MILITARY HEALTH CARE
Departments Should Update Policies for Providers in Operational Settings Like Field Hospitals and Aircraft Carriers
Report to Congressional Committees
United States Government Accountability Office
View GAO‑25‑106445. For more information, contact Sharon M. Silas at (202) 512-7114 or silass@gao.gov.
Highlights of GAO‑25‑106445, a report to congressional committees
Departments Should Update Policies for Providers in Operational Settings Like Field Hospitals and Aircraft Carriers
Why GAO Did This Study
DOD health care providers deliver care in settings where military operations take place. These operational settings include hospital ships, field hospitals, and aircraft carriers. Providers go to these settings—usually from DOD’s military medical treatment facilities—to provide critical health care services, such as trauma care for service members with battle injuries and civilian care during humanitarian missions. DOD military departments—Navy, Air Force, and Army—are responsible for ensuring providers in operational settings are qualified and competent to provide safe, quality care. This is part of DOD’s overall effort to assure clinical quality across the military health system.
House Report 117-397 accompanying the National Defense Authorization Act for Fiscal Year 2023 includes a provision for GAO to review how the military departments ensure provider quality in operational settings. GAO examined military departments’ progress in updating relevant policies, among other issues.
GAO reviewed policy documents and provider records and interviewed officials from the military departments and DOD’s Defense Health Agency.
What GAO Recommends
GAO is making three recommendations, one to each military department to issue, as soon as possible, updated policies on privileging and evaluating providers in operational settings. DOD concurred with all three recommendations and stated that the military departments are currently revising and updating their relevant policies.
What GAO Found
The military departments are to “privilege” health care providers (i.e., review a provider’s qualifications and grant permission to deliver specific health care services) for operational settings. Once privileged, providers should have professional performance and competence routinely evaluated.
In July 2023, a Department of Defense (DOD) instruction directed the military departments to align their policies for privileging and evaluating providers with other DOD guidance. GAO found that Navy, Air Force, and Army are in varying stages of updating and finalizing their policies to align with the July 2023 instruction; however, none have yet issued new policies. Navy and Air Force each have draft policies and are working to finalize and issue them. Navy expects to issue its policy by March 2025; Air Force has not specified a completion date. Army has just begun to update its policy, with no completion date specified.

GAO obtained information about the processes the military departments have been using for privileging and evaluating providers in operational settings. Both Navy and Air Force officials described processes for reviewing and accepting a provider’s existing privileges at a military medical treatment facility for use in operational settings. Navy and Air Force officials also each described regular evaluations of the providers’ delivery of care. Army could neither definitively describe its current processes for privileging providers nor a department-wide process for conducting provider evaluations. The July 2023 DOD instruction requires the military departments to have guidance for these processes.
Updating their policies to align with current guidance, per the July 2023 instruction, would help each department better manage clinical quality in operational settings. Ensuring providers are properly qualified and continue to perform in a professional, competent manner are critical aspects of meeting the health care needs of U.S. service members.
No table of contents entries found.
Abbreviations
|
DHA |
Defense Health Agency |
|
DOD |
Department of Defense |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
December 4, 2024
The Honorable Jack Reed
Chairman
The Honorable Roger Wicker
Ranking Member
Committee on Armed Services
United States Senate
The Honorable Mike Rogers
Chairman
The Honorable Adam Smith
Ranking Member
Committee on Armed Services
House of Representatives
The Department of Defense’s (DOD) military health system delivers critical health care services to service members and other beneficiaries in a range of settings, including operational settings. Operational settings—any setting outside of a military medical treatment facility—may be in place temporarily to meet the needs of a military mission. These settings often operate in unpredictable and rapidly evolving conditions. Further, these settings may be geographically remote, near combat zones, or in areas that have experienced natural disasters.
The military departments—Navy, Air Force, and Army—send health care providers into these settings to support the full range of military operations. The type of care delivered can range from first responder care to advanced medical care such as surgical procedures, depending on the clinical capabilities of the operational setting. Operational settings include hospital ships, aircraft carriers, aeromedical evacuation aircraft, and field hospitals.
Doctors and other health care providers who are qualified to deliver safe, quality care are central to DOD’s ability to ensure overall clinical quality within the military health system. To help ensure providers are qualified, DOD “privileges” providers—that is, reviews a provider’s qualifications and grants permission for the provider to perform certain health care services. Once privileged, DOD routinely evaluates providers to ensure continuing professional performance and competence.
The DOD component responsible for privileging and evaluating a provider depends on where the provider is stationed. DOD’s Defense Health Agency (DHA) manages this responsibility for providers at military medical treatment facilities. When a provider is in an operational setting, the military department in which they serve assumes responsibility for the duration of the provider’s assignment.
DHA issued a procedures manual in August 2019, which helped inform the military departments’ processes for managing clinical quality, including privileging and evaluating providers.[1] DOD issued an instruction in July 2023 directing the military departments to update their policies for managing clinical quality in operational settings to align with the DHA procedures manual. The DOD instruction did not specify a deadline for these updates.[2]
House Report 117-397 accompanying the National Defense Authorization Act for Fiscal Year 2023 includes a provision for GAO to review how the military departments ensure clinical quality in operational settings, including assessing their processes for provider privileging and clinical performance evaluations, among other things.[3] In this report, we
1. evaluate military departments’ progress updating policies for provider privileging and evaluations for operational settings, as instructed by DOD in July 2023;
2. describe how Navy privileges providers for and evaluates providers’ performance in operational settings;
3. describe how Air Force privileges providers for and evaluates providers’ performance in operational settings; and
4. describe how Army privileges providers for and evaluates providers’ performance in operational settings.
To evaluate military departments’ progress toward updating policies for provider privileging and clinical performance evaluations for operational settings, we reviewed each of the military departments’ actions taken to update their policies to align with the 2023 DOD instruction, as applicable.[4] We obtained documentation, including draft policies when available, and interviewed officials from each of the three military departments. We also interviewed officials from DHA.
To describe how the Navy, Air Force, and Army privilege providers for and evaluate providers’ performance in operational settings, we interviewed officials from the three military departments, U.S. Central Command, and DHA about the processes used to carry out these responsibilities.[5] We also reviewed the military departments’ past policies to provide additional context for these processes.
