prisons and eight of nine jails reported that medications for opioid use disorder are available for pregnant women, and officials representing one other prison told us that they are starting a program to provide this treatment.
Officials representing the nine prisons and nine jails we met with reported providing some services and types of care in different ways. For example, the nutrition that pregnant women receive varied across facilities. Officials representing six of nine prisons and eight of nine jails reported providing supplemental calories or a pregnancy diet for pregnant women. Officials representing one of the other three prisons reported that a clinical dietician and medical providers assess each pregnant woman and jointly decide on appropriate nutrition. Additionally, officials representing another prison told us that all women at the facility receive additional calories because they receive the same portions as incarcerated men in the state, and a doctor can determine that a pregnant woman requires a different diet.[49] Finally, officials representing one jail reported that a nutritionist at the facility can request special diets for pregnant women.
Additionally, who provided maternal health care to pregnant and postpartum women varied across selected facilities. For example, officials representing six of nine prisons and five of nine jails reported that they provide care through a partnership with a hospital, health system, or government entity. Additionally, officials representing three of nine prisons and three of nine jails told us that they contract with a private company to provide medical care.[50]
Many of the pregnant and postpartum women we met with reported receiving several of the services outlined above.[51] For example, 18 of 19 women we met with in prisons and all eight women we met with in jails reported receiving prenatal vitamins and being assigned a lower bunk. Additionally, 18 of 19 women we met with in prisons and six of eight women we met with in jails told us that they received supplemental food. For more information about the personal experiences of pregnant and postpartum women in the prisons and jails we visited, see appendix VI.
Selected Prisons and Jails Reported Following Applicable State Laws and Policies
Officials representing eight of nine prisons and six of nine jails reported that they are subject to state laws requiring particular care for and treatment of incarcerated pregnant and postpartum women.[52] These laws cover topics such as the use of restraints, restrictive housing, and other topics related to the treatment of pregnant and postpartum women.
Restraints. Officials representing all nine prisons and nine jails told us that they prohibit or limit the use of restraints for pregnant and postpartum women based either on state law or policy, including policy from the facility, state or local DOC, or sheriff’s office.[53] While officials representing all prisons and jails reported that their facilities followed laws or policies prohibiting or limiting the use of restraints, variations in these laws and policies existed across states and facilities.
Officials representing five of nine prisons and six of nine jails reported that state law or policy restricts, not prohibits, the use of restraints on pregnant women. For example, officials representing two prisons and two jails told us that staff may use restraints on pregnant women in certain situations, including for safety, such as when a pregnant woman presents a serious risk of harm to herself and others. Officials representing two prisons and three jails indicated that in cases when staff restrain a pregnant woman, they must document the use of restraints, such as by reporting to an external oversight body. For example, officials representing one of these three jails explained that if custody staff use restraints on a pregnant woman, they must report this use to a statewide oversight body.
Officials representing six of nine prisons and five of nine jails reported that custody staff receive training or information about using restraints on pregnant and postpartum women. For example, officials representing one prison told us that the same state law that, among other things, limits the use of restraints on pregnant women also requires the state department of corrections to train staff on the law’s provisions. In addition, officials representing one of nine jails that we met with reported that they provide all pregnant women with laminated cards. In addition to other information, the cards include a list of their rights during pregnancy, labor and delivery, and recovery after delivery, including limitations on the use of restraints.
Restrictive housing. Officials representing three of nine prisons also told us that state law either prohibits or limits the use of restrictive housing for pregnant, and in one state, postpartum, women. For example, officials representing one of these prisons told us that placing pregnant women in restrictive housing requires approval from state department of corrections officials.
Other facilities reported policies that limit the placement of pregnant women in restrictive housing or that add precautions to placing pregnant women in this setting. Officials representing two of nine prisons reported that based on policy, they do not or generally do not place pregnant women in restrictive housing. Officials representing one of these facilities explained that staff may only place pregnant or postpartum women in restrictive housing if doctors determine that the woman has specific medical or mental health needs and would benefit from the placement. Additionally, officials representing one of nine jails reported that staff may not place a pregnant woman in restrictive housing, and officials representing two other jails reported that staff generally do not place pregnant women in restrictive housing. Further, officials representing four of nine jails told us that staff may place pregnant women in restrictive housing under certain circumstances. Officials representing three of these jails told us that medical staff must clear women for placement in restrictive housing.
Other topics related to the treatment of pregnant and postpartum women. Officials representing two prisons and two jails identified other state laws affecting the treatment of pregnant and postpartum women in their facilities. According to officials representing two prisons, state laws require 72 hours of bonding time for incarcerated women and their infants following delivery. Officials from one jail also reported that state law entitles incarcerated women to a support person during delivery.[54] Additionally, officials from another jail reported that state law requires the jail provide education on prenatal topics for pregnant women.
Selected Prisons and Jails Reported Providing Additional Programs and Resources to Support Maternal Health Care
In addition to the care and services that professional organizations recommend or that are required by state laws, officials representing several of the nine prisons and nine jails also reported other programs and resources that support maternal health care at these facilities. These programs include pregnancy or parenting classes, doula programs, nursery programs, and lactation programs.
Pregnancy or parenting classes. Officials representing five of nine prisons and three of nine jails reported that their facilities offer classes on pregnancy or parenting. For example, officials representing one jail told us about an adapted version of the CenteringPregnancy program that medical staff and staff from the facility’s doula program provide for pregnant women at the facility.[55] During CenteringPregnancy sessions, medical providers facilitate discussions and lead activities for pregnant and postpartum women related to topics including nutrition, stress management, labor and delivery, and infant care. Additionally, officials representing one prison described the facility’s pregnancy and parenting programs, which incarcerated women lead for their peers. These classes cover topics that include having a healthy pregnancy, managing successful family visits, and improving communication skills with their children.
Doula programs. Officials representing one of nine prisons and four of nine jails reported that they provide incarcerated women the option of working with a doula. Five of the six pregnant and postpartum women we met with at a facility with a doula program reported working with a doula. Three of these five women assessed their experiences, and all three told us that they found the program helpful and appreciated the support they received from their doulas. Including those facilities with a doula program, officials representing six of nine prisons and five of nine jails reported that women may have a support person present during delivery.[56] Officials representing two of these prisons and two of these jails reported that the support person must receive authorization to act in this capacity, such as by undergoing a security review.
Nursery programs. Officials representing three of nine prisons and one of nine jails told us that their facilities operate nursery programs where eligible women can reside with their babies following delivery.[57] According to officials representing the three prisons and one jail with nursery programs, participants have access to several types of programming, which may include parenting and child development classes, educational opportunities, substance use disorder treatment, and life skills, such as anger management. Additionally, officials from the three prisons that operate nursery programs reported that program participants enroll in Special Supplemental Nutrition Program for Women, Infants, and Children to receive financial assistance for groceries as part of the program.
According to officials representing all four facilities with nursery programs, participants have access to reentry services.[58] Some of these services are specific to those participating in the nursery program. For example, officials from one facility reported that participants receive equipment, such as car seats to take home with them upon release from the facility. Additionally, officials from another program reported that participants can also receive services following their release, including home visits and referrals to community support.
Lactation programs. Some facilities offer programs that allow postpartum women to continue lactation following separation from their babies, when a nursery program is not available at a facility or a woman is not eligible to participate. Officials representing two of nine prisons and three of nine jails reported that postpartum women can express milk for pick-up and delivery to their infants. Additionally, officials representing one prison and three jails told us that they allow postpartum women to express milk but did not state whether they allow pick-up. Further, officials representing one prison and one jail told us that some postpartum women, such as those releasing within 6 months or those whose doctors request it, are permitted to express milk while others are not. Finally, officials representing two prisons and one jail told us that they are in the process of developing a program that would allow postpartum women to express milk for delivery to their infants.
Challenges and Opportunities Exist for Providing Maternal Health Care in State Prisons and Local Jails
Reported Challenges Include Personal Experiences of the Incarcerated Population, Inconsistent Services, and Other Logistical Issues
Officials representing several of the nine prisons and nine jails we met with, as well as officials from some of the five nongovernmental organizations (NGO) we met with, identified various challenges to providing maternal health care to incarcerated women.[59] We also reviewed 33 articles that described such challenges and opportunities to address them.[60] The challenges that these officials and articles frequently cited included those related to the personal experiences of incarcerated pregnant women, inconsistent access to services across facilities, and logistical challenges.
Identified Challenges Related to Personal Experiences of Incarcerated Pregnant Women
Officials representing several prisons and jails, as well as articles we reviewed, identified various challenges related to the personal experiences of incarcerated pregnant women. These challenges included stress and anxiety, the prevalence of other health conditions among this population, and differences in the care that these women received prior to entering the facility.
Stress and anxiety. Officials representing four of nine prisons and three of nine jails told us that stress from the correctional environment, isolation from loved ones, or pending separation from their infants can cause increased anxiety or frustration or complicate the provision of maternal health care for pregnant women. For example, officials representing one prison reported that women may seek to postpone upcoming inductions if they have not finalized placements for their infants. Nine of the 33 articles we reviewed also described the stress that pregnant women may experience while incarcerated, and six of these articles explained how this stress can negatively impact the health of these women or their infants.
Other health conditions. Officials representing four of nine prisons and four of nine jails reported that pregnant women in their facilities often have other health conditions, such as mental health concerns or substance use disorder, that can complicate their pregnancies and how facilities provide maternal health care. For example, officials representing one prison told us that almost every woman in their care has experienced trauma, which may result in hesitancy to accept care at the facility. Eighteen of the 33 articles we reviewed on challenges and opportunities related to providing care to incarcerated pregnant women also indicated that many of these women have high rates of other health conditions. Nine of these articles noted that incarcerated pregnant women have often experienced trauma, and six of these articles connect this trauma to pregnancy complications, poor health generally, or unique medical needs for these women.
Differences in care prior to entering the facility. Officials representing four of nine prisons reported that by the time pregnant women enter their facilities and staff begin to provide care for them, they have received different quality and types of maternal health care in previous facilities or in their communities. Officials representing three of these prisons explained that pregnant women at their facilities may not have received any care prior to their arrival, and officials representing one of these prisons stated that this delay may result in more progressed medical complications by the time the women receive care. Additionally, six of the 33 articles we reviewed described how pregnant women arriving at a prison or jail may have had limited access to health care prior to incarceration.
Inconsistent Access to Services
Other challenges identified by officials we met with and articles we reviewed include the inconsistent access incarcerated pregnant women have to services across facilities. Access to maternal health care may vary due to differences in the availability of care across facilities, copayments that require pregnant women to pay for at least some of the medical services they receive, or staff discretion when determining what services pregnant women may receive.
Differences in care availability across facilities. The types of maternal health care incarcerated pregnant women can access varies across facilities. Officials representing four of nine prisons and three of nine jails reported that it can be challenging to provide certain types of care for the pregnant population, such as appointments with specialists or adequate health care staff on-site at the facility. For example, officials representing one prison indicated that at the time of our meeting, the facility was transporting pregnant women to a local hospital for care because they could not find an obstetrician-gynecologist to replace the previous obstetrician-gynecologist, who spent 2 days per week at the facility. Additionally, officials representing one prison told us that pregnant women receive more medical screenings if they are incarcerated in a larger, urban jail in the state as opposed to a smaller, rural jail. Also, officials representing two of nine jails told us that their facilities cannot adequately address all mental health challenges that pregnant individuals experience because they do not have appropriate programs in place to do so.
Staff from two of the five NGOs we spoke with provided similar observations about the variability of care, noting that the availability of an on-site medical provider varies across facilities. In addition, smaller jails may not have an appropriate specialist for pregnant women or even any health care staff on-site.
Fifteen of the 33 articles we reviewed on challenges and opportunities for providing care to incarcerated pregnant women mentioned a lack of mandatory national standards for maternal health care in prisons or jails, and nine of these articles connected the lack of standards to variability in the care provided across facilities. For example, one article notes the lack of required health care services at prisons and jails. The article also acknowledges that facility accreditation is optional, and reports that existing research has shown a lack of consistent, comprehensive maternal health care in these facilities that often departs from national recommendations.[61]
Copayments. Although incarcerated individuals have a constitutional right to adequate medical and mental health care, this does not prohibit facilities from charging copayments for care.[62] Three of the 33 articles we reviewed indicated that facilities charging a copayment for maternal health care may present a barrier for incarcerated pregnant women, with one article noting that this population may have limited financial means to cover the cost.[63] Staff from two NGOs we spoke with agreed, stating that incarcerated individuals often cannot afford a copayment and may not pursue care if one exists.
Staff discretion. Seven of the 33 articles we reviewed reported that custody or medical staff discretion may influence the amount or quality of maternal health care that incarcerated pregnant women receive. For example, one article described how custody staff may act as gatekeepers to care because they assess a woman’s labor symptoms and determine when to contact medical personnel.[64] Another article, a nongeneralizable study of pregnant and postpartum women at a single state prison, reported that custody staff played a role as gatekeepers to care.[65] According to this study, while pregnant women at this facility received care at regular prenatal appointments, custody staff decided whether medical concerns women experienced in between appointments warranted a visit to the infirmary.
Other articles identified how judgment from others, including custody and medical staff, or stigma against the incarcerated pregnant population may affect a woman’s access to maternal health care or willingness to pursue this care. Two nongeneralizable studies suggested that stigma against incarcerated pregnant women by custody or medical staff may have affected the care women in selected facilities received.[66] One study, which derived nongeneralizable results from interviews with opioid treatment providers, reported that these providers shared observations of jail staff exhibiting discriminatory attitudes toward incarcerated pregnant women with opioid use disorder. The other study, which derived nongeneralizable results from a survey of perinatal nurses with experience caring for incarcerated women, found that while study participants had strong overall intentions to provide care to this population, stigmatizing attitudes remained significant.[67]
Staff from two of the NGOs we spoke with also stated that some custody staff may hesitate to provide incarcerated pregnant women with particular services or programs because they do not want to provide privileges to this population. Eight of the 27 incarcerated pregnant and postpartum women we met with reported they felt they could not access adequate maternal health care or that custody staff or medical providers did not treat them properly. For example, four of these women reported they felt medical staff rushed the care they provided or did not adequately address their health concerns. Additionally, officials from two of the five NGOs we spoke with indicated that incarcerated pregnant women may not seek care because they experience trauma due to the stigma of their incarceration when they receive health care at a community site.
Logistical Challenges
Officials we met with and articles we reviewed also identified logistical challenges to providing maternal health care to incarcerated pregnant women. These include complications with transportation and staffing and environmental disadvantages.
Transportation and staffing complications. Officials representing three of nine prisons reported that they experience challenges with coordinating transportation and staffing for appointments that occur outside of their facilities. Additionally, officials representing one jail reported that transporting individuals to specialty appointments or the hospital may result in staffing shortages at the facility. Two of the 33 articles we reviewed on challenges and opportunities related to providing care to incarcerated pregnant women noted that transportation challenges can delay or impede women’s access to maternal health care.
Environmental disadvantages. Seven of the 33 articles we reviewed indicated that the prison or jail environment and its constraints may limit the quality of maternal health care that women receive or negatively affect their health outcomes. For example, one of these articles described how the stress, inadequate nutrition and exercise, and violence associated with the prison or jail environment can affect health outcomes for pregnant women.[68] Another article noted that in a system traditionally designed for men, incarcerated pregnant women may not have access to the care they need, especially when these women cannot control factors important for their health, such as sleeping times or diet.[69]
Officials representing three prisons reported that the facility environment may present challenges to providing proper care for pregnant women. For example, officials representing one of these prisons reported that all women in that facility, including pregnant women, reside in a former juvenile facility that was not designed to support women’s needs. Additionally, officials representing two of nine prisons and five of nine jails reported challenges to ensuring continuity of care for women when they leave the facility. For example, officials representing two of these jails told us that medical staff may find it difficult to coordinate long-term care plans for incarcerated pregnant women because the length of time these women will spend in their facilities may not be known.
