DEFENSE HEALTH CARE
Information Needed to Improve Monitoring of Military Personnel Staffing at Medical Facilities
Report to Congressional Committees
United States Government Accountability Office
For more information, contact Rashmi Agarwal at agarwalr@gao.gov.
Highlights of GAO-25-106988, a report to congressional committees
Information Needed to Improve Monitoring of Military Personnel Staffing at Medical Facilities
Why GAO Did This Study
In 2023, DOD announced that its roughly 700 medical facilities have been chronically understaffed in recent years. The facilities are staffed primarily with military medical personnel and augmented with DOD civilian employees and private contractor employees.
Senate Report 118-58 includes a provision for GAO to review military medical personnel staffing at DOD medical facilities. This report describes (1) trends in military medical personnel staffing at the facilities from fiscal year 2015 through fiscal year 2023; and evaluates the extent to which DOD has (2) a collaborative facility staffing process, and (3) taken steps to monitor the availability of personnel to work in medical facilities, among other things.
GAO reviewed DOD guidance and documentation and analyzed personnel data for fiscal years 2015 through 2023 and timecard data for fiscal year 2023. GAO also interviewed DOD officials and nearly 350 personnel from six medical facilities selected for site visits based on military department affiliation, location, and size.
What GAO Recommends
GAO is making seven recommendations, including that DOD evaluate which activities count as medical facility work time and communicate to military medical personnel the importance of timecard data and how it is used. DOD concurred with GAO’s recommendations.
What GAO Found
The number of military medical positions and assigned personnel in Department of Defense (DOD) medical facilities has declined over time. Specifically, the number of authorized positions for military medical personnel declined by nearly 7 percent (63,179 to 58,945) from fiscal year 2015 through fiscal year 2023. Likewise, assigned personnel declined by about 16 percent (60,479 to 50,590) during the same time. The decline in assigned personnel is in part attributable to fewer medical personnel in the Army, Navy, and Air Force (military departments). Senior leaders from the Defense Health Agency (DHA), which manages medical facilities, stated they anticipate substantial shortfalls in military medical personnel until at least 2027 when personnel levels may increase.
To help address facility staffing challenges, DHA and the military departments implemented a collaborative process to staff medical facilities with military medical personnel. Pursuant to 2024 guidance from the Office of the Assistant Secretary of Defense for Health Affairs (Health Affairs), DHA prioritized vacancies by facility and occupation, and the military departments identified personnel to fill them in 2025. DHA and the military departments are also collaborating to update medical facility personnel requirements for future years.
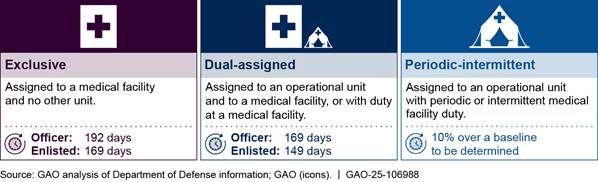
Health Affairs, DHA, and the military departments have taken steps to monitor the available work time of military medical personnel in medical facilities. The parties also agreed on how much time personnel would be expected to work in a facility as opposed to other military duties. These expectations vary depending on whether personnel are assigned exclusively to a facility.
Military Medical Personnel Categories and Annual Expected Medical Facility Work Time
To help ensure DOD meets these expectations, Health Affairs developed a monitoring tool that compares actual and expected work time by using medical facility timecard data from DHA. However, the monitoring tool is missing key information and relies on inaccurate and incomplete data. Specifically, the tool does not make key distinctions between facility work time and other time (e.g., deployments) or among personnel categories (e.g., exclusive vs. dual-assigned). Further, the tool relies on inaccurate and incomplete timecard data because DHA does not have a communication strategy, geared toward military medical personnel, that clarifies the importance of filling out timecards accurately, among other things. Until Health Affairs evaluates which activities count as facility work time in the tool and DHA communicates the importance of accurate timecard data, DOD will not have complete information to better monitor military medical personnel staffing at facilities.
|
Abbreviations |
|
|
DHA |
Defense Health Agency |
|
DOD |
Department of Defense |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
July 21, 2025
The Honorable Roger Wicker
Chairman
The Honorable Jack Reed
Ranking Member
Committee on Armed Services
United States Senate
The Honorable Mike Rogers
Chairman
The Honorable Adam Smith
Ranking Member
Committee on Armed Services
House of Representatives
The military health system has been challenged to provide enough personnel for its 736 medical facilities in the United States and overseas for the past several years, according to a 2023 Department of Defense (DOD) memorandum.[1] In peacetime and wartime, these medical facilities and the personnel who staff them are critical to DOD operations. They deliver health care to service members and to other beneficiaries entitled by law. The facilities are also training venues for military medical personnel to develop, improve, and sustain their skills. In wartime, the facilities receive and provide medical care to injured service members. Military medical personnel who staff the facilities must balance their work inside the facilities with military training and deployments outside the facilities. As a result, DOD augments the facilities’ staffing with civilian employees and private-sector contractors.