For illustrative examples of the military departments’ processes, we requested records for privileged providers who were temporarily assigned to five recent operational settings. We reviewed available records for 312 privileged providers.[6] These consisted of records for 162 providers in two Navy settings, 41 providers in one Air Force setting, and 109 providers in two Army settings. The military departments were unable to provide all requested documents for all 312 providers. According to officials in the military departments, some documentation could not be located or was unavailable due to challenges specific to the operational settings. For more information on our methodology for reviewing documentation of the processes for privileging and evaluating providers temporarily assigned to five selected operational settings, see appendix I.
We selected the operational settings based on the dates of recent deployments, which varied and ranged from December 2020 to January 2024. Three of the five selected operational settings (all Air Force and Army locations) were located within the U.S. Central Command area of responsibility.
We also reviewed records for 17 privileged providers permanently assigned to two Navy operational settings. According to Navy officials, the process Navy used to privilege these providers differs from the process used for temporary assignments; information about Navy privileging process for providers permanently assigned to the selected operational settings can be found in appendix II.
We conducted this performance audit from December 2022 to November 2024 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Health Care in Operational Settings
Military health care providers deliver a wide range of medical care in various operational settings. The level of care depends on the types of medical equipment and complexity of services that can be supported. For example, radiology and laboratory services may not be available. In addition, in these settings, providers may not have reliable access to the health care information systems used at military medical treatment facilities, according to DHA officials.
The medical care provided in operational settings includes
· treatment of disease and non-battle injuries—such as from physical training, falls, or vehicle accidents;
· trauma care for battle injuries, such as surgeries and stabilization for evacuation to a military medical treatment facility; and
· services to civilian patients during humanitarian missions across the world.
The Military Health System, Military Departments, and DHA
The military health system is a complex, integrated enterprise that has responsibility for health care delivery, combat medicine, medical education, public health, and medical research and development. See figure 1 for the organizational structure of the military health system, which includes the military departments and the Defense Health Agency.
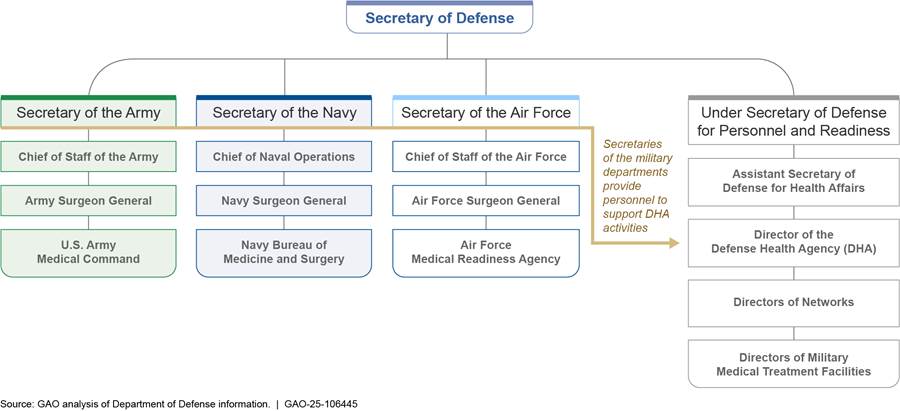
The military departments organize, train, and equip military forces—including medical personnel—as directed by the Secretary of Defense. Each military department’s surgeon general is responsible for developing and maintaining the readiness of providers to deliver health care to service members in both military medical treatment facilities and operational settings. Each military department maintains one or more organizational units that carry out this responsibility under the leadership of its surgeon general. These include the Navy’s Bureau of Medicine and Surgery, the Air Force Medical Readiness Agency, and the U.S. Army’s Medical Command.
DHA functions under DOD’s Under Secretary of Defense for Personnel and Readiness and is separate from the military departments.[7] DHA manages and administers military medical treatment facilities across the world and oversees health care delivery to active-duty service members and their family members. DOD transitioned the administration and management of health care delivery at military medical treatment facilities from the military departments to DHA between 2019 and 2022 in response to a statutory mandate to help streamline management and improve efficiency across the military health system. According to this mandate, DHA was to be responsible for the administration of each military medical treatment facility no later than September 30, 2021.[8] As a result, DHA is responsible for clinical care in military medical treatment facilities, including granting privileges to providers delivering clinical care in these settings.
The military departments retained responsibility for clinical care in operational settings.[9] As part of their responsibility for operational settings, the military departments are required to maintain policies on managing clinical quality, including processes for privileging and evaluating providers. In addition, the military departments are responsible for allocating providers and other personnel for duty at military medical treatment facilities and to operational settings.
DOD Processes for Privileging and Evaluating Providers
DHA issued a procedures manual in 2019 to outline key processes for managing clinical quality in the military health system. The DHA procedures manual includes requirements for aspects of provider privileging and evaluations in the military medical treatment facilities and in temporary duty assignments, which include deployments of providers from military medical treatment facilities to operational settings.
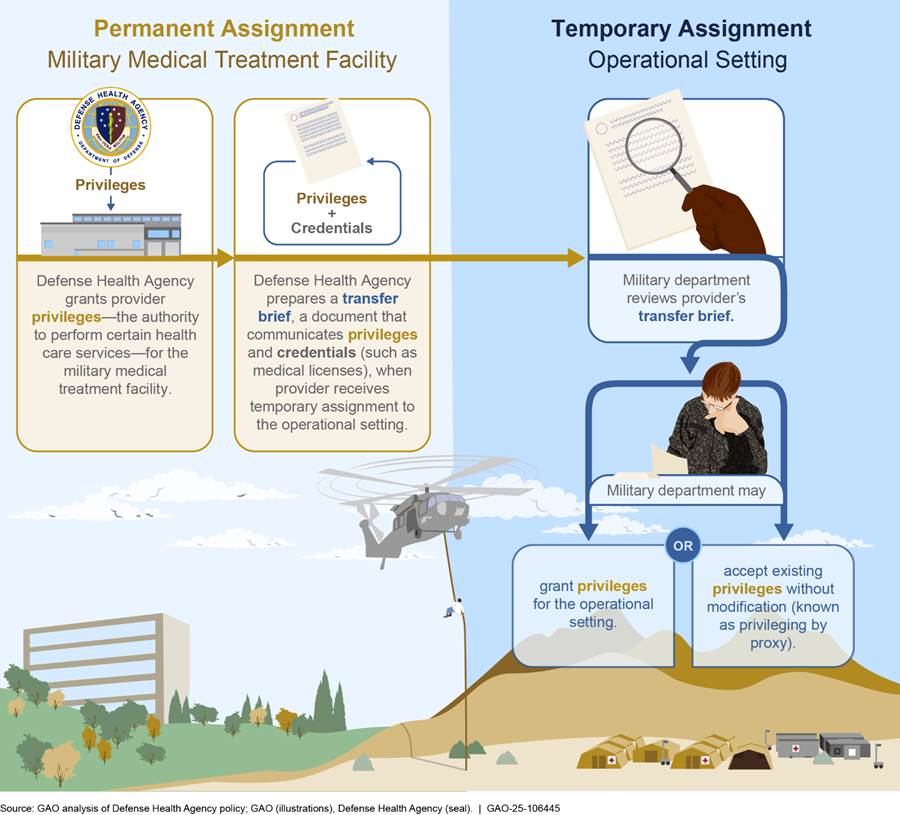
Privileging providers. A provider’s privileges define the scope and limits of their practice based on factors such as the health care setting they are serving in and the provider’s relevant training and experience. Generally, in military medical treatment facilities, privileging involves the review of a provider’s professional credentials—such as medical licenses—and qualifications necessary to grant permission for the provider to perform certain health care services. For example, before granting privileges, staff must verify the status of medical licenses, conduct queries of national databases that capture potentially adverse information about individual providers, and review assessments of provider performance. Officials designated as the privileging authority are responsible for deciding whether to grant privileges to providers, following their review and consideration of the locations’ capacities.