Reported Opportunities Exist for Prisons and Jails to Further Serve Incarcerated Pregnant Women
Several of the articles we reviewed identified opportunities for prisons and jails to further provide maternal health care for incarcerated pregnant women. Officials representing seven of nine prisons and five of nine jails expressed that providing medical care to pregnant women can generate positive outcomes, such as engaging women in care who may not have had access to it previously and providing quality care or facilitating healthy outcomes for these women and their infants. Officials we interviewed from NGOs and articles we reviewed reported further opportunities to provide this quality care, including by adopting standards for maternal health care across facilities, expanding program offerings, and adjusting institutional policies or operations to provide additional care services.
Adopting Standardized Maternal Health Care Across Facilities
Twelve of the 33 articles we reviewed on challenges and opportunities related to providing care to incarcerated pregnant women recommended prisons and jails adopt standardized maternal health care practices, such as those that professional organizations have developed.[70] Other articles that we reviewed recommended specific care standards that each facility should meet. For example, six articles recommended comprehensive pregnancy testing, such as that all women of child-bearing age receive a pregnancy test at admission, and five articles identified the importance of providing pregnant women with proper nutrition. Additionally, officials from one of the five NGOs we spoke with recommended that facilities have standardized plans for access to prenatal care and other services for pregnant women.
Expanding Program Offerings
The officials we met with from NGOs and the articles we reviewed recommended expanding program offerings to assist pregnant and postpartum mothers, including those that provide medications for opioid use disorder, mental health treatment, opportunities for breastfeeding or lactation, opportunities for mother-infant bonding, and doula services.
Medications for opioid use disorder. Nine of the 33 articles recommended providing access to medications for opioid use disorder for pregnant incarcerated women who need them. Six of these articles reported that medications for opioid use disorder are an evidence-based treatment or the ideal treatment option for pregnant women with opioid use disorder.
Mental health treatment. Seven of the 33 articles recommended providing mental health care for pregnant or postpartum populations. This recommended care includes screening for mental illness and postpartum depression, providing care to address mental health challenges and postpartum depression, and addressing trauma.
Breastfeeding or lactation programs. Ten of the 33 articles discussed developing or enhancing breastfeeding or lactation programs for incarcerated postpartum individuals. These recommendations included facilities making these programs available to their postpartum populations and providing pregnant and postpartum women with education on breastfeeding to assist them in making informed health choices.
Mother-infant bonding opportunities. Nine of the 33 articles advocated for enhancing mother and infant bonding. For example, four of these articles suggested that facilities establish nursery programs. Three of these articles recommended taking steps to facilitate mother-infant visitation, such as incarcerating women near their families, expediting visitation applications, and creating child-friendly visitation environments.
Doula programs. Eight of the 33 articles recommended that staff consider implementing a doula program or suggested that such a program may benefit incarcerated pregnant women. For example, one of these articles interviewed a nongeneralizable sample of women at one state prison and found that many of these women reported feeling dehumanized by the behavior of custody officers monitoring them during delivery.[71] The authors suggested that working with a doula could alleviate some of these feelings for these women.
Adjusting Institutional Policies or Operations
Some of the articles we reviewed and officials from the NGOs we met with recommended adjusting institutional policies and operations that could potentially affect maternal health outcomes, including limiting the use of restraints, eliminating copayments, promoting continuity of care, and enhancing data collection.
Limit the use of restraints. Nine of the 33 articles on the challenges and opportunities related to providing care to incarcerated pregnant women advocated for limiting or enforcing limitations on the use of restraints during pregnancy and, in some cases, during the postpartum period.[72] Five of the articles allowed for certain exceptions to these limitations, such as when a woman presents an imminent risk of harm to herself or others or of escape. Six of the articles described the importance of reporting or documenting any use of restraints, and, in some cases, reporting this use for an independent review. Five of the articles recommended training and educating custody or medical staff to make them aware of the risks of restraint use, the legal limitations on the use of restraints, or the correct application and removal of restraints.
Eliminate copayments. Two of the 33 articles recommended eliminating copayments for health care services during incarceration. Staff from two of the five NGOs we spoke with also suggested eliminating copayments.
Promote continuity of care. Seven of the 33 articles commented on the importance of establishing continuity of care for pregnant and postpartum women upon community reentry. For example, four of these articles referenced the importance of facilitating the continuation of substance use disorder treatment, such as medications for opioid use disorder, upon reentry.
Enhance data collection. Four of the 33 articles advocated for enhancing data collection on pregnancy in prisons and jails. One of these articles explained that additional data on this population could provide insight into gaps in maternal health care or how to address challenges to achieving optimal health outcomes for pregnant women at these facilities.[73] Additionally, officials from one of the five NGOs reported that collecting additional data on the pregnant population, including demographic information and pregnancy and maternal health outcomes, could provide insight into regional or racial differences in outcomes for this population.
Agency Comments
We provided a draft of this report to DOJ and HHS for review and comment. They provided technical comments, which we incorporated as appropriate.
We are sending copies of this report to the appropriate congressional committees, the Attorney General, the Secretary of Health and Human Services, and other interested parties. In addition, the report is available at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions about this report, please contact me at (202) 512-8777 or GoodwinG@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix VII.

Gretta L. Goodwin
Director, Homeland Security & Justice
List of Requesters
The Honorable Jon Ossoff
Chair
Subcommittee on Human Rights and the Law
Committee on the Judiciary
United States Senate
The Honorable Jamie Raskin
Ranking Member
Committee on Oversight and Accountability
House of Representatives
The Honorable Alma S. Adams, Ph.D.
House of Representatives
The Honorable Shontel Brown
House of Representatives
The Honorable Cori Bush
House of Representatives
The Honorable Jasmine Crockett
House of Representatives
The Honorable Robin L. Kelly
House of Representatives
The Honorable Summer Lee
House of Representatives
The Honorable Gwen Moore
House of Representatives
The Honorable Ayanna Pressley
House of Representatives
The Honorable Lauren Underwood
House of Representatives
This report addresses the following questions:
1. What data are available on the characteristics of incarcerated pregnant women and pregnancy outcomes in state prisons and local jails?[74]
2. What federal assistance can be used to support maternal health care in state prisons and local jails?
3. How do selected state prisons and local jails provide maternal health care for incarcerated pregnant women?
4. What are the identified and reported challenges and opportunities to providing maternal health care to incarcerated pregnant women?
State Sample Selection
To address all four questions, we obtained information from officials representing nine state prisons and nine local jails. These nine prisons and nine jails were located across a nongeneralizable sample of 12 states: Alabama, Arizona, California, Georgia, Illinois, Louisiana, New Jersey, New York, North Carolina, Ohio, Tennessee, and Texas. We report perspectives from officials representing state prisons and local jails in the aggregate, due to the sensitivity of some of the information we received about pregnant women and maternal health care at these facilities.
We selected this nongeneralizable sample of states based on several factors. These factors included the state’s female incarceration rate, the number of women under the jurisdiction of state correctional authorities in each state, and the number of women incarcerated in local jails in each state.[75] We used this information to identify states with a range of female incarceration rates that generally had higher numbers of women under the jurisdiction of state correctional authorities or incarcerated in jails because these states may have recent experience caring for incarcerated pregnant women.[76]
To address our first and second questions on available data on incarcerated pregnant women and federal assistance available for supporting their care, we also considered whether we were able to identify any available data on this population or any instances of federal funding serving this population for each state. We also considered the availability of nursery or doula programs in prisons or jails in the state as ways that these facilities provide maternal health care for pregnant and postpartum women, in response to our third question on how facilities provide this care.[77] Additionally, we considered each state’s maternal mortality rate to identify states with a range of rates and considered whether the state has a law in place that restricts the use of restraints on incarcerated pregnant women.[78] We also considered racial and ethnic data available for the population under the jurisdiction of state or federal correctional authorities to identify states that housed higher levels of different racial and ethnic groups because these states may have recent experience caring for incarcerated pregnant and postpartum women belonging to different racial and ethnic groups.[79] Finally, we considered the Census region of each state for geographic diversity.[80] We used these criteria to select an initial sample of 10 states, as well as eight alternate states.[81] We identified alternative states to contact if we did not receive a response from any of the 10 states in our initial sample.
After identifying our nongeneralizable sample of states and alternate states, we identified one prison and one jail in each of our sample states to interview officials regarding maternal health care in their facilities. We generally identified prisons through contacting state department of corrections (DOC) officials, who indicated which prison in their state we should meet with about maternal health care for incarcerated pregnant women. We generally identified jails by selecting jails in large metropolitan areas within the states in our sample. We contacted state and local officials via email and by phone. If we did not receive a meaningful response after at least three attempts to make contact, we selected a state from our list of alternates to begin outreach. In some states, we met with officials representing a prison and officials representing a jail. In other states, we met with officials representing either a prison or a jail.
We received information from officials involved in providing maternal health care to the women incarcerated in nine prisons and nine jails within 12 states. The information these officials provided was reported to us during interviews, in written responses, or in relevant documentation. These officials included medical or custody staff at state DOCs, prisons, sheriff’s departments, local DOCs, and jails. Some of these meetings included other staff members, such as facility social workers and a state DOC research manager. We also met with representatives from one community group and one local government program who provide doula services at two facilities. Because the officials we met with all provided information on maternal health care in their prisons or jails but have different roles or work for different entities, we refer to these officials as “officials representing prisons” or “officials representing jails.”
We conducted site visits to three of the states in our sample. To select these three states, we considered female incarceration rates, choosing one state with a relatively high female incarceration rate, one with a mid-level rate, and one with a low rate.[82] Because we planned to speak with incarcerated pregnant and postpartum women during these site visits, we selected states that had relatively higher numbers of women under the jurisdiction of state correctional authorities and incarcerated in local jails.[83] Additionally, we sought to include states that used federal funding to support programs for incarcerated pregnant women so we could observe these programs and speak to participants during our site visits. We also considered geographic diversity in selecting these three states. Based on these criteria, we selected California, Ohio, and Texas.
We conducted these site visits from June to November 2023. During these site visits, we visited facilities that incarcerate pregnant and postpartum women and spoke with officials who participate in providing maternal health care for these women, discussing the same topics from the semi-structured interviews we held with other officials in states where we did not conduct site visits.[84] We also observed different areas of the facilities we visited, including where pregnant and postpartum women receive some types of maternal health care or participate in nursery programs. Additionally, during our site visits, we conducted semi-structured interviews with a total of 27 incarcerated pregnant and postpartum women at two prisons and two jails across three states. Eight of these women were participating in facility nursery programs at the time we interviewed them. We asked officials from the facilities to identify women who were pregnant or, at most, 3 months postpartum at the time of our visits and to ask for volunteers to participate.[85] We also asked, if possible, to meet with women that reflect the facility’s racial and ethnic diversity. During these interviews, we asked the women about their experiences with receiving maternal health care while incarcerated.
Literature Review
To address our first and fourth questions on available data on incarcerated pregnant women and the challenges and opportunities for providing care to this population, we conducted a literature review. Through this review, we identified articles that included data on pregnant and postpartum women incarcerated in state prisons and local jails, such as the number of pregnant women and prevalence of pregnancy in studied facilities, demographic characteristics of pregnant women, and data on pregnancy outcomes and maternal health outcomes. We also identified articles that discussed challenges, recommended standards, or programs related to providing maternal health care to incarcerated pregnant and postpartum women. To identify these articles, we conducted a search of articles published from January 2013 through April 2023 to capture the most recently available articles at the time our search was conducted. We performed searches in ProQuest, Dialog Healthcare Databases, Scopus, Ebsco, and PubMed. We conducted distinct key word searches for data on the number of incarcerated pregnant women in state prisons and local jails, as well as characteristics of the women, such as race and ethnicity. We also conducted keyword searches on mental health, substance use disorder, and pregnancy and maternal health outcomes.
We conducted a two-stage screening of 204 articles identified via the search. First, two team members independently screened each title and abstract for relevance to the objective question about available data and, in a separate screen, for relevance to the objective question about challenges and opportunities for providing maternal health care. For the articles related to data availability, we excluded review articles that cited research but did not perform original research.
We determined that articles were relevant to the objective question about data availability if they were U.S.-based studies that included data on one or more of the following:
· The number or prevalence of pregnant women in state prisons or local jails;
· Demographic characteristics of incarcerated pregnant women, including race and ethnicity, as well as health characteristics such as mental health and substance use disorder among pregnant women in these facilities;
· Pregnancy outcomes; and
· Maternal health outcomes, including any disparities in these outcomes by race or ethnicity.
We determined that articles were relevant to our objective about challenges and opportunities for providing maternal health care for incarcerated pregnant women if they were studies, peer-reviewed articles from researchers, or articles from national entities that addressed one or more of the following:
· Challenges to providing maternal health care or achieving positive maternal health outcomes for incarcerated women;
· Recommended standards for maternal health care for incarcerated pregnant women; and
· Programs in state prisons or local jails that provide maternal health care.[86]
After completing independent screening, we reconciled any differences in screening decisions, resulting in a list of 60 articles related to available data and a list of 78 articles related to challenges, recommended standards, and programs for providing maternal health care.
Second, we independently screened the full text of each article from both lists to determine if they were still relevant based on the criteria stated above. After completing independent screenings, the team members reconciled any differences in their screening decisions based on each article’s methodology, strengths and limitations, and relevance. For any studies, we reviewed the methodologies to ensure that they were sound and determined that they were sufficiently reliable for our purposes. This screening process resulted in a finalized list of 12 articles related to available data and a list of 33 articles providing information on challenges and opportunities related to providing maternal health care. We reviewed each article in the finalized lists and systematically extracted relevant information for analysis and synthesis.
Select Nongovernmental Organizations
To address our second and fourth questions on federal assistance to support care for the incarcerated pregnant population and the challenges and opportunities for providing this care, we interviewed officials from five nongovernmental organizations (NGO). We selected these entities because their work is related to maternal health care for incarcerated women. For example, one of these NGOs provides services for pregnant women in two state prisons, and others have issued publications related to maternal health care in carceral settings. Table 3 provides a list of these five NGOs and a brief description of the work they do that is relevant to our objective questions.
|
Nongovernmental organization |
Description of relevant work |
|
American College of Obstetricians and Gynecologists (ACOG) |
ACOG is a professional membership organization for obstetrician-gynecologists. Among other functions, ACOG issues practice guidelines for health care professionals, including a committee opinion on reproductive health care for incarcerated individuals that included recommendations for maternal health care. |
|
Advocacy and Research on Reproductive Wellness of Incarcerated People |
Advocacy and Research on Reproductive Wellness of Incarcerated People research addresses reproductive health care issues for incarcerated women. It conducted the Pregnancy in Prison Statistics project, which collected data on the number of incarcerated pregnant women and the outcomes of their pregnancies. |
|
Ostara Initiative |
Evolving from existing doula programs in a Minnesota prison and an Alabama prison, the Ostara Initiative supports pregnant and parenting individuals across nine state prisons and jails in these two states.a The Ostara Initiative also researches and participates in policy development related to health and justice. |
|
Texas Jail Project |
Among other functions, the Texas Jail Project monitors, documents, and reports on jail conditions and advises lawmakers on jail issues in Texas. This includes developing and advocating for legislation to require jails to report the number of pregnant women booked into their facilities, provide prenatal care, and restrict the use of restraints for pregnant and postpartum women, among other topics. |
|
Women & Justice Project |
The Women & Justice Project works with currently and formerly incarcerated women to transform the criminal legal system. The Women & Justice Project has published work related to incarcerated pregnant women, including infographics on pregnancy and childbirth for incarcerated women. |
Source: GAO summaries of nongovernmental organization information. | GAO‑25‑106404
aDoulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
We asked officials from each NGO about their perspectives on maternal health care in prisons and jails relevant to their areas of work. We discussed the following topics, as relevant: (1) data on incarcerated pregnant women, (2) federal grant funding for providing maternal health care, (3) maternal health care and services for incarcerated women, (4) programs available to incarcerated pregnant women, and (5) challenges and opportunities for providing maternal health care or programs for this population.