While facing military medical personnel shortages and the COVID-19 pandemic, the military health system has undergone a historic transformation that complicated its workforce management.[2] In November 2022, DOD completed a complex, multiyear transition of administration and management of its medical facilities from the Army, Navy, and Air Force (the military departments) to the Defense Health Agency (DHA) in response to a statutory mandate.[3] DHA is now responsible for managing the workforce of the facilities by setting personnel requirements, requesting military medical personnel from the military departments, hiring civilian employees, and contracting for personnel and services. The military departments are responsible for assigning military medical personnel to staff the facilities and other military units that require them (e.g., Army medical brigades, Navy ships, Air Force aeromedical evacuation squadrons, Marine Corps battalions).
As DHA has assumed responsibility for medical facility management, it has faced health care inflation, a constrained budget, and a challenging civilian labor market that together reduced the number of civilians and contractor personnel it could hire for the facilities.[4] In July 2023, we reported that budgetary and hiring constraints mean that DHA cannot always use civilian and contractor personnel to mitigate reductions in military medical personnel.[5] When DOD is unable to provide care in its facilities, it refers patients to its network of private-sector civilian providers through the TRICARE program.[6] This too has been an issue of concern for the department. The 2023 DOD memorandum cited a challenging health care economy, ambitious assumptions about patient care capacity in the private sector, and long-term cost growth in the private sector as factors that led DOD leaders to adopt a new strategy of reattracting patients to DOD’s facilities.[7]
We have previously reported on concerns about DOD’s workforce management of its medical facilities. In August 2023, we reported on the completion of DOD’s transition of the facilities to DHA, noting that DHA faced challenges mitigating persistent shortfalls of facility personnel that preceded the transition.[8] In November 2018, we reported that planning for the transition of medical facilities had not included the development of policies and procedures for the management of military personnel.[9] We therefore recommended that DHA and the military departments develop policies and procedures to manage military personnel. We describe steps DOD has taken to implement this recommendation later in this report.
More recently, a Senate Armed Services Committee report accompanying a bill for the National Defense Authorization Act for Fiscal Year 2024 noted that the transition of medical facilities to DHA has presented a challenge for balancing the military departments’ assignment of military medical personnel to the facilities with their assignment of such personnel outside the facilities.[10] The Committee expressed concern that competing priorities for such personnel might strain the facilities or require additional coordination between the military departments and DHA. Accordingly, the Committee report includes a provision for us to review military medical personnel staffing at the facilities. This report describes (1) trends in staffing military medical personnel to DOD medical facilities from fiscal year 2015 through fiscal year 2023; and evaluates the extent to which DOD has (2) a collaborative process to staff facilities, (3) taken steps to monitor the availability of personnel to work in medical facilities, and (4) an effective framework to oversee military medical personnel staffing at its facilities.[11]
For our first objective, we obtained and analyzed data from the Army, Navy, and Air Force on their assigned active component military medical personnel, comparing them with data on authorized active component positions (i.e., positions identified in DOD data as approved and funded) for military medical personnel from fiscal year 2015 through fiscal year 2023. We selected fiscal year 2015 to provide 2 years of data before the statutory requirement for transferring administration and management of the facilities to DHA.[12] Fiscal year 2023 was the most recent year of complete staffing data available from the military departments at the time of our review. We determined that the data were sufficiently reliable for identifying staffing trends over time by unit type by reviewing documentation on the databases, comparing them with other data sources, testing for errors and omissions, and interviewing military department officials.