The DHA procedures manual outlines the two options that the military departments have for privileging providers for temporary assignments in the operational setting (see fig. 2). The military department may
· verify credentials and grant privileges to the provider for the operational setting; or
· accept the provider’s existing privileges granted by DHA at the military medical treatment facility where the provider is assigned—the provider’s home military medical treatment facility—without modification for the operational setting. This process—which allows a privileging authority to accept a provider’s privileges granted by another organization’s privileging authority—is known as privileging by proxy.
Evaluating providers. Provider evaluations assess a provider’s knowledge, skills, and ability to provide safe and effective care. Criteria for evaluation may include patient care, clinical knowledge, and interpersonal and communication skills. The DHA procedures manual requires ongoing evaluations every 6 months and an end-of-deployment evaluation following assignments to operational settings.[10] The military department determines the criteria included in its provider evaluations.
In July 2023, DOD issued a DOD instruction to further define the military departments’ roles and responsibilities related to health care delivery within the military health system. This included reiterating that responsibilities for privileging and evaluating providers in operational settings remain with the military departments. To carry out this responsibility, each military department surgeon general may delegate their privileging authority to an appropriate medical unit commander or other appropriate medical commanders.
The July 2023 instruction also specified that military departments should establish policies for operational settings that align with the DHA procedures manual to the extent practicable.[11] That is, the military departments should conduct such activities when it is practicable to do so given the challenges present in operational settings. For example, requirements for provider records to be uploaded to a centralized database during the provider’s deployment may not be practicable due to the inability to access such databases in certain operational settings, according to Air Force officials.
Military Departments Have Not Issued Updated Policies for Provider Privileging and Evaluations for Operational Settings
The military departments are in varying stages of updating and finalizing their policies to align with the July 2023 DOD instruction; however, as of August 2024, none have issued new policies. The July 2023 DOD instruction directs the military departments to establish guidance for managing clinical quality in operational settings consistent with DHA’s 2019 procedures manual. Such guidance, according to the DOD instruction, should outline the departments’ processes for privileging providers on temporary duty assignments to operational settings and the timing of provider evaluations during and following these assignments. The instruction also requires the military departments to document any deviations from the DHA procedures manual when the department determines a procedure to be impractical for operational settings.
The military departments have not issued updated policies for privileging and evaluating providers in operational settings since prior to 2016, when DOD began planning for its most recent reorganization of the military health system.[12] As such, the policies that exist do not reflect guidance DOD has since issued, in 2019 and 2023, to clarify roles and responsibilities for managing clinical quality in operational settings.
· Navy. Navy officials told us they began revising their policy in 2019 and will soon finalize and issue an updated policy.[13] Navy officials expect to release the military department’s updated comprehensive policy that covers providers in all operational settings by March 2025. Navy provided us with a copy of the draft policy, which is subject to revisions until final approval, according to Navy officials.[14]
· Air Force. Air Force’s efforts to update its policy are underway, but officials did not know when it would be issued. In the interim, the department issued a memorandum that states the DHA procedures manual supersedes military department policy in the case of any inconsistencies.[15] Air Force provided us with a copy of the early draft policy that, as of May 2024, is being revised.
· Army. Army officials told us in February 2024 that it planned to begin the process of updating its policies. Army’s efforts to date include convening a work group that met in June 2024. As of August 2024, Army officials have not specified a planned issuance date.
Officials from each of the military departments told us that they had awaited the DOD instruction—which was issued in July 2023—before updating and finalizing department policies. Air Force and Army officials told us they anticipated that the instruction would further clarify roles and responsibilities between the military departments and DHA for managing aspects of clinical quality, including privileging and evaluating providers. According to officials, this clarification was necessary given that some responsibilities were transferred to DHA while others were retained by the military departments during DOD’s significant recent reorganization. Navy officials told us that, though they began updating the department’s policies in 2019, the policies required additional revisions to comply with the DOD instruction.
As noted above, the military departments do not have policies that reflect current guidance for managing clinical quality in operational settings. Finalizing and issuing, as soon as possible, policies to align the military departments with the DOD instruction would help to ensure that the departments’ processes are consistently applied across operational settings and are, to the extent practicable, comparable to those implemented at military medical treatment facilities, as required. In addition, these policies could make clear any military department exceptions to this standardization—such as to accommodate the variability and challenges inherent to operational settings—as appropriate. Issuing these policies can help ensure that U.S. service members in operational settings are receiving care from providers with the necessary skills, training, and clinical competency.
Navy Accepts Existing Privileges for Providers Temporarily Assigned to Operational Settings and Evaluates Their Performance within These Settings
Navy officials described for us the department’s current process for privileging providers temporarily assigned to operational settings, which they said is based on the DHA procedures manual. Navy officials also described the department’s policies for evaluating providers in operational settings. According to Navy, requirements for privileging and provider evaluations will be included in the updated policies.