Available Data on Incarcerated Pregnant Women
To address our first question on what data are available on the characteristics of pregnant women in state prisons and local jails, as well as pregnancy outcomes, we interviewed or received written responses from Department of Justice (DOJ) and Health and Human Services (HHS) officials about the extent to which they collect data on this population. We reviewed datasets from HHS that include data on maternal health and pregnancy outcomes to determine to what extent, if any, we could identify incarcerated women in these datasets. This included meetings with officials from HHS to discuss what data, if any, we could identify on the maternal health outcomes of incarcerated women from the Healthcare Cost and Utilization Project, Pregnancy Risk Assessment Monitoring System, National Vital Statistics System, Pregnancy Mortality Surveillance System, and Maternal Mortality Review Information Application.[87] We also reviewed available reports from DOJ’s Bureau of Justice Statistics (BJS) that provided relevant data.[88] Additionally, we reviewed the results of a BJS study on the feasibility of collecting data on the health needs of pregnant women in the criminal justice system.[89] These data include the number of incarcerated pregnant women, outcomes of pregnancies, the provision of pregnancy care and services, the health status of pregnant women, and racial and ethnic disparities in maternal health at the federal, state, tribal, and local levels. We also spoke with BJS officials about their findings from this feasibility study and next steps for this effort.
We also interviewed officials representing our sample of nine prisons and nine jails about the data that they collect on pregnant women in their facilities, including data on demographics and pregnancy and maternal health outcomes. Additionally, we asked about challenges to collecting these data and the extent to which officials share these data with other entities, including under what circumstances, if any, these officials report data to federal entities. Further, we asked officials from state DOCs about the data they collect or receive from facilities on incarcerated pregnant and postpartum women, and whether they report these data to federal entities.
We also reviewed the 12 articles we identified as part of our literature review that included data on the number, characteristics, and outcomes of the incarcerated pregnant population. We reported the relevant findings of these studies to demonstrate what data are available on this population.
Available Federal Support
To address our second question on available federal assistance to support maternal health care in state prison and local jails, we asked officials from DOJ and HHS about funding or other forms of assistance they provide that could support this care. We also asked the officials representing the nine prisons and nine jails that we met with if they were aware of any federal assistance that could be used to support maternal health care in their facilities. We also asked what types of federal assistance would be useful if it was available.
To identify whether any DOJ grant funds were used to support maternal health care in state prisons and local jails, we collected and analyzed grant award data from two DOJ grant systems, including the Grants Management System and JustGrants.[90] We requested key word searches of the terms “prenatal care,” “maternal care,” “maternity care,” “post-partum care,” “perinatal,” “maternal health,” “maternal morbidity,” “maternal mortality,” and “maternal death” for all DOJ grants awarded from fiscal year 2018 through April 2023 (the date of the most recent complete data available at the time of our searches). For each search result, we analyzed the award data to determine whether DOJ awarded grant funds to support maternal health care in state prisons and local jails. We assessed the availability and reliability of the DOJ data by interviewing DOJ officials familiar with these systems and reviewing available data dictionaries for these systems. We determined that the DOJ data were sufficiently reliable for the purposes of identifying grants with relevant award descriptions.
Additionally, we interviewed and collected information from DOJ’s Office of Justice Programs (OJP) officials about their knowledge and experience with administering grant funding, including whether any grant funding could be or has been used to support maternal health care in state prisons and local jails.
To identify whether any HHS grant funds were used to enhance maternal health care in state prisons and local jails, we interviewed and collected information from HHS officials, including those from the Administration for Children and Families (ACF) and Health Resources and Services Administration (HRSA). In particular, we gathered information about HHS officials’ knowledge and experience with administering grant funding, including whether any grant funding could or has been used to support maternal health care in state prisons and local jails. We also met with officials from the Office of the Assistant Secretary for Financial Resources to discuss HHS grant data systems. ACF and HRSA officials each provided us with a list of grant awards that they said have been used to support maternal health care in state prisons and local jails from fiscal year 2018 through 2023.
To identify these awards, ACF officials reported requesting that all regional Head Start and Early Head Start grant program managers identify whether any award recipients reported using funds to provide maternal health care for incarcerated pregnant women.[91] Additionally, HRSA officials identified grant program awards that recipients used to support maternal health care in state prisons and local jails through keyword searches in two data systems. HRSA officials searched reports from Healthy Start Initiative grant recipients in one of these data systems, the Electronic Handbooks system, using key words including “incarcerated,” “correctional facilities,” “prison,” and “jail.”[92] Officials also searched another data system, the Title V Information System, which collects financial, programmatic, and performance measure data, along with narrative reports, from state Title V programs.[93] Officials searched this data system using key words including “incarcerated,” “correctional facilities,” “prison,” “jail,” and “juvenile detention.” We reviewed the award narrative information for each result to confirm that recipients used these awards to support maternal health care in state prisons and local jails. We determined that the HHS data were sufficiently reliable for the purposes of identifying grants with relevant award descriptions.
To identify whether DOJ and HHS grant solicitations, also known as notices of funding opportunity, identified maternal health care in prison and jails as an allowable use of funding for any of its grant programs, we asked DOJ and HHS to identify which grant programs could be used to support maternal health care in state prisons and local jails. We then reviewed all 39 available grant solicitations for the 10 DOJ grant programs that officials told us could be used to support maternal health in state prisons and local jails from fiscal years 2018 through 2023.[94] We also reviewed a sample of five grant solicitations for the five HHS grant programs that officials told us could be used to support maternal health in state prisons and local jails from fiscal years 2018 through 2023.[95] We also searched DOJ and HHS websites for information on relevant grant programs.
We also reviewed the efforts that DOJ and HHS are taking to respond to the White House Blueprint for Addressing the Maternal Health Crisis (blueprint) by interviewing and collecting information from knowledgeable DOJ and HHS officials and reviewing the actions and goals for DOJ and HHS described in the blueprint.[96]
Maternal Health Care Provision
To address our third question on how selected state prisons and local jails provide maternal health care for incarcerated pregnant women, we obtained information from officials representing selected facilities to determine the policies and practices that these facilities have for providing maternal health care. We asked facility officials about any standards from professional organizations that guide the policies and practices they have for providing maternal health care. Using our prior work on pregnant women in federal custody, we developed a list of services and types of care that we reviewed with officials to determine if they provided these services and types of care at the facilities they represented.[97] These officials also provided information about programs, such as nursery or doula programs, that the facilities they represented make available to pregnant and postpartum women. Additionally, we asked officials to share information about any other services that the facilities they represented provide for pregnant and postpartum women. In some cases, officials also provided documentation. For example, officials representing some facilities provided copies of facility policies and written information about specific programs these facilities provide to pregnant and postpartum women, such as nursery programs or peer education opportunities.
During our site visits to selected facilities, we interviewed officials who provide care to pregnant and postpartum women and observed some places where they provide this care at the prisons and jails, including medical facilities and nursery programs. As described previously, in addition to our interviews with officials, we also met with selected pregnant and postpartum women in two prisons and two jails across three states. We asked them about the services and types of care they received, their awareness of and participation in certain programs, and their perspectives of the accessibility and quality of care. We also asked whether they had been placed in restraints or restrictive housing while pregnant.
Challenges and Opportunities for Providing Maternal Health Care
To respond to our fourth objective on the challenges to providing maternal health care for incarcerated pregnant and postpartum women, we met with officials representing selected facilities about the challenges they experience in providing this care. We analyzed their responses to identify shared challenges. Additionally, officials from the NGOs we met with also provided insight into the challenges associated with providing maternal health care in carceral settings. Further, we identified challenges discussed in some of the 33 articles we selected through our literature review for this objective question. Where appropriate, we also included information that pregnant and postpartum women shared with us during our interviews with them.
To identify opportunities to enhance maternal health care in prisons and jails, we used information that officials from NGOs reported to us. Additionally, we identified opportunities reported in some of the 33 articles from our literature review. We analyzed the recommendations that these articles made related to how facilities provide maternal health care to identify shared themes.
We conducted this performance audit from November 2022 to October 2024 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
We conducted a literature review to: (1) identify available data on the characteristics of incarcerated pregnant women and their pregnancy outcomes and to (2) learn about the challenges to providing maternal health care in state prisons and local jails and actions identified to enhance this care.[98] Through this review, we identified articles that included data on the pregnant or postpartum population incarcerated in state prisons or local jails or that discussed challenges, recommended standards, or programs related to providing maternal health care for this population.
To identify these articles, we conducted keyword searches in ProQuest, Dialog Healthcare Databases, Scopus, Ebsco, and PubMed for publications from January 2013 through April 2023. These key word searches included searches for data on the number of pregnant and postpartum women incarcerated in state prisons or local jails, characteristics of these women, and their pregnancy and maternal health outcomes. We selected the articles listed below for inclusion in this report. For more information about how we selected these articles, see appendix I.
Ahlbach, Chris, Carolyn Sufrin, and Rebecca Shlafer. “Care for Incarcerated Pregnant People with Opioid Use Disorder: Equity and Justice Implications.” Obstetrics & Gynecology, vol. 136, no.3 (2020): 576-581, https://doi.org/10.1097/AOG.0000000000004002
Alirezaei, Somayeh, and Robab Latifnejad. “The Needs of Incarcerated Pregnant Women: A Systematic Review of Literature.” International Journal of Community Based Nursing & Midwifery, vol. 10, no. 1 (2022): 1-16, https://doi.org/10.30476/IJCBNM.2021.89508.1613
Asiodu, Ifeyinwa V., Lauren Beal, and Carolyn Sufrin. “Breastfeeding in Incarcerated Settings in the United States: A National Survey of Frequency and Policies.” Breastfeeding Medicine, vol. 16, no. 9 (2021): 710-716, https://doi.org/10.1089/bfm.2020.0410
Association of Women’s Health, Obstetric and Neonatal Nurses. “Nursing Care of Incarcerated Women during Pregnancy and the Postpartum Period.” Journal of Obstetric, Gynecologic & Neonatal Nursing, vol. 47, no. 2 (2018): 236-238, https://doi.org/10.1016/j.jogn.2018.01.001
Baldwin, Adele, Agnieszka Sobolewska, and Tanya Capper. “Pregnant in Prison: An Integrative Literature Review.” Women and Birth, vol. 33, no.1 (2020): 41-50, https://doi.org/10.1016/j.wombi.2018.12.004
Cross, JaNeen. “Imprisoning Pregnant and Parenting Women: A Focus on Social Justice, Equal Rights, and Equality.” Health & Social Work, vol. 45, no. 3 (2020): 195-201, https://doi.org/10.1093/hsw/hlaa008
Ferszt, Ginette G., Joyce E. Hickey, and Kimberly Seleyman. “Advocating for Pregnant Women in Prison: The Role of the Correctional Nurse.” Journal of Forensic Nursing, vol. 9, no. 2 (2013): 105-110, https://doi.org/10.1097/JFN.0b013e318281056b
Ferszt, Ginette G., Michelle Palmer, and Christine McGrane. “Where Does Your State Stand on Shackling of Pregnant Incarcerated Women?” Nursing for Women’s Health, vol. 22, no. 1 (2018): 17-23, https://doi.org/10.1016/j.nwh.2017.12.005
Fritz, Stephanie, and Kevin Whiteacre. “Prison Nurseries: Experiences of Incarcerated Women during Pregnancy.” Journal of Offender Rehabilitation, vol. 55, no. 1 (2016): 1-20, https://doi.org/10.1080/10509674.2015.1107001
Goshin, Lorie S., Joyce A. Arditti, Danielle H. Dallaire, Rebecca J. Shlafer, and Allison Hollihan. “An International Human Rights Perspective on Maternal Criminal Justice Involvement in the United States.” Psychology, Public Policy and Law, vol. 23, no. 1 (2017): 53-67, https://doi.org/10.1037/law0000101
Hatters Friedman, Susan, Aimee Kaempf, and Sarah Kauffman. “The Realities of Pregnancy and Mothering While Incarcerated.” The Journal of the American Academy of Psychiatry and the Law, vol. 48, no.3 (2020): 365-375.
Howland, Mariann A., Bethany Kotlar, Laurel Davis, and Rebecca J. Shlafer. “Depressive Symptoms among Pregnant and Postpartum Women in Prison.” Journal of Midwifery & Women’s Health, vol. 66, no. 4 (2021): 494-502, https://doi.org/10.1111/jmwh.13239
Hutchinson-Colas, Juana, and Khadija AlShowaikh. “Pregnant Behind Bars.” American Journal of Public Health, vol. 112, no. 1 (2022): 14-16, https://doi.org/10.2105/AJPH.2021.306580
Kelsey, C.M., Nickole Medel, Carson Mullins, Danielle Dallaire, and Catherine Forestell. “An Examination of Care Practices of Pregnant Women Incarcerated in Jail Facilities in the United States.” Maternal and Child Health Journal, vol. 21 (2017): 1260-1266, https://doi.org/10.1007/s10995‑016‑2224‑5
Kelsey, Caroline M., Morgan J. Thompson, and Danielle H. Dallaire. “Community-Based Service Requests and Utilization among Pregnant Women Incarcerated in Jail.” Psychological Services, vol. 17, no. 4 (2020): 393-404, https://doi.org/10.1037/ser0000314
King, Zoe, Camille Kramer, Carl Latkin, and Carolyn Sufrin. “Access to Treatment for Pregnant Incarcerated People with Opioid Use Disorder: Perspectives from Community Opioid Treatment Providers.” Journal of Substance Abuse Treatment, vol. 126 (2021): 1-9, https://doi.org/10.1016/j.jsat.2021.108338
Kirubajaran, Abirami, Jackie Tsang, Susan Dong, Jeanette Hui, Padmaja Sreeram, Zuhal Mohmand, Shannon Leung, Alesandra Ceccacci, and Mara Sobel. “Pregnancy and Childbirth during Incarceration: A Qualitative Systematic Review of Lived Experiences.” BJOG: An International Journal of Obstetrics and Gynecology, vol. 129 (2022): 1460-1472, https://doi.org/10.1111/1471‑0528.17137
Knittel, Andrea, Angeline Ti, Sarah Schear, and Megan Comfort. “Evidence-Based Recommendations to Improve Reproductive Healthcare for Incarcerated Women.” International Journal of Prisoner Health, vol. 13, no. 3/4 (2017): 200-206, https://doi.org/10.1108/IJPH‑07‑2016‑0031
Knittel, Andrea K., Samantha Zarnick, John M. Thorp Jr., Elton Amos, and Hendree E. Jones. “Medications for Opioid Use Disorder in Pregnancy in a State Women’s Prison Facility.” Drug and Alcohol Dependence, vol. 214 (2020): 1-5, https://doi.org/10.1016/j.drugalcdep.2020.108159
Kotlar, Bethany, Rachel Kornrich, Michelle Deneen, Catelynn Kenner, Lauren Theis, Silke von Esenwein, and Amy Webb-Girard. “Meeting Incarcerated Women’s Needs for Pregnancy Related and Postpartum Services: Challenges and Opportunities.” Perspectives on Sexual and Reproductive Health, vol. 47, no. 4 (2015): 221-225, https://doi.org/10.1363/47e3315
Kramer, Camille, Karenna Thomas, Ankita Patil, Crystal M. Hayes, and Carolyn B. Sufrin. “Shackling and Pregnancy Care Policies in US Prisons and Jails.” Maternal and Child Health Journal, vol. 27 (2023): 186-196, https://doi.org/10.1007/s10995‑022‑03526‑y
Kramer, Camille, Ashley-Devon Williamston, Rebecca J. Shlafer, and Carolyn B. Sufrin. “COVID-19’s Effect on Pregnancy Care for Incarcerated People.” Health Equity, vol. 6, no. 1 (2022): 406-411, https://doi.org/10.1089/heq.2022.0035
Kuhlik, Lauren, and Carolyn Sufrin. “Pregnancy, Systematic Disregard and Degradation, and Carceral Institutions.” Harvard Law & Policy Review, vol. 14, no. 2 (2020): 417-466.
Lipnicky, Ashlyn, Sierra Stites, Carolyn Sufrin, Jennifer K. Bello, Rebecca Shlafer, Patricia J. Kelly, and Megha Ramaswamy. “Jail Provision of Pregnancy and Sexual Health Services in Four Midwestern States.” Women’s Health Issues, vol. 33, no. 1 (2023): 97-104, https://doi.org/10.1016/j.whi.2022.07.004
Nair, Smriti, James E. McGreevy, Juana Hutchinson-Colas, Heather Turock, Frank Chervenak, and Gloria Bachmann. “Pregnancy in Incarcerated Women: Need for National Legislation to Standardize Care.” Journal of Perinatal Medicine, vol. 49, no. 7 (2021): 830-836, https://doi.org/10.1515/jpm‑2021‑0145
Peeler, Mary, Kevin Fiscella, Mishka Terplan, and Carolyn Sufrin. “Best Practices for Pregnant Incarcerated Women with Opioid Use Disorder.” Journal of Correctional Health Care, vol. 25, no. 1 (2019): 4-14, https://doi.org/10.1177/1078345818819855
Pendelton, Virginia E., Elizabeth M. Schmitgen, Laurel Davis, Rebecca J. Shlafer. “Caregiving Arrangement and Caregiver Well-being when Infants are Born to Mothers in Prison.” Journal of Child and Family Studies, vol. 31 (2022): 1894-1907, https://doi.org/10.1007/s10826‑021‑02089‑w
Rajagopal, Karissa, Deborah Landis-Lewis, Kimberly Haven, and Carolyn Sufrin. “Reproductive Health Care for Incarcerated People: Advancing Health Equity in Unequitable Settings.” Clinical Obstetrics and Gynecology, vol. 66, no. 1 (2023): 73-85, https://doi.org/10.1097/grf.0000000000000746
Rose, Susan J., and Thomas P. LeBel. “Confined to Obscurity: Health Challenges of Pregnant Women in Jail.” Health & Social Work, vol. 45, no. 3 (2020): 177-185, https://doi.org/10.1093/hsw/hlaa015
Shlafer, Rebecca J., Erica Gerrity, and Grant Duwe. “Pregnancy and Parenting Support for Incarcerated Women: Lessons Learned.” Progress in Community Health Partnerships: Research, Education, and Action, vol. 9, no. 3 (2015): 371-378, https://doi.org/10.1353/cpr.2015.0061
Shlafer, Rebecca J., Erica Gerrity, Chauntel Norris, Rachel Freeman-Cook, and Carolyn B. Sufrin. “Justice for Incarcerated Mom’s Act of 2021: Reflections and Recommendations.” Women’s Health, vol. 18, no. I-II (2022): 1-11, https://doi.org/10.1177/17455057221093037
Shlafer, Rebecca, Jennifer Saunders, Christy Boraas, Katy Kozhimannil, Narayana Mazumder, Rebecca Freese. “Maternal and Neonatal Outcomes among Incarcerated Women Who Gave Birth in Custody.” Birth, vol. 48 (2021): 122-131, https://doi.org/10.1111/birt.12524
Steely Smith, Mollee K., Stephanie H. Wilson, and Melissa J. Zielinski. “An Integrative Literature Review of Substance Use Treatment Service Need and Provision to Pregnant and Postpartum Populations in Carceral Settings.” Women’s Health, vol. 19 (2023): 1-13, https://doi.org/10.1177/17455057221147802
Suarez, Alicia. “‘I Wish I Could Hold Your Hand’: Inconsistent Interactions Between Pregnant Women and Prison Officers.” Journal of Correctional Health Care, vol. 27, no. 1 (2021): 23-29, https://doi.org/10.1089/jchc.19.06.0048
Sufrin, Carolyn, and Committee on Health Care for Underserved Women. “Reproductive Health Care for Incarcerated Pregnant, Postpartum, and Nonpregnant Individuals: ACOG Committee Opinion, Number 830.” Obstetrics and Gynecology, vol. 138, no.1 (2021): 24-34, https://doi.org/10.1097/aog.0000000000004429
Sufrin, Carolyn, Lauren Beal, Jennifer Clarke, Rachel Jones, and William Mosher. “Pregnancy Outcomes in US Prisons, 2016–2017.” AJHP Open-Themed Research, vol. 109, no. 5 (2019): 799-805, https://doi.org/10.2105/AJPH.2019.305006
Sufrin, Carolyn, Rachel Jones, William Mosher, and Lauren Beal. “Pregnancy Prevalence and Outcomes in U.S. Jails.” Obstetrics & Gynecology, vol. 135, no. 5 (2020): 1177-1183, https://doi.org/10.1097/AOG.0000000000003834
Sufrin, Carolyn B., and Andrea Knittel. “Health Care and Social Justice Implications of Incarceration for Pregnant People Who Use Drugs.” International Review of Psychiatry, vol. 33, no. 6 (2021): 557-571, https://doi.org/10.1080/09540261.2021.1887097
Sufrin, Carolyn, Lauren Sutherland, Lauren Beal, Mishka Terplan, Carl Latkin, and Jennifer Clark. “Opioid Use Disorder Incidence and Treatment Among Incarcerated Pregnant People in the U.S.: Results from a National Surveillance Study.” Addiction, vol. 115, no. 11 (2020): 2057-2065, https://doi.org/10.1111/add.15030
Wouk, Kathryn, Jaslyn Piggott, Sarah Towner Wright, Aunchalee E.L. Palmquist, and Andrea Knittel. “Lactation Support for People Who Are Incarcerated: A Systematic Review.” Breastfeeding Medicine, vol. 17, no. 11 (2022): 891-925, https://doi.org/10.1089/bfm.2022.0138
Department of Health and Human Services Grant Programs
The Department of Health and Human Services’ (HHS) Health Resources and Services Administration (HRSA) and Administration for Children and Families (ACF), among other HHS agencies, award federal assistance through their many grants programs to state, local, and tribal governments. HHS has five grant programs that could be used to enhance maternal health care in prisons and jails. Officials from HHS’s ACF and HRSA told us that while their grant programs are not specifically designed for providing maternal health care in prisons and jails, award funds for five grant programs could be used for this purpose. Table 4 provides more information about these five grant programs.
|
Grant program |
Purpose of grant program |
Entities eligible to receive awards |
|
Community Services Block Grant program |
To support services that alleviate the causes and conditions of poverty in under-resourced communities. |
State governments, U.S. territory governments, as well as tribal governments and organizationsa |
|
Head Start and Early Head Start Grant Program |
To increase the number of low-income children receiving high-quality, comprehensive early education services and pregnant persons receiving high-quality prenatal and postpartum services. |
Local public or private non-profit agencies, including community-based and faith-based organizations, or local for-profit agencies |
|
Healthy Start Initiativeb |
To reduce rates of infant death, improve maternal health outcomes, and reduce racial and ethnic disparities. |
Domestic public or private entities, domestic faith-based and community-based organizations, tribes, and tribal organizations |
|
Social Services Block Grant program |
To provide essential social services that promote self-sufficiency and protect children and adults from neglect, abuse, and exploitation. |
State governments and U.S. territory governments |
|
Title V Maternal and Child Health Services Block Grant program |
To improve public health systems for mothers, children, and their families, including supporting children and youth with special health care needs. |
Health agencies of states, U.S. territories, and the Marshall Islands, Micronesia, and Palau |
Source: GAO analysis of HHS information. | GAO‑25‑106404
aState governments must allocate 90 percent of grant award funds to local eligible entities that meet requirements outlined in the Community Services Block Grant Act.
bAwards were available in fiscal years 2019 and 2023.
Department of Justice Grant Programs
The Department of Justice’s (DOJ) Office of Justice Programs (OJP), the largest grantmaking component of DOJ, awards federal assistance through its many grant programs. According to OJP officials, OJP has 10 grant programs that can be used to support maternal health care in state prisons and local jails. OJP officials told us that while these grant programs are not specifically designed for providing maternal health care in prisons and jails, award funds could be used for this purpose. Table 5 provides information about these 10 grant programs.
|
Grant program and fiscal year(s) available |
Purpose of grant program |
Entities eligible to receive awards |
|
Adult Drug Court Discretionary Grant Programa (2018 through 2023
|
To provide financial and technical assistance to eligible entities to plan, implement, and enhance the operations of adult treatment courts. |
State governments, city or township governments, county governments, and other eligible public or private entitiesb |
|
Comprehensive Opioid, Stimulant, and Substance Abuse Site-Based Programc (2018 through 2023) |
To support eligible entities to plan, develop, and implement comprehensive efforts that identify, respond to, treat, and support those impacted by the use and misuse of opioids, stimulants, and other substances. |
State governments, city or township governments, county governments, and other eligible public entities |
|
Improving Adult and Juvenile Crisis Stabilization and Community Reentry Program (2022 through 2023) |
Supports eligible entities to provide comprehensive treatment, recovery, and other supportive reentry services to people experiencing mental health, substance use, or co-occurring disorders who are currently involved in the criminal justice system or were formerly involved.d |
State, local, and tribal governments, as well as community-based nonprofit organizations |
|
Residential Substance Abuse Treatment Program (2018 through 2023) |
Assists states with developing and implementing residential substance use disorder treatment programs within state and local correctional facilities. |
State governments |
|
Second Chance Act: Community-based Reentry Programe (2018 through 2023) |
Provides funding to eligible entities who are providing comprehensive reentry services to individuals who have been incarcerated. |
Federally recognized tribal governments and certain nonprofits |
|
Second Chance Act: Improving Reentry Education and Employment Outcomes Programf (2021 through 2023) |
Supports eligible entities to implement and expand education and employment programs that serve individuals during incarceration and community reentry. |
State governments, city or township governments, county governments, certain nonprofits, and other eligible public and private entities |
|
Second Chance Act: Improving Substance Use Disorder Treatment and Recovery Outcomes for Adults in Reentry Program (2022 through 2023) |
To implement or expand systems approaches that improve outcomes for adults with substance use disorders who are reentering communities. |
State governments, city or township governments, county governments, certain nonprofits and other eligible public and private entities |
|
Second Chance Act: Pay for Success Programg (2019 through 2023) |
To enhance or implement clinical services and other evidence-based responses to improve reentry, reduce recidivism, and address the treatment and recovery needs of people with mental health, substance use, or co-occurring disorders who are currently involved in the criminal justice system or were formerly involved |
State governments, city or township governments, county governments, and other eligible public entities |
|
Second Chance Act: Smart Supervision Programh (2022 through 2023) |
To increase the capacity and increase the ability of probation and parole agencies to improve supervision success rates, thereby increasing community safety and reducing crime. |
State governments, city or township governments, county governments, and other eligible public entities |
|
Second Chance Act: Statewide Adult Recidivism Reduction Program (2018) |
To provide state agencies with resources and technical assistance that will result in improved reentry systems and reduced recidivism among populations released from incarceration. |
Limited to the five state recipients of the fiscal year 2017 Second Chance Act Statewide Adult Recidivism Reduction Strategic Planning Program awards. These five state recipients include Alaska, Utah, Louisiana, Delaware, and the District of Columbia. |
Source: GAO analysis of DOJ information. | GAO‑25‑106404
aAdult Drug Court and Veterans Treatment Court Discretionary Grant Program in 2020 and 2021.
bOther eligible public and private entities eligible for DOJ grant programs in this table may include, among others, federally recognized tribal governments, public housing authorities/Indian housing authorities, special district governments, other units of state and local governments, independent school districts, and for-profit organizations other than small businesses.
cComprehensive Opioid Abuse Site-based Program in 2018 and 2019, and the Comprehensive Opioid, Stimulant, and Substance Abuse Site-based Program in 2020, 2021, and 2022.
dAccording to the National Institute of Justice within DOJ’s Office of Justice Programs, reentry refers to the transition from life in jail or prison to life in the community.
eSecond Chance Act Comprehensive Community-Based Adult Reentry Program in 2018 and 2019.
fSecond Chance Act: Adult Reentry Education, Employment, Treatment and Recovery Program in 2021.
gSecond Chance Act: Pay for Success Initiative in 2021 and 2022; Second Chance Act Pay for Success Initiative: Outcomes-based Contracting to Lower Recidivism and Address Substance Use Disorders Through Reentry and Housing Services in 2020; and the Second Chance Act Pay for Success Initiative: Outcomes-based Contracting to Lower Recidivism and Homelessness in 2019.
hSmart Reentry and Supervision: Grants, Tools, and Technical Assistance to Facilitate Change program in 2022.