Navy Accepts Providers’ Privileges Granted by DHA When Providers Are Temporarily Assigned to Operational Settings
Navy’s existing process for privileging providers temporarily assigned to operational settings is based on the DHA procedures manual, and Navy plans to reflect this process in the updated policy when issued, according to Navy officials. While the Navy surgeon general is responsible for privileging providers for operational settings, the surgeon general delegated this authority to the command surgeon of U.S. Fleet Forces Command, as allowed in the DOD instruction.[16] According to Navy’s policy, the command surgeon may further delegate privileging authority to others, including the force medical officer, as appropriate.[17] Navy officials explained that the official to whom the privileging authority is delegated accepts providers’ existing privileges granted by DHA at the home military medical treatment facilities without modification—for clinical care provided during temporary assignments to operational settings, such as hospital ships; this process is known as privileging by proxy.[18]
Before a provider’s existing privileges are accepted, Navy officials told us officials in Fleet Forces review the provider’s transfer brief and all relevant materials, such as documentation of necessary training and clinical proficiency, to determine whether a provider’s credentials and privileges granted for care delivered in the military medical treatment facility are appropriate for the operational setting. Based on this review, Navy officials may document acceptance of the provider’s existing privileges in the centralized database managed by DHA or via memorandum, which is also stored in the database.[19] Navy officials indicated that documenting acceptance of privileges via memorandum is typically used for providers assigned to hospital ships. For example, Navy officials provided copies of the records for the two selected operational settings that documented the review of transfer briefs and acceptance of privileges for most of the 162 providers.[20]
Navy Evaluates Providers’ Performance in Operational Settings
According to Navy officials, Navy has two primary ways to evaluate privileged providers delivering care in all operational settings, depending on the length of time providers serve in that location. Evaluations are to be completed by officials within the provider’s medical chain of command and reviewed by the medical executive committee.
· Ongoing professional practice evaluations. According to Navy officials, Navy evaluates providers’ clinical competency every 6 months across all operational settings. However, due to the constraints of certain operational settings, Navy officials may not be able to upload these into the centralized database.[21]
· Performance appraisal reports. According to Navy officials, providers who are temporarily assigned to operational settings for 5 or more days but less than 6 months receive a performance appraisal report, which evaluates clinical performance. Performance appraisal reports are also routinely completed every 2 years as part of the privileging process, according to Navy officials.
Navy officials indicated that peer reviews may also be completed on a monthly or quarterly basis in the operational setting and stressed that they try to ensure that these peer reviews are performed by providers with similar skills.
We received performance appraisal reports for most of the 162 providers identified by Navy officials, as deployments to the two selected operational settings were less than 6 months. These reports also served as the end-of-deployment evaluation for these providers, according to Navy officials.
Air Force Approves Privileges and Conducts Evaluations for Providers Temporarily Assigned to Operational Settings
Air Force officials described for us the department’s current process for privileging providers for operational settings. In addition, Air Force officials described how they currently evaluate providers’ performance in these settings. Air Force officials indicated that privileging and provider evaluation requirements for operational settings would be included in their updated clinical quality management policies.
Air Force Approves Provider Privileges for Operational Settings
Air Force’s current process for privileging providers temporarily assigned to operational settings is based on the DHA procedures manual, according to Air Force officials. The Air Force surgeon general delegated privileging authority for operational settings to the Air Force medical commanders at military medical treatment facilities in April 2024, in accordance with the DOD instruction.[22] As a result, Air Force officials explained that the Air Force medical commander at the provider’s home military medical treatment facility is currently responsible for approving the provider’s privileges before the provider is sent to the operational setting. Air Force officials stated that the medical staff manager at the provider’s home military medical treatment facility reviews and verifies the provider’s credentials and conducts queries of national databases, as required in the DHA procedures manual. Then, the provider completes an electronic application for privileges in the centralized database, which is routed for approval by the Air Force medical commander.
The Air Force medical commander at the military treatment facility then conveys these privileges to the commander in the operational setting using the transfer brief, according to Air Force officials. Air Force officials explained that the commander in the operational setting reviews the transfer brief and may send a provider back to the home military medical treatment facility if that provider’s clinical skills are not aligned with needs in the operational setting.[23]
Air Force officials provided copies of privileging applications and original transfer briefs for some of the 41 providers temporarily assigned to the selected operational setting. However, Air Force officials could not provide us with the complete records for all providers because documentation was not preserved due to the rapid closure of that setting.[24]
Air Force Evaluates Providers at the Conclusion of 6-Month Deployments
According to Air Force officials, Air Force providers delivering patient care in operational settings are evaluated every 6 months—the typical duration of an Air Force deployment. According to Air Force officials, the provider evaluation is completed by the chief medical officer in that setting who evaluates if a provider is delivering quality health care. The Air Force documents these provider evaluations using a standardized Air Force form.
Air Force officials stated that providers leave the operational setting with paper copies of their provider evaluation forms. These forms should be uploaded into the centralized database managed by DHA by the military medical treatment facility commander upon providers’ return to the facility, as the database may not be accessible in operational settings, according to Air Force officials. Most of these evaluations for the 41 providers were unavailable; complete record preservation was not practicable due to the rapid closure of the operational setting we selected for our review, according to Air Force officials.
Army Does Not Have a Standardized Process for Privileging and Evaluating Providers for Operational Settings
We found that Army has neither a standardized privileging nor evaluation process for providers in operational settings. While Army officials told us the department is beginning to update its policies, Army officials could not describe a consistent process Army uses to ensure that its providers have the qualifications to provide clinical care in the assigned operational settings. Army officials also told us that evaluating provider performance is determined by the individual operational settings—not set by department-wide policy. Finalizing and issuing an updated policy per the July 2023 DOD instruction would help Army to establish standardized processes for provider privileging and evaluation of clinical performance in operational settings.
Army Lacks a Standardized Privileging Process
Army lacks a standardized process to privilege its providers for operational settings. Army officials could not definitively describe what steps, if any, Army currently takes to privilege providers for operational settings, and they stated this could vary by setting. Army officials stated that, in their experience, the commander in the operational setting should review the transfer brief prepared by DHA at the provider’s home military medical treatment facility and accept the provider’s existing privileges. However, Army officials also told us that the commander in the operational setting is not a designated privileging authority, as the Army surgeon general has not delegated privileging authority to these commanders.