The Department of Health and Human Services’ (HHS) Administration for Children and Families (ACF) and Health Resources and Services Administration (HRSA) award federal assistance through their many grant programs, among other HHS agencies.[99] According to officials and grant documentation, at least 23 awards under the Healthy Start Initiative, Head Start and Early Head Start, and Title V Maternal and Child Health Services Block Grant programs were used to support maternal health care in prisons and jails during fiscal year 2018 through 2023.[100] See table 6 for more information about each award.
|
Award recipient |
How award funds are supporting maternal health care |
|
Head Start and Early Head Start grant programa |
|
|
Lead
|
Leads provides Early Head Start services to the mothers and infants in the Achieving Baby Care Success Nursery at the Ohio Reformatory for Women. The nursery allows children to stay with their mothers during their incarceration. As part of the program, Leads assigned a home visitor who offers weekly sessions and biweekly socialization events. The home visitor provides targeted learning opportunities to assist mothers in building their parenting skills. |
|
Child Development Council of Franklin County, Inc. |
Child Development Council of Franklin County, Inc. partnered with the social services department at the Franklin County Correction Center in Ohio to provide case management services to incarcerated pregnant women. A family service worker meets with the women each week to provide workshops on topics such as fetal development, maternal mental health, lifestyle changes, and breastfeeding. The women also learn how to obtain services they will need upon their release, such as housing and employment, as well as how to regain custody of their other children and maintain their sobriety. Child Development Council of Franklin County, Inc. also assists mothers with placing their babies in kinship or foster care and enrolls the babies in Early Head Start. They also partnered with another program at the Franklin County Correction Center to provide services to pregnant women with substance use disorder. |
|
Central Missouri Community Action |
Central Missouri Community Action partnered with the Women’s Eastern Reception, Diagnostic, and Correctional Center to support the health and well-being of participating incarcerated pregnant women. Program staff conduct weekly visits and provide participants with depression and nutritional screenings as well as child and maternal health education materials. They also share information about what to expect during delivery and options for the babies after birth, such as kinship care, foster care, or a local community program. They provide pregnant women with access to information to support their health and wellness, as well as that of their babies, and have a prenatal program to support incarcerated women and their newborns. |
|
Wyoming Child & Family Development, Inc. |
Wyoming Child and Family Development, Inc. provides services to incarcerated pregnant women in two prisons in Wyoming. They conduct weekly visits and hold group socializations and meetings. Once the babies are delivered, the women are usually transferred to the prison in Casper, Wyoming. The infants may be placed with relatives or foster care families in the Casper, Wyoming area. The program enrolls the babies in Early Head Start with their caregivers. The Early Head Start program also maintains contact with the incarcerated women to support reunification with their child or children, and to support planning for the future—such as working with community organizations for housing, employment, and childcare. |
|
Oahe Child Development Center, Inc. |
Oahe Child Development Center, Inc. works with the South Dakota Department of Corrections to provide services to incarcerated pregnant and postpartum women participating in the Mother Infant Program, a nursery program that allows children to stay with their mothers during their incarceration. They conduct weekly home visits and hold group meetings at the prison where the incarcerated pregnant women reside. Once the babies are delivered, the infants are enrolled in Early Head Start and receive weekly home visits and socialization opportunities. The infants are also supported by caregivers while the incarcerated mothers work. |
|
University of Nevada Reno Early Head Start Program |
The program provides services, including prenatal services, to pregnant women who are incarcerated and defined as homeless. They also conduct outreach with treatment programs to assist mothers released to treatment programs. |
|
Washington State: Puget Sound Early Head Start-Washington Corrections Center for Women (WCCW) |
Puget Sound Educational Service District provides services to women incarcerated at the Washington Corrections Center for Women, including those in the nursery program. The program supports child development and the parent-child relationship. The mothers receive coaching and mentorship focused on child development. They partner with the mothers to assess their development, health, nutrition, and safety needs and provide information about how to access health, nutrition, oral health, and mental health community resources. They also cover topics such as maternal depression education and screening, bonding and attachment, childhood exams, developmental screenings, and school readiness. |
|
Oregon State: Community Action Organization-Coffee Creek Child Development Center |
The Community Action Organization offers services to incarcerated mothers housed at Coffee Creek Women’s Correctional Facility in Wilsonville, Oregon. They support eight children and their mothers in a year-round program. They meet twice per week with the support of a teacher, family advocates, an education specialist, and a mental health consultant. They support activities that focus on child development, education, health, nutrition, and family support. Staff provide intensive transition planning for post-release, ensuring families are successfully connected to an Early Head Start or Head Start program in their home community. |
|
Healthy Start Initiative grant programb |
|
|
County of Fresno |
The program funds a public health nurse and staff from the county Department of Behavioral Health (including a substance abuse specialist) and a health center to provide pregnancy health education, substance use assessment, and health care services information to pregnant women at a local county jail on a weekly basis. The program offers pregnant women case management services and referrals for follow-up upon release from jail. |
|
Maricopa County Department of Health |
The South Phoenix Healthy Start Initiative doulas and case managers provide incarcerated parents within the jail systems of south Phoenix, Arizona, including pregnant women at Estrella Jail, virtual and in-person visitation, care coordination, and health education, and they connect participants with community resources.c The program arranges case management visits and joint family visits. Additionally, the Birth Behind Bars program trains doulas to care for pregnant women. Doulas assist during birth, attend hospital births, and conduct prenatal and postnatal visits. Case managers and doulas continue to offer support and assistance after release from jail. |
|
County of Sedgwick, Kansas, Healthy Babies Sedgwick County Division of Health |
The Healthy Babies program coordinates with a residential work release program to explore ways to collaborate with other programs that serve incarcerated populations, including the juvenile detention center and the county jail. |
|
MomsFirst Cleveland Health Department |
MetroHealth Medical Center, the Cuyahoga County, Ohio hospital, provides medical care in a local jail, along with county jail staff. Healthy Start funding helps support a portion of a family medicine doctor’s salary and a full-time medical assistant who ensure the jail complies with the recommended prenatal visit schedule. They also aim to reduce the number of Cesarean section deliveries and increase maternal support for pregnant and postpartum women at the jail. |
|
The Family Tree Information Education and Counseling Center |
The Family Tree Healthy Start Program provides services and supports incarcerated women in the Lafayette Parish Correctional Center in Louisiana and partners with Project H.O.P.E. (Helping Offenders Parent Effectively), a 6-week group-based psychoeducational parenting class available to women at the jail. The Family Tree Healthy Start Program meets one-on-one with pregnant women at the jail to discuss the services they provide for incarcerated women, how their partner or family can be involved, and what happens when they are released from jail. A case manager meets with the women regularly to provide support, answer questions, and advocate for their needs. |
|
Title V Maternal and Child Health Services Block Grant programd |
|
|
State of Alabama |
Alabama is undertaking various efforts to reduce opioid use and neonatal abstinence syndrome, including for the incarcerated population. These efforts include providing access to universal testing and access to treatment options. Alabama also funds an organization that provides free dental treatment to mothers, which receives referrals from organizations that provide services to incarcerated women with children. |
|
State of Arkansas |
Distributing reproductive and maternal health information flyers to incarcerated women through the Breastfeeding Coalition to raise awareness of available services once incarcerated mothers are released. |
|
State of California |
Funds a local county maternal and child health program to collaborate with the county jail to provide public health nurses to meet with incarcerated women every week to provide health information, resources, and connect them to California maternal and child health programs. |
|
State of Colorado |
Provided subject matter expertise and helped to develop a lactation policy for incarcerated women in Denver with the Denver Sheriff’s Department and distributing the policy to juvenile detention centers and local jails across the state. Colorado also funds a community-based organization to increase the capacity of the doula workforce to service incarcerated pregnant and postpartum women, among other target populations. This includes training 17 doulas across three locations; one of these locations is the Denver Women’s Correctional Facility. At the Denver Women’s Correctional Facility, the doula provides expertise in perinatal substance use and recovery and facilitates peer-led parenting curriculum at the facility. The program also trains doulas at the hospital to work more effectively with incarcerated women during delivery. |
|
State of Delaware |
Provides access to birth control for incarcerated women who are transitioning back into the general population |
|
State of Illinois |
Provides pregnancy education, breastfeeding education, and lactation support and counseling to women in the state’s two women’s correctional facilities. |
|
State of Indiana |
Funding a community-based organization to serve mothers and babies transitioning from the Indiana Women’s Prison to their home communities. The program educates, helps women create resumes and think about job placement, provides necessities, secures housing, and connects these women to social services and health care services. |
|
State of Kansas |
Participating in a U.S. Breastfeeding Coalition learning community focused on lactation support for incarcerated women. |
|
State of Missouri |
Providing health care for women of childbearing age who are incarcerated by the Missouri Department of Corrections. |
|
State of Texas |
Supporting five lactation support centers throughout Texas, including one support center that provides breastfeeding classes at a county correctional facility. |
Source: GAO analysis of Department of Health and Human Services grant information. | GAO‑25‑106404
aThe purpose of the Head Start and Early Head Start grant program is to increase the number of low-income children receiving high-quality, comprehensive early education services and pregnant persons receiving high-quality prenatal and postpartum services.
bThe purpose of the Healthy Start Initiative grant program is to reduce rates of infant death, improve maternal health outcomes, and reduce racial and ethnic disparities.
cDoulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
dThe purpose of the Title V Maternal and Child Health Services Block Grant program is to improve public health systems for mothers, children, and their families. This includes support for children and youth with special health care needs. According to HRSA officials, recipients of the Title V Maternal and Child Health Services Block Brant program must match the funding provided by the grant with state funds. The activities that recipients report funding to HHS may be accomplished with the grant funds, state matching funds, or through a partnership with other agencies and entities. Further, Title V Maternal and Child Health Services Block Grant recipients report to HRSA annually on how the state’s Title V program is addressing a specific Maternal and Child Health topic. State recipients may or may not choose to highlight how their programs support care for incarcerated pregnant and postpartum women. As such, there may be more states that use funds for this purpose that are not included in this table.
We obtained information from officials representing nine state prison facilities and officials representing nine local jail facilities in a nongeneralizable sample of states to discuss maternal health care in their state prison and local jail facilities. We selected this nongeneralizable sample of states based on several factors, including the state’s female incarceration rate, the number of women under the jurisdiction of state correctional authorities, and the number of women confined in local jails to identify states with a range of female incarceration rates that generally had higher numbers of women under the jurisdiction of state correctional authorities or confined in jails.[101]
For each state, we also considered the availability of data on the incarcerated pregnant population, whether we were aware of any federal funding serving this population, and the availability of nursery or doula programs in prison or jail facilities.[102] Additionally, we considered the state’s maternal mortality rate, whether the state has a law in place that restricts the use of restraints on the pregnant population, and racial and ethnic data available for the population under the jurisdiction of state and federal correctional authorities. Finally, we considered the Census region of each state for geographic diversity.
After selecting a nongeneralizable sample of states using these criteria, we identified prisons primarily through contacting state department of corrections (DOC) officials, who indicated which prison in their state we should meet with about maternal health care for incarcerated pregnant women. We generally identified jail facilities for the largest cities in these states because these facilities likely had larger populations and may have recent experience providing care to pregnant women.
We asked officials representing the nine prisons and nine jails we selected about the services and types of care that they provide for pregnant and postpartum women in their facilities. We asked these officials about the services and types of care that we identified and reported on in prior work on pregnant women in federal immigration detention facilities and federal prisons.[103]
Perspectives from Officials Representing Selected State Prisons
Table 7 provides the number of prisons which, according to officials, provide a particular service or type of care. It also includes examples of how officials reported providing some services or types of care.
|
Pregnancy-related service or type of carea |
Number of prisons whose representatives reported providing this service or type of care |
Examples of how officials reported providing this service or type of care |
|
Intake health screening |
9 |
— |
|
Pregnancy testing at intake |
9 |
— |
|
Access to abortionb |
9 |
— |
|
Provision of prenatal care |
9 |
— |
|
Prenatal vitamins |
9 |
— |
|
Provision of labor and delivery care |
9 |
Officials representing all nine prisons reported that pregnant women deliver at hospitals in the community. |
|
Provision of postpartum care |
9 |
— |
|
Recordkeeping on care |
9 |
Officials representing eight of nine prisons reported that medical staff use electronic health records to store data on care.c |
|
Mental health services and counseling |
9 |
— |
|
Substance use disorder care |
9 |
Officials representing seven prisons indicated that the substance use disorder care they provide includes medications for opioid use disorder, though officials representing one of these prisons reported that medical staff taper this treatment for postpartum women.d Officials representing one prison indicated that the substance use disorder care they provide will soon include medications for opioid use disorder because they are starting a program. Officials representing one prison indicated that while they provide substance use disorder care, this care does not include medications for opioid use disorder for pregnant women. |
|
Human immunodeficiency virus (HIV) care |
9 |
— |
|
Nutrition |
9 |
Officials representing five prisons indicated that pregnant women receive supplemental calories. Officials representing one prison reported that pregnant women receive a pregnancy diet. Officials representing one prison told us that everyone receives high-calorie meals at the facility because they receive the same calories as those incarcerated at the men’s facility. Officials representing one prison told us that a clinical dietician works with medical providers to decide on the appropriate nutrition for each pregnant woman in custody. Officials representing one prison indicated that they provide nutritional services to pregnant women but did not specify what these services entail. |
|
Special accommodations |
9 |
— |
|
Lower bunk assignments |
9 |
— |
|
Additional bedding |
1 |
— |
|
Adjusted work assignments |
5 |
— |
|
Special clothing |
6 |
Officials representing three prisons told us that pregnant women receive different color clothing or the option to wear different color clothing. Officials representing four prisons reported that pregnant women receive larger uniform sizes. Officials representing one prison indicated that pregnant women receive pants with expandable waistbands. |
Source: GAO analysis of information provided by officials representing selected state prisons. | GAO‑25‑106404
Note: We spoke with officials representing nine state prison facilities in a nongeneralizable sample of states to discuss maternal health care in their state prison facilities. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as racial and ethnic data available for the population under the jurisdiction of state and federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities, among other factors. Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
aWe identified which of the nine prisons provided each service or type of care based on information that officials representing these nine prison facilities reported or documentation from these facilities. If a facility is excluded from the count of prisons providing a service or type of care, this does not necessarily mean that the facility does not provide that service or type of care. Instead, it may mean that officials did not mention that service or type of care to us, even though the facility they represent provides it. Additionally, we did not independently verify the availability or provision of services and types of care that officials or facility documentation identified as available.
bAccess to abortion services is based on what officials reported to us, which may mean that the facility provides access to abortion within the context of any applicable state laws. Officials made these statements as of the dates of our interviews, and state laws and facility policies may have changed following our interviews.
cOfficials representing one prison indicated that its medical provider maintains its own data system with information on pregnancy, maternal, and general health outcomes but did not specify if that system was electronic or contained individual-level records.
dMedications for opioid use disorder include buprenorphine and methadone.
Perspectives from Officials Representing Selected Jails
Table 8 provides the number of jails which, according to officials, provide a particular service or type of care. It also includes examples of how officials reported providing some services or types of care.
|
Pregnancy-related service or type of carea |
Number of jails whose representatives reported providing this service or type of care |
Examples of how officials reported providing this service or type of care |
|
Intake health screening |
9 |
— |
|
Pregnancy testing at intake |
9 |
— |
|
Access to abortionb |
9 |
— |
|
Provision of prenatal care |
9 |
— |
|
Prenatal vitamins |
9 |
— |
|
Provision of labor and delivery care |
9 |
Officials representing all nine jails reported that pregnant women deliver at hospitals in the community. |
|
Provision of postpartum care |
9 |
— |
|
Recordkeeping on care |
9 |
Officials representing all nine jails reported that medical staff use electronic health records to store data on care. |
|
Mental health services and counseling |
9 |
— |
|
Substance use disorder care |
9 |
Officials representing eight of nine jails indicated that the substance use disorder care they provide includes medications for opioid use disorder, though officials representing one of these jails reported that medical staff taper this treatment for postpartum women.c Officials representing one jail indicated that they provide substance use disorder care but did not specify if this care includes medications for opioid use disorder. |
|
Human immunodeficiency virus (HIV) care |
8 |
— |
|
Nutrition |
9 |
Officials representing six jails reported that pregnant women receive supplemental calories. Officials representing one jail indicated that pregnant women receive additional nutrients. Officials representing one jail told us that pregnant women receive a doctor-approved diet. Officials representing one jail reported that a nutritionist can request specific diets for pregnant patients. |
|
Special accommodations |
9 |
— |
|
Lower bunk assignments |
8 |
— |
|
Additional bedding |
4 |
— |
|
Adjusted work assignments |
1 |
— |
|
Special clothing |
5 |
Officials representing two jails reported that pregnant women receive different color clothing. Officials representing two jails told us that pregnant women can request larger uniform sizes. Officials representing one jail indicated that pregnant women receive pregnancy pants. |
Source: GAO analysis of information provided by officials representing selected local jails. | GAO‑25‑106404
Note: We spoke with officials representing nine local jail facilities in a nongeneralizable sample of states to discuss maternal health care in their local jail facilities. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as racial and ethnic data available for the population under the jurisdiction of state and federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities, among other factors. Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
aWe identified which of the nine jails provided each service or type of care based on information that officials representing these nine jail facilities reported or documentation from these facilities. If a facility is excluded from the count of jails providing a service or type of care, this does not necessarily mean that the facility does not provide that service or type of care. Instead, it may mean that officials did not mention that service or type of care to us, even though the facility they represent provides it. Additionally, we did not independently verify the availability or provision of services and types of care that officials or facility documentation identified as available.
bAccess to abortion services is based on what officials reported to us, which may mean that the facility provides access to abortion within the context of any applicable state laws. Officials made these statements as of the dates of our interviews, and state laws and facility policies may have changed following our interviews.
cMedications for opioid use disorder include buprenorphine and methadone.
We interviewed 27 incarcerated women who were pregnant or had given birth while incarcerated at two state prison and two local jail facilities.[104] These semi-structured interviews included 13 pregnant and 14 postpartum women. 19 of these women were incarcerated in state prisons and eight were incarcerated in local jails. The women we interviewed discussed topics such as medical and mental health services, nutrition, restraint usage, and restrictive housing, among others. Not all the women discussed all the topics, so the number of respondents varies across topics.
Interviews with Pregnant and Postpartum Women Regarding Their Care in State Prisons
We interviewed 19 incarcerated women who were pregnant or had given birth while serving prison sentences at two state prison facilities, including seven pregnant and 12 postpartum women. Eight of the postpartum women were participating in a nursery program and residing with their babies at the time of our interviews. The women we interviewed had been incarcerated for a range of 1 month to 17 months at the time of our visits. See table 9 for more information.
|
Knowledge of pregnancy status |
All 19 of the women we interviewed stated they knew they were pregnant when they arrived at the prison where they were currently incarcerated or associated with their nursery program. Seven women said they were visibly pregnant when they arrived at the prison. Five women said they notified someone they were pregnant, and eight women said the prison already knew that they were pregnant when they arrived. |
|
Pregnancy testing |
Four women told us they received a pregnancy test when they arrived at the prison during intake. |
|
Information about available medical care at the prison |
Ten women we interviewed said that they received some information about medical care services and pregnancy services when they arrived at the prison, and eight did not receive such information. |
|
Medical care received after pregnancy was confirmed |
All 19 women said they saw a medical professional at the prison after their pregnancies were confirmed. The amount of time they said it took to see an obstetrician varied from the day of arrival to 1 month after arrival. |
|
Where medical care was provided |
Eighteen women told us they received additional medical care related to their pregnancies while incarcerated at the prison. One woman said she did not receive any additional care prior to her delivery. Nine women said they received additional medical care both at the prison and in an offsite medical facility. Seven women said they received additional medical care at just the prison. One woman said she received additional medical care solely at an offsite facility. Of the 12 women who had given birth at the time of our interview, nine said that they had a postpartum checkup at the prison. |
|
Health concerns |
Ten women said that they had health concerns related to their pregnancies that they felt should have been addressed when they arrived at the prison. Of these women, six said they notified facility staff of their concerns. Eight women said that they did not have any health concerns related to their pregnancies when they arrived. |
|
Perspectives on care received |
Eight women said they had generally positive perspectives on the care they received. Seven women said the care they received was okay or had mixed perspectives. Two women said the care they received was not good, or that their needs were not addressed by care providers. |
|
Pregnancy counseling and mental health care |
Seven women stated that they were participating in some type of counseling related to their pregnancies. Four women stated they were aware of counseling that was available but did not participate. Six women stated they did not participate in counseling or that it was not available. |
|
Maternity clothing |
Eight women said they received special maternity clothing, including a pink shirt. Ten women said they did not receive special maternity clothing; they received the standard uniform. Three of these 10 women noted they were provided a larger size. |
|
Accommodations and programs |
Four women said there were not additional resources or accommodations for pregnant women at the prison or did not specify any. Seven women mentioned a variety of programs and resources available to them, including exercise, meeting with case workers and social workers, parenting classes, peer education, programs related to coping with trauma, substance use recovery, mental health counseling, and religious programs. One woman indicated she was not able to participate in some programs the prison offered because of her pregnancy and subsequent postpartum status. |
|
Postpartum care |
Of the 12 women who had given birth at the time of our interview, nine said that they had a postpartum checkup at the prison. One woman said she went to the infirmary immediately postpartum. Three women who had already given birth mentioned that mental health counseling after delivering their babies was available and one woman mentioned participating in mental health counseling. Six women mentioned having a lower bunk assignment while postpartum. Two women mentioned a lighter work assignment or break from work assignment while postpartum. |
|
Bunk assignments |
Eighteen women said they had a lower bunk assignment while pregnant or postpartum. |
|
Work assignments |
Six women said they did not have a work assignment or had a light work assignment while pregnant and postpartum. |
|
Prenatal vitamins |
Eighteen women said they received prenatal vitamins while pregnant. |
|
Nutrition |
Eighteen women said they received extra nutrition with a meal, which some women mentioned could be taken with them as a snack for later, such as a sandwich or piece of fruit while pregnant. Seven women told us they had constant access to water and one woman told us she did not have constant access to drinking water. |
|
Restrictive housin
|
Eleven women said they were not placed in restrictive housing while at the prison during their pregnancies. Two women told us they were placed in restrictive housing at the prison during their pregnancies, and two women told us they were placed in restrictive housing when they were postpartum. Three women told us they were isolated in medical segregation or as part of quarantine for COVID-19 during their pregnancies while at the prison. |
|
Restraints |
Ten women said they were not placed in restraints by prison staff while pregnant. Nine women told us they were placed in restraints by prison staff during their pregnancies. Of these nine women, seven told us they were placed in handcuffs, with four women specifying the handcuffs were in front of their bodies. Additionally, two women said their legs were placed in restraints. One woman said her hands and legs were restrained while postpartum. |
|
Requests for additional care |
Fifteen women stated that there was not a particular medical or mental health service that they requested during their pregnancy or postpartum period that they did not receive. One of these women stated she has not requested things she needs because she does not feel staff would care. One woman told us that she did not receive medication she was prescribed, and one woman said she asked for depression medication and mood stabilizers to be restarted while postpartum but did not receive them. One woman said she asked to be taken to the hospital for low blood pressure but was not taken. |
Source: GAO analysis of interviews with pregnant and postpartum women incarcerated in two state prisons. | GAO‑25‑106404
Notes: We interviewed seven pregnant and 12 postpartum women at two state prisons in September 2023 and November 2023. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as the racial and ethnic breakdown of the population under the jurisdiction of state and federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities, among other factors. Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth. We asked officials at these prisons to identify pregnant women and women who had given birth while incarcerated. The prison officials identified these women and asked for volunteers to meet with us. Although these interviews are not generalizable and may not be indicative of the care provided at all state prisons, they provided us with perspectives on the care provided to pregnant women. We did not independently verify statements made by these 19 women we interviewed.
Interviews with Pregnant and Postpartum Women Regarding Their Care in Local Jails
We interviewed eight incarcerated women who were pregnant or had given birth while incarcerated in two local jail facilities, including six pregnant and two postpartum women. The women we interviewed had been incarcerated for a range of 1 week to 7 months at the time of our visits. See table 10 for more information.
|
Knowledge of pregnancy status |
Seven of the eight women we interviewed said they knew or suspected they were pregnant before arriving at the jail. Five of these women told us they notified someone they were pregnant either at the time of their arrests or during jail intake. One of these women said she was already far along in her pregnancy and was visibly pregnant. |
|
Pregnancy testing |
Six women told us they received a pregnancy test when they first arrived at the jail. One woman said she received a pregnancy test at a hospital prior to arriving at the jail and one woman was already far along in her pregnancy and was visibly pregnant. |
|
Information about available medical care at the prison |
Three women stated they received information about available medical care services and pregnancy services when they arrived at the jail. Two women told us they did not receive such information. |
|
Medical care received after pregnancy was confirmed |
All eight women said they saw a medical professional after their pregnancies were confirmed; the care the women received occurred at the jail. Seven women also said they received care at an outside facility, such as a community hospital, for an ultrasound for specialty care. The amount of time they reported it took to see a medical professional after their pregnancies were confirmed varied from the week that they arrived at the jail to 7 weeks after they arrived at the jail. |
|
Where medical care was provided |
Seven women told us they received additional medical care for their pregnancies while at the jail after initial intake and medical screening. Of these women, six said they received this care from both medical staff in the jail as well as from outside facilities, such as the community hospital. One woman said she had recently arrived at the facility at the time of our interview and had not received any additional medical care from the facility yet. She told us she received additional medical care at a hospital when she had an issue related to her pregnancy. |
|
Health concerns |
Five women stated they had health concerns related to their pregnancies that they felt should be addressed when they arrived at the jail. Three of these women told us they notified staff about their concerns, and one had someone else notify staff for them. Four of the five women who told us they had concerns said their concerns were addressed. |
|
Perspectives on care received |
Five women shared positive perspectives on the quality of care they received at the jail and outside facilities. Two women indicated that the care they received from medical staff at intake and the hospital felt rushed. One woman felt her postpartum concerns were not appropriately addressed by her doctor at the jail. |
|
Pregnancy counseling and mental health care |
Two women said they were receiving some support or counseling from a doula.a Two women said they participated in religious counseling or therapy. Two women said they had received mental health care at the jail. One woman was not aware of any available counseling and was told none was provided at the jail. One woman said she chose not to see a mental health counselor because she feared limitations to her privileges and access to other programs. |
|
Pregnancy-related programs |
Six women said someone from the jail met with them to discuss programs available to them related to their pregnancies. Five women told us they were participating in a doula program, and one was also participating in a lactation program. Two women told us they did not receive any information about programs related to their pregnancy, with one noting there are no programs for pregnant women at the jail. |
|
Postpartum care |
Two of the eight women we spoke with had already delivered their babies. Both told us that they received follow-up medical care at the jail; one also received follow-up care at the hospital and the other expected to receive follow-up care at the hospital in the future. One postpartum woman reported experiencing a postpartum condition that she said was not adequately addressed by medical staff at the jail; she intended to address the issue at her hospital follow-up appointment. |
|
Maternity clothing |
Six women said they received a special-colored uniform designated for pregnant women. Two women said they did not receive special maternity clothing; they received the standard uniform and could request a larger size. |
|
Bunk assignments |
All eight women said they had a lower bunk assignment while pregnant. |
|
Prenatal vitamins |
All eight women said they received prenatal vitamins while pregnant. |
|
Nutrition |
Six women told us they received extra portions of protein at meals while pregnant. Two women told us they did not regularly receive extra portions at meals. None of the women told us they received snacks. Four women told us they received bottled water at the jail. |
|
Restrictive housin
|
Six women told us they were not placed in restrictive housing while pregnant at the jail. Two women were isolated from others at the facility at some point during their pregnancies. One woman said she was placed in disciplinary segregated housing for 28 days. One woman said the jail isolated her from others for the first month because of her case type (but did not further specify). |
|
Restraints |
Six women said they were not placed in restraints during their pregnancies. Two women told us they were placed in restraints at some point during their pregnancies. Of these two women, one said she was initially handcuffed to the bed at the hospital during early labor but was released from the restraints after being admitted. One woman said she was handcuffed both before and after she knew she was pregnant. |
|
Requests for additional care |
Five women stated that there was not a particular medical or mental health service that they requested during their pregnancies or postpartum periods that they did not receive. One woman said she had a postpartum condition and feels her concerns were not appropriately addressed by jail medical staff; she planned to bring it up at her follow-up appointment at the hospital. One woman said it took a while for her requested mental health care to be scheduled. Another woman said that she has asked for counselors from outside the facility to come to the jail more frequently. |
Source: GAO analysis of interviews with pregnant and postpartum women incarcerated in two local jails. | GAO‑25‑106404
Notes: We interviewed six pregnant and two postpartum women at two local jails in June 2023 and September 2023. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as the racial and ethnic breakdown of the population under the jurisdiction of state and federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities, among other factors. We asked officials at these jails to identify pregnant women and women who had given birth while incarcerated. The jail officials identified these women and asked for volunteers to meet with us. Although these interviews are not generalizable and may not be indicative of the care provided at all local jails, they provided us with perspectives on the care provided to pregnant women. We did not independently verify statements made by these eight women we interviewed.
aA doula is a trained professional who provides physical, emotional, and informational support before, during and shortly after childbirth.
GAO Contact
Gretta L. Goodwin at (202) 512-8777 or GoodwinG@gao.gov
Staff Acknowledgments
In addition to the contact named above, Meg Ullengren (Assistant Director), Stephanie Heiken (Analyst-in-Charge), Charlotte Gamble, Kathryn Lenart, Nira Marte, and Sarah Turpin made key contributions to this report. Nasreen Badat, Willie Commons III, Karen Doren, Eric Hauswirth, Gabriel Jimenez-Barron, Ying (Sophia) Liu, Jeanne Murphy-Stone, Patricia Powell, Janet Temko-Blinder, and Sirin Yaemsiri also contributed to this report.
GAO’s Mission
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]Maternal mortality refers to the death of a woman during pregnancy, at delivery, or soon thereafter. According to the World Health Organization, a maternal death is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. Maternal deaths are assigned to code numbers A34, O00–O95, and O98–O99 of the International Classification of Disease, 10th Revision. Maternal deaths may include those identified solely based on the pregnancy checkbox on the death certificate when no other pregnancy information is provided in the cause-of-death statement. A recent article by Joseph et al. suggested that these checkbox-only deaths should not be included in the definition of maternal mortality counts. See K.S. Joseph, et al., “Maternal Mortality in the United States: Are the High and Rising Rates Due to Changes in Obstetrical Factors, Maternal Medical Conditions, or Maternal Mortality Surveillance?” American Journal of Obstetrics and Gynecology, vol. 230, no. 4 (2024). The National Center for Health Statistics, the agency that produces national vital statistics, has previously noted that maternal deaths may be overcounted or undercounted in the U.S. and has taken steps to minimize overcounting of maternal deaths with women of older ages.
[2]GAO, Maternal Health: HHS Should Improve Assessment of Efforts to Address Worsening Outcomes, GAO‑24‑106271 (Washington, D.C.: Feb. 21, 2024). We use the term “women” in this report based on definitions in data sources but acknowledge this term does not include all people who may become pregnant, such as people who do not identify as either male or female, and some transgender men.
[3]Helen Fair and Roy Walmsley, “World Female Imprisonment List, Fifth Edition,” Institute for Crime & Justice Policy Research, (2022), accessed Apr. 30, 2024, https://www.icpr.org.uk/theme/prisons‑and‑use‑imprisonment/world‑prison‑brief.
[4]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Medical Problems Reported by Prisoners: Survey of Prison Inmates, 2016 (Washington, D.C.: June 2021) and U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Medical Problems of Jail Inmates (Washington, D.C.: Nov. 2006); BJS collected data for these reports in 2016 and 2002, respectively.
[5]According to BJS data, while approximately 11,100 women were incarcerated in federal prisons in 2022, approximately 64,800 women were incarcerated in state prisons. An additional 92,900 women were incarcerated in local jails. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Prisoners in 2022 – Statistical Tables (Washington, D.C.: Nov. 2023); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Jail Inmates in 2022 – Statistical Tables (Washington, D.C.: Dec. 2023).
[6]The White House, White House Blueprint for Addressing the Maternal Health Crisis (Washington, D.C.: June 2022).
[7]Maternal morbidity refers to unexpected outcomes of labor and delivery that result in short- or long-term consequences to a woman’s health.
[8]Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
[9]GAO, Immigration Detention: Care of Pregnant Women in DHS Facilities, GAO‑20‑330 (Washington, D.C.: Mar. 24, 2020).