Throughout our review, Army officials told us that DHA was responsible for privileging Army providers in operational settings. Specifically, in September 2023, Army officials told us that DHA was the privileging authority for operational settings. Army officials reiterated this position in February 2024 when they stated that DHA performs privileging for all Army providers.[25] Army officials told us they did not have the staff to perform privileging tasks because Army staff responsible for privileging providers were transferred to DHA after the management of the military medical treatment facilities transitioned from military departments to DHA. When we asked Army officials to reconcile their statements with the requirements in the law and the July 2023 DOD instruction, which states that military departments are responsible for privileging providers for operational settings, Army officials acknowledged that it was a poor assumption that DHA would perform privileging for operational settings.
As a result, Army officials told us in August 2024 that they are reliant on DHA officials at providers’ home military medical treatment facilities to carry out the responsibilities associated with privileging providers for operational settings. Army officials stated that identifying the appropriate privileging authorities for Army’s various operational settings is complex and that delegation of privileging authority would be premature without processes, resources, and communication plans in place to conduct these actions. Army officials stated that identification of privileging authorities for operational settings will be a key component of an updated policy.[26]
Army’s lack of a standardized privileging process for operational settings is inconsistent with the department’s responsibility for privileging these providers, as specified in the July 2023 DOD instruction. Updating its policy consistent with the July 2023 DOD instruction would align Army’s processes with the DHA procedures manual and help establish a standardized privileging process. A standardized privileging process would help ensure all providers in Army operational settings have the skills and training necessary to meet the health care needs of military personnel.
We reviewed available documentation related to provider privileging for two selected Army operational settings.[27] Because the Army operational settings we selected for our review were located in the U.S. Central Command area of responsibility, Army provided us with a privileging form—required to document review of the transfer brief and approval of privileges.[28] Army provided this form for nearly all of the 29 providers assigned to one of the two selected Army operational settings, and the majority of these forms were complete. Army officials told us that the required form was not completed for the 80 providers serving in the other selected operational setting because this facility was unaware of the requirement to complete the form. However, Army officials stated that the required privileging form has been completed for all providers in this operational setting since it became aware of the requirement in November 2023.
Army Does Not Have a Standardized Process for Evaluating Providers’ Performance in the Operational Setting
Army does not have a standardized process for performing provider evaluations in operational settings or for end-of-deployment evaluations, according to Army officials, though some operational settings may have their own requirements for evaluating providers clinical competence. Army officials noted that all Army service members receive officer evaluation reports, which assess their ability to carry out their military duties. For providers, these duties could include clinical responsibilities. However, these evaluation reports are not designed to assess providers’ clinical competency, according to Army officials, and may not be completed by medical personnel with the knowledge to do so. Army officials told us that providers may also have monthly clinical care peer reviews, but this is determined by the personnel and mission in each of Army’s operational settings.
Army officials stated that they would expect Army personnel assigned to operational settings to follow the DHA procedures manual, though, as previously mentioned, Army does not have an updated policy to communicate this expectation. Therefore, Army may not routinely evaluate performance of privileged providers in operational settings. Issuing an updated policy as required by the July 2023 DOD instruction would ensure operational settings follow the DHA procedures manual, which requires routine evaluations every 6 months and at the end of temporary assignments to operational settings.
Army provided us with peer review memos, summarizing which providers had peer reviews in a given month, from one of the two selected operational settings. These memos indicated that some of the 80 providers in this operational setting had received at least one monthly peer review.[29] Army was unable to provide us with provider evaluations for the 29 providers at the other selected operational setting because Army did not require peer review or other types of provider evaluations, according to Army officials. An updated policy that aligned with the DHA procedures manual would help ensure all providers are routinely evaluated for clinical competency in Army operational settings.
Conclusions
While the reorganization of the military health system begun in 2016 did alter certain responsibilities of the military departments, Navy, Air Force, and Army retained a responsibility they have long had: managing clinical quality in the operational setting. A central aspect of that responsibility has been their privileging and evaluation of providers sent to work in operational settings. Neither Army, Air Force, nor Navy have updated their policies regarding these responsibilities since prior to 2016, when DOD began its reorganization. We found that they are now in varying stages of updating their written policies as required by the July 2023 DOD instruction, to reflect the procedures manual issued by DHA in 2019.
Navy and Air Force were able to describe to us the process they have been using to privilege and evaluate providers in the operational settings. By finalizing and publishing updated policies, they can help ensure these policies are consistently applied in practice. Army is further behind the other departments in beginning to update its policies; the lack of a clear policy was evident in Army officials’ inability to describe a consistent process for either privileging or evaluating providers in operational settings. Furthermore, while Army commanders in operational settings may review privileging documents, these commanders are not able to privilege providers as Army’s Surgeon General has not delegated privileging authority to them—an issue that could be resolved in an updated policy.
Expeditiously issuing updated policies on the privileging of providers in operational settings, including when and how providers are evaluated while posted there, would provide certain assurances to all three military departments. Specifically, these policies could help ensure adequate and consistent review of providers’ qualifications and competency to provide the care needed in these settings given the resources available. As a result, Navy, Air Force, and Army would have greater assurances that deployed providers have the skills and training necessary to meet the health care needs of their patients.
Recommendations for Executive Action
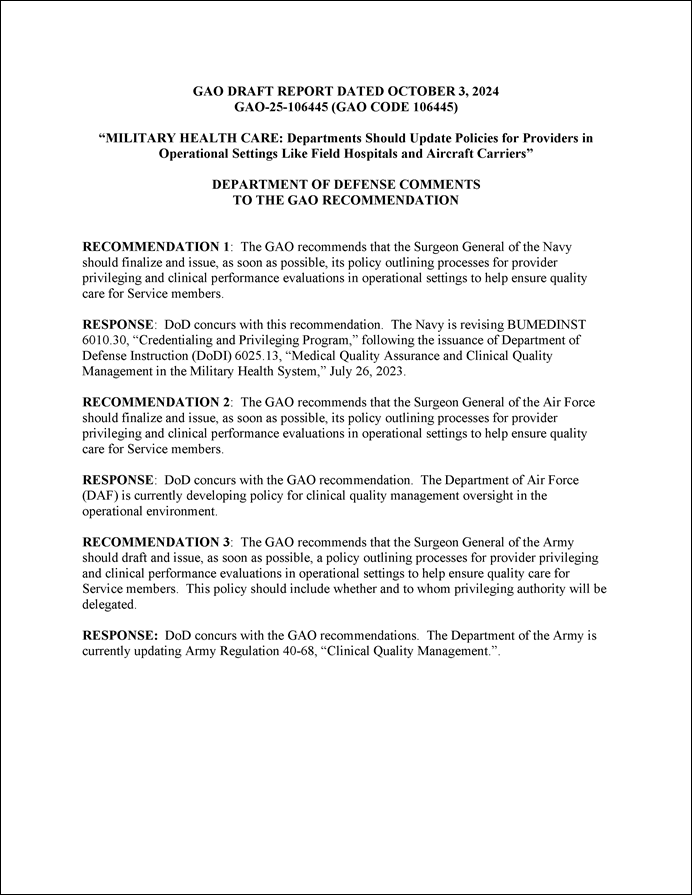
We are making three recommendations to the DOD military departments:
The Surgeon General of the Navy should finalize and issue, as soon as possible, its policy outlining processes for provider privileging and clinical performance evaluations in operational settings to help ensure quality care for service members. (Recommendation 1)
The Surgeon General of the Air Force should finalize and issue, as soon as possible, its policy outlining processes for provider privileging and clinical performance evaluations in operational settings to help ensure quality care for service members. (Recommendation 2)
The Surgeon General of the Army should draft and issue, as soon as possible, a policy outlining processes for its provider privileging and clinical performance evaluations in operational settings to help ensure quality care for service members. This policy should include whether and to whom privileging authority will be delegated. (Recommendation 3)
Agency Comments
We provided a draft of this report to DOD for review and comment. In its comments, reproduced in appendix III, DOD concurred with all three recommendations, stating that the military departments are currently revising and updating their relevant policies.