[10]GAO, Pregnant Women in DOJ Custody: U.S. Marshals Service and Bureau of Prisons Should Better Align Policies with National Guidelines, GAO‑21‑147 (Washington, D.C.: Jan. 25, 2021). We made six recommendations in our 2021 report, four to the U.S. Marshals Service and two to the Bureau of Prisons (BOP) to take steps to more closely align their policies with national guidance on pregnancy-related care, and to require facilities to collect data on pregnant or postpartum women placed in restrictive housing, among other things. DOJ concurred with these recommendations. As of September 2024, the U.S. Marshals Service implemented three recommendations and partially addressed one recommendation; BOP addressed both recommendations. By fully implementing these recommendations, U.S. Marshals Service would have greater assurance that pregnant and postpartum women in their custody receive appropriate treatment and care.
[11]GAO, Maternal Mortality and Morbidity: Additional Efforts Needed to Assess Program Data for Rural and Underserved Areas, GAO‑21‑283 (Washington, D.C.: Apr. 8, 2021; GAO, Maternal Health: Outcomes Worsened and Disparities Persisted During the Pandemic, GAO‑23‑105871 (Washington, D.C.: Oct. 19, 2022); and GAO‑24‑106271. In our 2021 report we made three recommendations, including that relevant HHS agencies disaggregate and review data by rural and underserved areas, and that HHS establish a formal coordinated approach for monitoring maternal health efforts. HHS concurred with our recommendations and implemented them. Implementing these recommendations should better position HHS to help ensure that program funding is being used to help address any needs in these areas and to understand the extent to which its programs are helping to reach its goals. We made two recommendations in our 2024 report including that HHS should include key performance management processes to assess the performance of the agency’s maternal health efforts against the blueprint’s goals. HHS concurred with our recommendations. As of September 2024, HHS has not yet addressed the recommendations from our 2024 report. By implementing these recommendations, HHS would be able to measure the performance of its programs and their effect on maternal health outcomes.
[12]We interviewed officials in the following states: Alabama, Arizona, California, Georgia, Illinois, Louisiana, New Jersey, New York, North Carolina, Ohio, Tennessee, and Texas.
[13]We reviewed the most recent data available from the U.S. Department of Justice’s Bureau of Justice Statistics from the following reports: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Correctional Populations in the United States, 2015 (Washington, D.C.: Dec. 2016); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Census of Jails, 2005-2019 – Statistical Tables (Washington, D.C.: Oct. 2021); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Prisoners in 2021 – Statistical Tables (Washington, D.C.: Dec. 2022).
[14]We conducted in-person visits in California, Ohio, and Texas. To select these three states, we chose one state with a relatively high female incarceration rate, one with a mid-level rate, and one with a low rate. We reviewed the most recent data available from the U.S. Department of Justice’s Bureau of Justice Statistics. See U.S. Department of Justice, Correctional Populations in the United States, 2015. Because we planned to speak with incarcerated pregnant and postpartum women during these site visits, we selected states that had relatively higher numbers of women under the jurisdiction of state correctional authorities and incarcerated in local jails. We reviewed the most recent data available from the U.S. Department of Justice’s Bureau of Justice Statistics. See U.S. Department of Justice, Prisoners in 2021 and U.S. Department of Justice, Census of Jails, 2005-2019.
[15]These datasets included the Healthcare Cost and Utilization Project, Pregnancy Risk Assessment Monitoring System, the National Vital Statistics System, Pregnancy Mortality Surveillance System, and Maternal Mortality Review Information Application. The Healthcare Cost and Utilization Project is a collection of healthcare databases developed through a federal-state-industry partnership. These databases contain data about hospital care in the U.S. The Pregnancy Risk Assessment Monitoring System collects data on maternal attitudes and experiences before, during, and shortly after pregnancy. The births in the jurisdictions participating in in this effort represent approximately 81 percent of all live births in the U.S. The National Vital Statistics System is an intergovernmental data sharing system which collects and disseminates data on vital statistics—including births and deaths—across the U.S. The Pregnancy Mortality Surveillance System is a national surveillance system of pregnancy-related deaths. Maternal Mortality Review Committees convene at the state or local level to review deaths during or within a year of pregnancy to determine whether deaths were pregnancy-related and share this data with HHS through the Maternal Mortality Review Information Application.
[16]These nongovernmental organizations included the American College of Obstetricians and Gynecologists (ACOG), Advocacy and Research on Reproductive Wellness of Incarcerated People, the Ostara Initiative, the Texas Jail Project, and the Women & Justice Project. ACOG is a professional membership organization for obstetrician-gynecologists which has issued a committee opinion on reproductive health care for incarcerated individuals. Advocacy and Research on Reproductive Wellness of Incarcerated People is a research group which conducted the Pregnancy in Prison Statistics—a nongeneralizable study on pregnancy outcomes in prison and jails nationwide. The Ostara Initiative provides support services to pregnant and parenting individuals across nine state prisons and local jails in Minnesota and Alabama. The Texas Jail Project monitors, documents, and reports on jail conditions in Texas jails; it also advises lawmakers on jail issues in the state. The Women & Justice Project works with currently and formerly incarcerated women to advocate for changes to the criminal legal system.
[17]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Census of State and Federal Adult Correctional Facilities, 2019 – Statistical Tables (Washington, D.C.: Nov. 2021); and U.S. Department of Justice, Census of Jails, 2005-2019. As of 2019, there were 1,155 public state prisons and 411 private prisons which incarcerated individuals under state correctional authorities. As of 2019, there were 3,116 total jail facilities in the U.S. and 34 of those were private jails.
[18]As of 2019, there were 217 public state prisons and 211 private prisons which incarcerated women under state correctional authorities, according to BJS.
[19]Of the total 110,510 women in jail custody in 2019, 1,800 women were in private jails.
[20]An example of other state-level bodies with an oversight role is the Texas Commission on Jail Standards, which is the regulatory and enforcement agency for all county jails and privately operated municipal jails in Texas.
[21]According to BJS, the decline in the overall incarcerated population resulted from both a reduction in admissions to carceral facilities and expedited releases in response to the COVID-19 pandemic, generally during the period of March to June 2020. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Impact of COVID-19 on State and Federal Prisons, March 2020-February 2021 (Washington, D.C: Aug. 2022); and U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Impact of COVID-19 on the Local Jail Population, January-June 2020 (Washington, D.C.: Mar. 2021).
[22]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, National Prisoner Statistics, [United States], 1978-2022 (ICPSR 38871), Inter-university Consortium for Political and Social Research [distributor], accessed June 6, 2024, https://www.icpsr.umich.edu/web/NACJD/studies/38871; U.S. Department of Justice, Jail Inmates in 2022-Statistical Tables; U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Jail Inmates in 2017 (Washington, D.C.: Apr. 2019).
[23]Specifically, in 2022, the number of women in state prisons was at 80 percent of pre-pandemic levels and the number of women in local jails was at 84 percent of pre-pandemic levels. From 2020 through 2022, the number of women in state prisons increased by 5 percent and the number of women in local jails increased by 21 percent.
[24]Estelle v. Gamble, 429 U.S. 97, 104 (1976).
[25]Brown v. Plata, 563 U.S. 493 (2011).
[26]American College of Obstetricians and Gynecologists is a professional membership organization for obstetrician–gynecologists; it issues policy and position statements related to the field of obstetrics and gynecology, including guidance on health care for incarcerated women. The American Correctional Association is a professional membership organization for individuals or groups in corrections. The National Commission on Correctional Health Care is an independent nonprofit organization that publishes standards for health services in correctional facilities in addition to other resources. Both the American Correctional Association and the National Commission on Correctional Health Care offer accreditation to correctional facilities that can demonstrate they meet their respective recommended standards.
[27]U.S. Department of Justice, Medical Problems Reported by Prisoners; and U.S. Department of Justice, Medical Problems of Jail Inmates. BJS collected data for these reports in 2016 and 2002, respectively. These are the most recent BJS data available regarding pregnancy in state prisons and local jails.
[28]U.S. Department of Justice, Medical Problems Reported by Prisoners; examples of other forms of prenatal care specified in the report include instructions on childcare, a special diet, medication, or special testing from a medical provider. In this report, BJS noted that there were approximately 89,200 women in state prison in 2016, at the time of data collection.
[29]U.S. Department of Justice, Medical Problems of Jail Inmates; examples of other forms of prenatal care specified in the report include instructions on childcare, exercises, a special diet, medication, or special testing from a medical provider. In another report that used 2002 BJS data, BJS stated that there were approximately 77,400 women in local jails in 2002, at the time of data collection. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Prison and Jail Inmates at Midyear 2002 (Washington, D.C.: Apr. 2003).
[30]According to BJS officials, BJS collects demographic information in its national sample surveys but does not report it for incarcerated pregnant women in state prisons and local jails due to the relatively small population and potential for unreliable estimates.
[31]The Joint Explanatory Statement, accompanying the Consolidated Appropriations Act, 2021, Pub. L. No. 116-260, 134 Stat. 1182 (Dec. 27, 2020), incorporates House Report 116-455, H.R. Rep. No. 116-455, at 95.
[32]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Data on Maternal Health and Pregnancy Outcomes from Prisons and Jails: Results from a Feasibility Study (Washington, D.C.: Jan. 2024).
[33]These recommendations include (1) collect information on maternal healthcare practices and data elements commonly available in case management systems; (2) prioritize collecting aggregate-level data over individual-level data; (3) prioritize supplemental over new stand-alone data collections; (4) employ established methods to maximize response rates; and (5) assess the need to obtain maternal health data from Indian country jails and private facilities.
[34]As of May 2024, BJS told us it has not yet developed plans to implement a similar data collection effort from jails. These officials said they conducted the necessary work during the feasibility study to collect similar data from local jails, but that resource considerations will determine whether they will be able to test and administer an instrument to collect data from local jails.
[35]Pregnancy outcomes refer to how pregnancies are completed, including live births, pre-term births, miscarriages, and ectopic pregnancies, among other outcomes. According to BJS officials, the survey of state DOCs will request information on maternal health and pregnancy outcomes between January 1, 2023, and December 31, 2023, including the annual count of female admissions to prison tested for pregnancy, the number of those tests that were positive, and the number of pregnancy outcomes by outcome type. Additionally, the survey will request information about maternal health services and accommodations among state DOCs and provide a 1-day count (December 31, 2023) of pregnant women by race/Hispanic origin, and the number of women residing in a nursery program.
[36]However, BJS reported in its maternal health feasibility study that some facilities do not use electronic health records. BJS also found that this information was often maintained in the form of handwritten notes, PDFs, and paper charts at some facilities.
[37]Generally, jails do not regularly report information or data to state DOCs.
[38]The Health Insurance Portability and Accountability Act of 1996, Pub. L. No. 104-191, 110 Stat. 1936 (commonly known as “HIPAA”) protects the privacy of individually identifiable health information and includes limitations on data sharing.
[39]In April 2024, the Health Resources and Services Administration (HRSA) announced a one-time funding opportunity for health centers funded by HRSA under section 330 of the Public Health Service Act, Pub. L. No. 78-410, 58 Stat. 682 (1944), as added by Pub. L. No. 104-299, § 2, 110 Stat. 3626, 3626-42 (1996) (codified as amended at 42 U.S.C. § 254b), to implement new approaches to support transitions in medical care for people leaving incarceration during the 90 days prior to their release to help them return to the community by expanding access to primary health care for these individuals, including mental health and substance use disorder treatment. Health centers can also use these funds to provide case management services to address issues these individuals face upon reentry into the community, such as housing and food insecurity, financial strain, access to transportation, and intimate partner violence.
[40]The Bureau of Justice Assistance supports state, local, and tribal governments, and the community-based organizations they partner with, to achieve safer communities. The Bureau of Justice Assistance administers grants and provides training and technical assistance to its grant recipients and the field at-large, which may include grant programs that can be used to support maternal health care. The National Institute of Corrections is an agency within BOP which provides training, technical assistance, information services, and policy and program development assistance to federal, state, and local corrections agencies. It also provides guidance regarding correctional policies, practices, and operations nationwide in areas of emerging interest and concern.
[41]HHS does not know the specific amount of money recipients of these 23 grant awards spent providing assistance for maternal health care in state prisons and local jails because their awards could be used by recipients to support additional types of services in other locations beyond providing that care. Two other grant programs—the Community Services Block Grant program, the Social Services Block grant program—do not report data about their use of funds on a level that would allow us to identify whether award funds were being used to support maternal health care in prisons and jails. According to HRSA officials, recipients of the Title V Maternal and Child Health Services Block Grant program must match the funding provided by the grant with state funds. The activities that recipients report funding to HHS may be accomplished with the grant funds, state matching funds, or through a partnership with other agencies and entities. Further, Title V Maternal and Child Health Services Block Grant recipients report to HRSA annually on how the state’s Title V program is addressing a specific Maternal and Child Health topic. State recipients may or may not choose to highlight how their programs support care for incarcerated pregnant and postpartum women. As such, there may be more states that use funds for this purpose that are not included in this report.
[42]Healthy Start Initiative and Head Start and Early Head Start grant programs use solicitations. The Community Services Block Grant program does not use solicitations because it is a formula grant program and HHS provides awards directly to the states. The Social Services Block Grant program uses action transmittals for states to apply for funding, wherein states make a case for their needs. The Title V Maternal and Child Health Services Block Grant program does not use solicitations because it is a formula grant program. States apply for funds each year and provide their annual report by completing the grant program’s guidance materials. We reviewed the grant program guidance and did not find any indication that funds may be used to provide maternal health care for incarcerated women in prisons and jails specifically, but the guidance does indicate that states may collaborate on programs with other governmental agencies, including corrections agencies.
[43]From fiscal year 2018 through 2023, the Healthy Start Initiative issued two solicitations; we reviewed both solicitations. According to HHS officials, HHS issues Head Start and Early Head Start competitive solicitations by specific service area. As such, there were 480 Head Start and Early Head Start solicitations from fiscal year 2018 through fiscal year 2023. We reviewed three competitive solicitations that resulted in awards that are being used to provide maternal health care for incarcerated women in prisons and jails.
[44]Department of Health and Human Services, Addressing the Maternal Health Crisis in the United States: An Update from the U.S. Department of Health and Human Services (Washington, D.C.: Jul. 2024).
[45]Officials representing the ninth prison and ninth jail did not indicate whether they follow guidance from professional organizations at their facilities.
[46]In prior GAO work on pregnant women in federal immigration detention facilities and federal prisons, we identified and reported on several different services and types of care that pregnant and postpartum women may receive at federal facilities. See GAO‑20‑330 and GAO‑21‑147.
[47]Carolyn Sufrin and Committee on Health Care for Underserved Women, “Reproductive Health Care for Incarcerated Pregnant, Postpartum, and Nonpregnant Individuals: ACOG Committee Opinion, Number 830,” Obstetrics and Gynecology, vol. 138, no.1 (July 2021). As stated previously, officials representing eight of nine prisons and eight of nine jails we met with reported following guidance from one or more professional organizations.
[48]Examples of medications for opioid use disorder include methadone and buprenorphine.
[49]Officials representing the ninth prison reported that they provide nutritional services to pregnant women but did not specify the nature of these services.
[50]Officials representing one of nine jails did not provide details on the arrangement they use to provide health care at their facility.
[51]If a woman is excluded from the count of pregnant and postpartum women who described receiving a specific service or type of care, it does not necessarily mean that the woman did not receive that service or type of care. Instead, it may mean that she did not mention receiving this service or type of care to us. Additionally, we did not independently verify which services or types of care that the women we met with actually received.
[52]We did not conduct a comprehensive review of state laws pertaining to maternal health care in prisons and jails for all 50 states or independently determine whether prisons and jails we met with followed the laws applicable to their states.