We are sending copies of this report to the appropriate congressional committees, the Secretary of Defense, and other interested parties. In addition, the report will be available at no charge on GAO’s website at http://www.gao.gov.
If you or your staff have any questions about this report, please contact me at (202) 512-7114 or at SilasS@gao.gov. Contact points for our Office of Congressional Relations and Office of Public Affairs can be found on the last page of this report. Other major contributors to this report are listed in appendix IV.
Sharon M. Silas
Director, Health Care
For the providers that served in our five selected operational settings, we requested available documentation related to privileges. This included documentation of privileges granted to providers at the military medical treatment facilities prior to assignment to operational settings and documentation demonstrating review and acceptance of providers’ privileges for operational settings. We also requested documentation of the respective surgeon general’s delegation of privileging authority for operational settings for each military department, as allowed by the Department of Defense instruction.
Privileges granted prior to operational setting assignments were documented in inter-facility credentials transfer briefs (which we refer to as transfer briefs).[30] For our request, the military departments provided transfer briefs, most of which were generated for us from information stored in the centralized database.[31] When the military departments recreated the transfer briefs from the database for our review, current information overwrote certain historic details about a provider’s privileges, which resulted in inaccuracies to these recreated transfer briefs. Therefore, we assessed them to be unreliable for our review. According to the Defense Health Agency (DHA), a permanent fix was implemented in March 2024 to ensure historic information would be maintained.
For most of the 312 providers, the military departments could not provide the original transfer briefs because copies were not required to be stored in the centralized database, according to officials. When available, we reviewed other documentation that military departments provided to support their review of the transfer briefs.[32]
We also requested documentation of evaluations that assessed provider clinical competency—that is, their ability to deliver quality care—at periodic intervals, rather than in response to a specific incident or inquiry. The documentation of these evaluations may vary by department. Also, prior to May 2023, certain provider evaluations were not required to be stored in the centralized database.[33] As result, some provider evaluations may have been unavailable to us for review.[34]
Navy performs all credentialing and privileging functions for providers permanently assigned to operational settings, according to Navy officials.[35] During the credentialing and privileging process, Navy verifies that a provider’s professional credentials—such as medical licenses—are valid and reviews these credentials and other qualifications to determine what privileges should be granted for the specific provider in that operational setting.
Navy officials told us that they follow requirements in the Defense Health Agency (DHA) procedures manual when credentialing and privileging permanently assigned providers for these operational settings. The DHA procedures manual requires review of the following types of information, among others:
· Provider medical licenses. Before Navy initially grants privileges, Navy officials must verify that each provider has at least one current, valid, active, and unrestricted license and that any additional licenses held by a provider, including inactive and expired licenses, are also in good standing. After privileges are granted, Navy officials must also verify that licenses that would expire during the privileging cycle are renewed, or allowed to expire in good standing if the provider has another active license.
· National database queries. As part of the credentialing and privileging process, Navy officials are to query databases that may contain potentially adverse information about individual providers,
including the National Practitioner Data Bank and the Department of Health and Human Services List of Excluded Individuals and Entities.[36]
· Provider evaluations. Navy officials are to collect and review information about providers’ performance to inform privileging decisions in a variety of ways, including through clinical references, professional practice evaluations, and performance appraisals completed at the end of each privileging cycle.
To understand how Navy implements these processes outlined in the DHA procedures manual, we selected two operational settings (aircraft carriers) to which providers were permanently assigned based on dates of recent deployments, in November 2022 and May 2023. We obtained and reviewed available documentation related to provider credentialing, privileging, and evaluations for the 17 privileged providers permanently assigned to the selected Navy operational settings.
We found that Navy generally followed requirements in the DHA procedures manual when credentialing, privileging, and evaluating permanently assigned providers during the most recent deployments for the selected aircraft carriers.
· Medical licenses. Navy provided documentation that it verified providers’ active, renewed, and expired licenses, as required by DHA, for nearly all providers assigned to selected aircraft carriers.
· National database queries. Navy provided documentation that it performed required queries of provider databases prior to privileging for all providers assigned to the selected aircraft carriers.
· Clinical references. Navy provided documentation that it obtained two clinical references from required individuals for all 4 providers assigned to the selected aircraft carriers on their first assignment (4 of the 17 providers) within the military health system, as required by DHA.[37] For the remaining 13 providers, Navy provided documentation of performance appraisal reports prepared at the provider’s previous duty station, which served as clinical references for providers previously working within the military health system.
· Ongoing professional practice evaluations. Navy provided documents used to track completion of ongoing professional practice evaluations, which showed that Navy monitored provider evaluations for nearly all of the 17 providers assigned to the selected aircraft carriers.[38]
· Performance appraisal reports. Navy provided documentation that it obtained performance appraisal reports from previous assignments for all of the 13 providers assigned to the selected aircraft carriers from another military health system facility, as required by DHA. Navy provided documentation of performance appraisal reports completed after assignment to the selected aircraft carriers for all of the 6 providers who had completed their assignments at the time of our review. The 11 remaining providers were still assigned to the operational settings at the time of our review and, therefore, would not have had a completed performance appraisal report.