[53]The officials we met with represented prisons and jails located across 12 states, all of which have state laws addressing the use of restraints on pregnant and postpartum women.
[54]Officials representing another jail noted that a support person may include a doula, partner, family member, or friend.
[55]CenteringPregnancy is a program for prenatal care developed in the 1990s and available at sites across the country. Participants in the program join groups of eight to 10 pregnant women with similar due dates. In addition to private medical assessments, each prenatal appointment that participants attend incudes a collective group session led by the medical provider and their staff, who facilitate discussion and lead activities on topics related to pregnancy and infant care.
[56]According to officials representing one jail, state law in one of the states where one of these prisons and one of these jails are located entitles women to a support person during delivery.
[57]Officials representing the three prisons and one jail that operate nursery programs reported that women must meet eligibility criteria to participate. According to officials representing the three prisons and one jail that operate a nursery program, typical disqualifying factors include convictions for violent crimes or crimes against children. Officials representing the three prisons with nursery programs indicate that the maximum length of stay ranges from 18 to 36 months and participants must conclude their sentences within those maximum lengths of stay. For the one nursery program operated by a jail, officials reported that children of participants may stay for up to 1 year, at which point they must enter kinship or foster care if their mothers remain incarcerated.
[58]According to OJP’s National Institute of Justice, reentry refers to the transition from life in jail or prison to life in the community.
[59]The federal government does not have a role in operating state prisons and local jails. The five NGOs we met with were ACOG, Advocacy and Research on Reproductive Wellness of Incarcerated People, the Ostara Initiative, the Texas Jail Project, and Women & Justice Project.
[60]We reviewed 33 articles that discussed at least one challenge to providing maternal health care to incarcerated women or at least one opportunity to address these challenges. We use “articles” to refer to all the sources we reviewed, which included both nongeneralizable studies and commentaries by researchers published in peer reviewed journals or from professional organizations, such as ACOG. Not all articles address the same topics related to the challenges and opportunities of providing maternal health care in prisons and jails.
[61]Chris Ahlbach, Carolyn Sufrin, and Rebecca Shlafer, “Care for Incarcerated Pregnant People with Opioid Use Disorder: Equity and Justice Implications,” Obstetrics and Gynecology, vol. 136, no.3 (Sept. 2020).
[62]None of the officials we met with representing any of the nine prisons or nine jails told us they charged a copayment for health services. Additionally, none of the 27 pregnant and postpartum women we met with told us they made a copayment for any care that they received while in custody.
[63]Sufrin and Committee on Health Care for Underserved Women, “Reproductive Health Care for Incarcerated Pregnant, Postpartum, and Nonpregnant Individuals.” None of these articles were studies which indicated how frequently facilities charge copayments.
[64]Karissa Rajagopal et al., “Reproductive Health Care for Incarcerated People: Advancing Health Equity in Unequitable Settings,” Clinical Obstetrics and Gynecology, vol. 66, no. 1 (Mar. 2023).
[65]Alicia Suarez, “‘I Wish I Could Hold Your Hand’: Inconsistent Interactions Between Pregnant Women and Prison Officers,” Journal of Correctional Health Care, vol. 27, no.1 (Nov. 2021).
[66]Zoe King et al., “Access to Treatment for Pregnant Incarcerated People with Opioid Use Disorder: Perspectives from Community Opioid Treatment Providers,” Journal of Substance Abuse Treatment, vol. 126 (Feb. 2021); Lorie S. Goshin et al., “Stigma and US Nurses' Intentions to Provide the Standard of Maternal Care to Incarcerated Women,” American Journal of Public Health vol. 110, no. S1 (2020).
[67]Researchers measured stigmatizing attitudes toward incarcerated pregnant women by asking participants to rate their agreement with a series of statements on topics including substance use, shackling, fearfulness when providing care to incarcerated pregnant women, and comparing incarcerated and nonincarcerated pregnant women.
[68]Rajagopal et al., “Reproductive Health Care for Incarcerated People.”
[69]Susan Hatters Friedman, Aimee Kaempf, and Sarah Kauffman, “The Realities of Pregnancy and Mothering While Incarcerated,” The Journal of the American Academy of Psychiatry and the Law, vol. 48, no. 3 (2020).
[70]One article recommending that facilities standardize maternal health care practices was ACOG’s committee opinion on reproductive health care for incarcerated women, which outlines standards they recommend all facilities adopt.
[71]Suarez, “‘I Wish I Could Hold Your Hand.’”
[72]Twelve of the 33 articles that we reviewed discussed how restraints can complicate the provision of maternal health care or harm a pregnant woman or unborn fetus. The complications that the articles described include how restraints can interfere with a medical provider’s ability to assess and treat a pregnant woman, especially in emergencies. Potential harms that the articles described include difficulty breaking a fall while restrained, which could result in injuries to the woman or the fetus.
[73]Smriti Nair, et al., “Pregnancy in Incarcerated Women: Need for National Legislation to Standardize Care,” Journal of Perinatal Medicine, vol. 49, no. 7 (June 2021).
[74]We use the term “women” in this report based on definitions in data sources but acknowledge this term does not include all people who may become pregnant, such as people who do not identify as either male or female, and some transgender men.
[75]We reviewed the most recent data available from the U.S. Department of Justice’s Bureau of Justice Statistics from the following reports: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Correctional Populations in the United States, 2015 (Washington, D.C.: Dec. 2016); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Census of Jails, 2005-2019 – Statistical Tables (Washington, D.C.: Oct. 2021); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Prisoners in 2021 – Statistical Tables (Washington, D.C.: Dec. 2022).
[76]We considered states with relatively high incarceration rates to be those states with the 16 highest female incarceration rates, those with mid-level rates to be those states with the middle 19 rates, and those with low rates to be those states with the 15 lowest rates. We considered states with relatively high numbers of women under the jurisdiction of state correctional authorities to be those 15 states with the most women under the jurisdiction of state correctional authorities. We considered states with relatively high numbers of women incarcerated in local jails to be those 15 states with the most women incarcerated in local jails.
[77]Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
[78]Centers for Disease Control and Prevention, National Center for Health Statistics, Maternal Mortality Rate by State, 2018-2021 (Washington, D.C.).
[79]We reviewed the following report for racial and ethnic data for the population under the jurisdiction of state and federal correctional authorities: U.S. Department of Justice, Prisoners in 2021.
[80]U.S. Census Bureau, Census Regions and Divisions of the United States (Washington, D.C.: Oct. 8, 2021), accessed Apr. 26, 2023.
[81]After using these factors to select an initial sample of 10 states, we compared these 10 states to a list of states with the highest percentages of sentenced individuals whose most serious offense was drug-related from the Bureau of Justice Statistics (BJS) and a list of states with the highest homeless populations from the National Alliance to End Homelessness. The team ensured that the sample included states ranked in the top half of all states for each of these lists. We considered these criteria because vulnerable populations such as those who have substance use disorder or those who were homeless prior to incarceration may require additional maternal health care services.
[82]U.S. Department of Justice, Correctional Populations in the United States, 2015.
[83]U.S. Department of Justice, Prisoners in 2021; U.S. Department of Justice, Census of Jails, 2005-2019.
[84]At two facilities, we also met with representatives from a community or local government program that provided maternal health care services at these facilities.
[85]Some of the women we met with who were participating in nursery programs may have been more than 3 months postpartum.
[86]We deemed international articles relevant if they included information on studies of state prisons and local jails in the U.S. or discussed U.S. facilities specifically.
[87]The Healthcare Cost and Utilization Project, managed by the Agency for Healthcare Research and Quality, is a collection of healthcare databases developed through a federal-state-industry partnership. These databases contain data about hospital care in the U.S. The Pregnancy Risk Assessment Monitoring System, managed by the Centers for Disease Control and Prevention, collects data on maternal attitudes and experiences before, during, and shortly after pregnancy. The births in the jurisdictions participating in this effort represent approximately 81 percent of all live births in the U.S. The National Vital Statistics System, also managed by the Centers for Disease Control and Prevention, is an intergovernmental data sharing system which collects and disseminates data on vital statistics—including births and deaths—across the U.S. The Pregnancy Mortality Surveillance System, managed by the Centers for Disease Control and Prevention, is a national surveillance system of pregnancy-related deaths. Maternal Mortality Review Committees convene at the state or local level to review deaths during or within a year of pregnancy to determine whether deaths were pregnancy-related and share these data with the Centers for Disease Control and Prevention through the Maternal Mortality Review Information Application.
[88]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Medical Problems of Jail Inmates (Washington, D.C.: Nov. 2006) and U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Medical Problems Reported by Prisoners: Survey of Prison Inmates, 2016 (Washington, D.C.: June 2021).
[89]U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. Data on Maternal Health and Pregnancy Outcomes from Prisons and Jails: Results from a Feasibility Study (Washington, D.C.: Jan. 2024).
[90]The Grants Management System is the legacy system used by DOJ’s Office of Justice Programs (OJP) to track and manage awards throughout the grant life cycle. In October 2020, OJP began using a new grants management system called JustGrants.
[91]According to ACF officials, Head Start and Early Head Start grant award funds can be used to support maternal health care in state prisons and local jails. The Head Start and Early Head Start grant program seeks to increase the number of low-income children receiving high-quality, comprehensive early education services and pregnant persons receiving high-quality prenatal and postpartum services.
[92]According to HRSA officials, Healthy Start grant award funds can be used to support maternal health care in state prisons and local jails. The Healthy Start grant program seeks to reduce rates of infant death, improve maternal health outcomes, and reduce racial and ethnic disparities.
[93]According to HRSA officials, Title V Maternal and Child Health Block Grant program award funds can be used to support maternal health in state prisons and local jails. The Title V Maternal and Child Health Block Grant program seeks to improve public health systems for mothers, children, and their families, including by supporting children and youth with special health care needs.
[94]The 10 DOJ grant programs are the Adult Drug Court Discretionary Grant Program, Comprehensive Opioid, Stimulant, and Substance Abuse Site-Based Program, Improving Adult and Juvenile Crisis Stabilization and Community Reentry Program, Residential Substance Abuse Treatment Program, Second Chance Act: Community-based Reentry Program, Second Chance Act: Improving Reentry Education and Employment Outcomes Program, Second Chance Act: Improving Substance Use Disorder Treatment and Recovery Outcomes for Adults in Reentry Program, Second Chance Act: Pay for Success Program, Second Chance Act: Smart Reentry, and Second Chance Act: Statewide Adult Recidivism Reduction Program.
[95]The five HHS grant programs are Healthy Start Initiative, Head Start and Early Head Start grant program, Community Services Block Grant program, Social Services Block Grant program, and Title V Maternal and Child Health Services Block Grant program. Healthy Start Initiative and Head Start and Early Head Start grant programs use solicitations. The Community Services Block Grant program does not use solicitations because it is a formula grant program and HHS provides awards directly to the states. The Social Services Block Grant program uses action transmittals for states to apply for funding, wherein states make a case for their needs. The Title V Maternal and Child Health Services Block Grant Program does not use solicitations because it is a formula grant program. States apply for funds each year and provide their annual report by completing the grant program’s guidance materials. From fiscal year 2018 through 2023, the Healthy Start Initiative issued two solicitations; we reviewed both solicitations. According to HHS officials, HHS issues Head Start and Early Head Start competitive solicitations by specific service area. As such, there were 480 solicitations from fiscal year 2018 through fiscal year 2023. We reviewed three competitive solicitations HHS selected for us that resulted in awards that are being used to provide maternal health care for incarcerated women in prisons and jails.
[96]The White House, White House Blueprint for Addressing the Maternal Health Crisis (Washington, D.C.: June 2022).
[97]GAO, Immigration Detention: Care of Pregnant Women in DHS Facilities, GAO‑20‑330 (Washington, D.C.: Mar. 24, 2020) and GAO, Pregnant Women in DOJ Custody: U.S. Marshals Service and Bureau of Prisons Should Better Align Policies with National Guidelines, GAO‑21‑147 (Washington, D.C.: Jan. 25, 2021). Additionally, when speaking with officials from a state DOC, we asked if the state DOC had any policies or standards in place related to each service or type of care.
[98]We use the term “women” in this report based on definitions in data sources but acknowledge this term does not include all people who may become pregnant, such as people who do not identify as either male or female, and some transgender men.
[99]ACF promotes the economic and social well-being of families, children, youth, individuals and communities with funding, strategic partnerships, guidance, training, and technical assistance. HRSA works to improve health outcomes and achieve health equity through access to quality services, a skilled health workforce, and innovative, high-value programs.
[100]The Healthy Start Initiative grant program is intended to reduce rates of infant death, improve maternal health outcomes, and reduce racial and ethnic disparities. The Head Start and Early Head Start grant program seeks to increase the number of low-income children receiving high-quality, comprehensive early education services and pregnant persons receiving high-quality prenatal and postpartum services. The Title V Maternal and Child Health Services Block Grant program works to improve public health systems for mothers, children, and their families. This includes support for children and youth with special health care needs. According to HRSA officials, recipients of the Title V Maternal and Child Health Services Block Grant program must match the funding provided by the grant with state funds. The activities that recipients report funding to HHS may be accomplished with the grant funds, state matching funds, or through a partnership with other agencies and entities. Further, Title V Maternal and Child Health Services Block Grant recipients report to HRSA annually on how the state’s Title V program is addressing a specific Maternal and Child Health topic. State recipients may or may not choose to highlight how their programs support care for incarcerated pregnant and postpartum women. As such, there may be more states that use funds for this purpose that are not included in this report.
[101]We reviewed the most recent data available from the U.S. Department of Justice’s Bureau of Justice Statistics from the following reports: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Correctional Populations in the United States, 2015 (Washington, D.C.: Dec. 2016); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Census of Jails, 2005-2019 – Statistical Tables (Washington, D.C.: Oct. 2021); U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, Prisoners in 2021 – Statistical Tables (Washington, D.C.: Dec. 2022).
[102]Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth.
[103]GAO, Immigration Detention: Care of Pregnant Women in DHS Facilities, GAO‑20‑330 (Washington, D.C.: Mar. 24, 2020) and GAO, Pregnant Women in DOJ Custody: U.S. Marshals Service and Bureau of Prisons Should Better Align Policies with National Guidelines, GAO‑21‑147 (Washington, D.C.: Jan. 25, 2021).
[104]We use the term “women” in this report based on definitions in data sources but acknowledge this term does not include all people who may become pregnant, such as people who do not identify as either male or female, and some transgender men. We did not independently verify statements made by the women we interviewed or assess prison compliance with policies based on these statements. We met with pregnant and postpartum women during our site visits to two state prisons in September 2023 and November 2023 and two local jails in June 2023 and September 2023. To develop our sample, we considered state rates and counts of incarcerated females and state maternal mortality rates, as well as the racial and ethnic breakdown of the population under the jurisdiction of state and federal correctional authorities. We also considered whether we were aware of any federal funding serving this population, diversity of geographic location, and the availability of nursery and doula programs in prison or jail facilities. Doulas are trained professionals who provide physical, educational, and emotional support and advocate for mothers before, during, and shortly after childbirth. We asked officials at these prisons and jails to identify pregnant women and women who had given birth while incarcerated. The prison and jail officials identified these women and asked for volunteers to meet with us. With the consent of these women, we conducted semi-structured interviews to obtain insight into the care they received at their respective prisons and jails. The women participating in the nursery programs also discussed their treatment and care in the nursery programs. While the perspectives of the women we interviewed cannot be generalized to all treatment and care provided at the prisons we visited, they provided us with helpful insights on pregnancy-related care.