GAO Contact
Sharon M. Silas, (202) 512-7114 or silass@gao.gov
Staff Acknowledgments
In addition to the contact named above, Jill K. Center (Assistant Director), Ann Tynan (Assistant Director), Erin C. Henderson (Analyst-in-Charge), Maggie Devlin, Jacquelyn Hamilton, Erin K. Rubens, Ethiene Salgado-Rodriguez, and Cathy Hamann Whitmore made key contributions to this report. Also contributing were Lori Atkinson, Loren Collier, Romonda McKinney, and Erin Pearson.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, X, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]Department of Defense, Defense Health Agency, Defense Health Agency Procedures Manual 6025.13: Clinical Quality Management in the Military Health System (Falls Church, Va.: Aug. 29, 2019).
[2]Department of Defense, DOD Instruction 6025.13: Medical Quality Assurance and Clinical Quality Management in the Military Health System (Washington, D.C.: July 26, 2023).
[3]H.R. Rep. 117-397, at 204 (2022). We plan to address additional aspects of how the military departments manage clinical quality in operational settings, such as review of patient safety events, in a subsequent report.
In an August 2022 report, we reviewed DHA’s processes for managing clinical quality at military medical treatment facilities, including credentialing and privileging. See GAO, Military Health Care: Improved Procedures and Monitoring Needed to Ensure Provider Qualifications and Competence, GAO‑22‑104668 (Washington, D.C.: Aug. 11, 2022).
[4]DOD Instruction 6025.13.
[5]DOD operational settings may be aligned with one of DOD’s 11 unified combatant commands, which are joint military commands of the DOD that are composed of units from two or more service branches of the United States Armed Forces and conduct broad and continuing missions. Because these combatant commands may have some oversight responsibilities for operational settings, we requested policy documents and interviewed officials, as needed. U.S. Central Command’s area of responsibility includes operational settings from the Middle East to Central and South Asia.
[6]Privileged providers are those who have been granted permission and responsibility to provide specified or delineated health care within the scope of the provider’s license, certification, or registration. Privileges granted prior to operational setting assignments were documented in inter-facility credentials transfer briefs (which we refer to as transfer briefs). These contain information such as a provider’s credentials (e.g., education, licenses, and certifications) and current practice privileges and locations.
[7]DHA is a joint combat support agency. That is, the agency’s purpose is to support the military departments with maintaining the readiness of medical personnel. Military medical treatment facilities provide the necessary clinical workload to meet the military departments’ medical readiness requirements, so that medical personnel possess the skills and knowledge needed to provide health care services in operational settings.
[8]See 10 U.S.C. § 1073c.
[9]See Pub. L. No. 116-92, Tit. VII, § 712(a)(5), 133 Stat. 1198, 1444 (2019).
[10]The procedures manual also describes focused professional practice evaluations, which are time-limited periods during which the military department evaluates and determine the provider’s professional performance. These evaluations may occur when a provider does not have documented evidence of competently performing a certain privilege or if a question arises regarding the provider’s ability to provide safe, high-quality care.
[11]Department of Defense, DOD Instruction 6025.13.
[12]Current versions of Navy, Air Force, and Army policies addressing provider privileging and evaluation are dated 2015, 2011, and 2004, respectively. For the current version of Navy’s policy, see Department of the Navy, Bureau of Medicine and Surgery, Credentialing and Privileging Program, Bureau of Medicine and Surgery Instruction 6010.30 (Falls Church, Va.: March 2015). For the current version of Air Force’s policy, see Department of the Air Force, Medical Quality Operations, Air Force Instruction 44-119 (Washington, D.C.: August 2011). Air Force also released a guidance memorandum to accompany this instruction in 2023; see Department of the Air Force, Medical Quality Operations, Department of the Air Force Guidance Memorandum to Department of the Air Force Instruction 44-119 (Washington, D.C.: March 2023). In May 2024, Air Force issued an additional guidance memorandum that extended the 2023 memorandum for another year; see Medical Quality Operations, Department of the Air Force Guidance Memorandum to Department of the Air Force Instruction 44-119 (Washington, D.C.: May 2024). For the current version of Army’s policy, see Department of the Army, Clinical Quality Management, Army Regulation 40-68 (Washington, D.C.: March 2004). Army also issued a rapid action revision of Army Regulation 40-68 in 2009; see Department of the Army, Clinical Quality Management, Rapid Action Revision, Army Regulation 40-68 (Washington, D.C.: May 2009).
[13]In December 2023, Navy issued an instruction pertaining to clinical quality management for health care delivered in operational settings under the control of the United States Fleet Forces Command and United States Pacific Fleet—two component commands within the Navy. The instruction covers provider privileging and evaluation. See Department of the Navy, U.S. Fleet Forces Command, U.S. Pacific Fleet, COMUSFLTFORCOM/COMPACFLT Instruction 6025.13: Fleet Clinical Quality Management Program (Norfolk, Va., Pearl Harbor, Hawaii: Dec. 6, 2023).
[14]Because draft policies are subject to revisions until finalized, we did not evaluate any draft policies provided by the military departments.
[15]See Air Force, Medical Quality Operations (March 2023) and Medical Quality Operations (May 2024).
[16]U.S. Fleet Forces Command is responsible for training, certifying, and providing combat-ready Navy forces to combatant commanders.
[17]Navy’s credentialing and privileging instruction includes the Navy surgeon general’s delegation of privileging authority for operational settings to the command surgeon of U.S. Fleet Forces Command and specifies that the command surgeon may further delegate privileging authority to the type commander fleet surgeon or force medical officer. The instruction also includes the Navy surgeon general’s delegation of privileging authority for the Marine Corps to the medical officer of the Marine Corps, who may further delegate privileging authority to the Marine Forces force surgeons or Marine Expeditionary Forces. See Department of the Navy, Bureau of Medicine and Surgery, Credentialing and Privileging Program, Bureau of Medicine and Surgery Instruction 6010.30 (Falls Church, Va.: March 2015). Navy officials explained that providers temporarily assigned to Marine Corps operational settings exercise privileges granted at their home military medical treatment facilities.
[18]According to the DHA procedures manual, privileging by proxy allows an institution to accept the privileging decision from another privileging authority to authorize care. The DOD instruction specifies that privileging by proxy may be used when privileges are not altered in a provider’s transfer to new clinical duties.
Navy hospital ships are mobile facilities equipped to provide a full spectrum of acute medical and surgical services. According to Navy officials, these hospital ships are typically deployed every couple of years to provide medical support for other U.S. military missions or to provide medical care as part of foreign and domestic humanitarian assistance and disaster relief missions.
[19]Navy officials explained that privileging by proxy is only used to accept “core privileges”—the expected baseline scope of care for a fully trained and competent provider of a particular clinical specialty—for the operational setting. While some providers may have additional non-core privileges, Navy officials indicated that settings outside of military medical treatment facilities only support core privileges.
[20]We did not examine transfer briefs provided by Navy because of problems with the reliability of these files when Navy recreated them for our review using information stored in the centralized database managed by DHA.
[21]According to Navy officials, while on board ships, there is no access to the centralized database. Instead, provider performance is documented in a file and then incorporated into performance appraisal reports.
[22]See Department of the Air Force, Headquarters United States Air Force, Delegation of Privileging Authority Responsibilities to DAF Medical Commanders (Washington, D.C.: April 2024). Air Force officials explained that this delegation memorandum was developed to clarify privileging authority within the Air Force in response to the July 2023 DOD instruction.
[23]DOD operational settings may be aligned with one of DOD’s 11 unified combatant commands, seven of which are geographic. For example, as a geographic combatant command, U.S. Central Command’s area of responsibility includes operational settings across the Middle East to Central and South Asia. Given that the selected Air Force operational setting was located within the U.S. Central Command area of responsibility, an additional privileging form was required per U.S. Central Command policy. Air Force officials stated that it was not possible to provide these forms to us because Air Force did not retain complete records due to the rapid closure of the selected operational setting.
[24]For the majority of providers assigned to the selected operational setting, Air Force recreated transfer briefs for our review using information stored in the centralized database managed by DHA. We did not examine these transfer briefs provided by Air Force because of problems with the reliability of these files when Air Force recreated them for our review. According to DHA, a permanent fix was implemented in March 2024 to address the reliability concerns. For more information, see appendix I.
[25]DHA officials stated that it is responsible for privileging only in military medical treatment facilities and has no authority to provide oversight for providers practicing outside these settings.
[26]Army officials indicated in August 2024 that a draft privileging authority delegation memorandum is in development, as is a memorandum of agreement with DHA to address privileging functions for operational settings, but Army officials did not provide a timeline for finalizing these memoranda.
[27]We did not examine transfer briefs provided by Army because of problems with the reliability of these files when Army recreated them for our review using information stored in the centralized database managed by DHA.
[28]According to U.S. Central Command officials, the form is required to be completed by the provider, officials at the provider’s home military treatment facility, and officials in the operational setting for providers assigned to a location under U.S. Central Command and does not apply to all operational settings. See “Credential Review and Privileging Form” in United States Central Command, Headquarters United States Central Command, Central Command Regulation 40-1, Medical Services, Healthcare Operations (MacDill Air Force Base, Fla.: February 2023).
[29]Providers may not have qualified for a peer review in a given month if they had not provided care to enough patients to achieve a sufficient number of clinical cases; documentation of peer review may have been unavailable for remaining providers, according to Army officials.
[30]The inter-facility credentials transfer brief is the means by which information is shared between different entities. The transfer brief contains information such as a provider’s credentials (e.g., education, licenses, and certifications) and current practice privileges and locations. The transfer brief conveys the documentation of privileges granted to providers at the military medical treatment facilities prior to their assignment to operational settings.
[31]The transfer briefs are generated by the centralized credentialing and privileging database managed by DHA, which stores information about providers’ privileges, among other information. When providers are deployed, transfer briefs are generated from the centralized database with the most current dates at that point in time, according to DHA officials.
[32]Navy officials provided records documenting their review of transfer briefs and Army provided an additional form used to document review of transfer briefs and approval of privileges, as required by U.S. Central Command policy.
[33]In May 2023, DHA issued a memo directing that all professional practice evaluations be uploaded to the DHA-managed database and was effective in November 2023. See Department of Defense, Defense Health Agency, “Clarification Regarding Current Clinical Competency and an Exception to Policy Concerning Professional Practice Evaluations” (Falls Church, Va.: May 2, 2023).
[34]Although some provider evaluations were not available for our review, it does not mean the evaluations were not completed.
[35]Navy officials told us that providers may be permanently or temporarily assigned to certain operational settings, such as aircraft carriers. Navy’s process to ensure providers are qualified to serve in these settings differs based on the provider’s type of assignment. According to Navy officials, privileged providers may be permanently assigned to these operational settings for 1- or 2-year tours depending on clinical specialty. This process is the same for providers assigned to Navy and Marine Fleet Forces, according to Navy officials. The second finding in the body of this report describes Navy’s processes for privileging providers that are temporarily assigned to operational settings.
[36]The National Practitioner Data Bank is an electronic repository administered by the U.S. Department of Health and Human Services that collects and releases information on providers such as those who have been disciplined by a state licensing board or have malpractice claims history. The presence of information in the National Practitioner Data Bank does not necessarily disqualify a provider from employment in the military health system. If any potentially adverse information is identified, then it must be reviewed to assess whether it is appropriate to grant (or renew) the provider’s privileges.
The Department of Health and Human Services List of Excluded Individuals and Entities database tracks providers who are excluded from employment under federally funded health care programs for a variety of reasons, such as a conviction for Medicare fraud or patient abuse. Unlike the National Practitioner Data Bank, appearing on the List of Excluded Individuals and Entities automatically disqualifies a provider from federal employment in any capacity, including in the military health system.
[37]We have previously reported that the DHA procedures manual is unclear regarding whether clinical references are also required when renewing privileges for existing providers. In August 2022, we recommended that the Director of DHA revise the procedures manual to clarify whether clinical references are required for providers whose privileges are being renewed. The Department of Defense concurred with this recommendation and DHA plans to update its implementation guidance in the short term and revise its procedures manual in the longer term. As of February 2024, the department estimated completion of planned actions in response to this recommendation in July 2025. In the interim, Navy officials indicated that the performance appraisal report prepared at a provider’s previous duty station takes the place of clinical references for providers who have been part of the military health system (i.e., previously assigned to another military health system facility). See GAO, Military Health Care: Improved Procedures and Monitoring Needed to Ensure Provider Qualifications and Competence, GAO‑22‑104668 (Washington, D.C.: Aug. 11, 2022).
[38]Prior to May 2023, ongoing professional practice evaluation summaries were not required to be stored in a central location.