To supplement our understanding of staffing trends and inform our other objectives, we also conducted site visits to a nongeneralizable sample of six US-based medical facilities and interviewed approximately 350 facility personnel, including doctors, nurses, x-ray and laboratory technicians, pharmacists, administrative staff, and facility leaders.[13] We selected these six facilities to provide variation across multiple characteristics, including the market type of each facility, military department affiliation, the presence of graduate medical education, the presence of collocated operational units, patient volume, and facility size.[14]
For our second objective, we reviewed staffing guidance and business rules on medical facility workforce management from the Under Secretary of Defense for Personnel and Readiness and the Assistant Secretary of Defense for Health Affairs. We also reviewed DHA documents on its staffing distribution process and results from fiscal year 2024 through fiscal year 2025. We compared DHA and military department actions against selected leading practices for interagency collaboration from our prior work.[15]
For our third objective, we reviewed information on a tool with which Health Affairs plans to monitor the availability of personnel working in medical facilities. Specifically, we reviewed information presented in the tool and the data sources that it leverages. Among these data sources, we reviewed 2023 data from DHA’s timecard system for four of the six selected medical facilities.[16] We also reviewed DOD reports about timecard data. We compared information presented by the tool and the quality of timecard data with the Information and Communication component from Standards for Internal Control in the Federal Government.[17] We also compared the accuracy and completeness of timecard data with a DOD instruction that describes the importance of quality military health system data.[18] We determined these data were not sufficiently accurate or complete to describe hours worked by military medical personnel at medical facilities. Therefore, we are not using the data to report how military medical personnel spend their time.
For our fourth objective, we reviewed and analyzed DOD guidance, memorandums, and reports regarding governance of the military health system and efforts to address medical facility staffing challenges. We also reviewed meeting minutes and briefings from two military health system governance councils for leadership discussions regarding facility staffing challenges and interviewed officials from the Office of the Assistant Secretary of Defense for Health Affairs. We compared this information with key elements of business and financial management systems oversight.[19]
For a detailed description of our scope and methodology, see appendix I.
We conducted this performance audit from July 2023 to July 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Organizational Roles and Responsibilities in the Military Health System
The military health system is a complex enterprise. DHA is responsible for health care delivery, and the responsibility for medical readiness is shared among the military departments—the Army, the Navy, and the Air Force—and DHA. The Office of the Secretary of Defense provides oversight of the military health system. Figure 1 illustrates the hierarchy of responsibilities executed within the military health system.
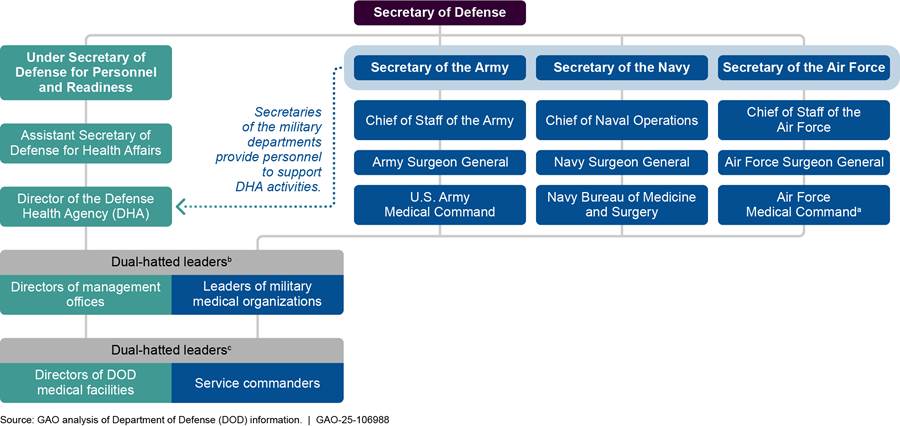
aAir Force Medical Command was established on August 15, 2024, according to Air Force officials, and achieved initial operational capability (i.e., establishment of its headquarters and subordinate commands and wings) on March 12, 2025.
bEight of the nine directors of the management offices are dual-hatted; that is, they also hold a leadership position in their respective military medical organization, according to DHA officials. Specifically, the directors of the Atlantic, Central, Continental, East, Europe, Indo-Pacific, Pacific Rim, and West management offices are dual-hatted. These same officials stated that the remaining management office director for the National Capital Region does not hold a leadership position in a military medical organization.
cDual-hatted medical facility directors or service commanders are military service officers. As facility directors, they exercise authority, direction, and control of all facility operations, and control of all personnel assigned or performing work duties at the facility, among other things. As service commanders for military medical personnel assigned to DOD medical facilities, they exercise administrative control in the facilities; exercise command and control over such personnel executing military service duties (e.g., planned and unplanned deployments, military operations, training, and exercises); establish personnel training requirements, and provide advanced notice to the DHA Director of personnel participation in training, among other things.
The Under Secretary of Defense for Personnel and Readiness is the principal staff assistant and advisor to the Secretary of Defense for health-related matters and, in that capacity, develops policies, plans, and programs for health and medical affairs.[20]
The Assistant Secretary of Defense for Health Affairs serves as the principal advisor to the Under Secretary of Defense for Personnel and Readiness for all DOD health-related policies, programs, and activities.[21] The Assistant Secretary has the authority to develop policies; conduct analyses; issue guidance; provide advice and make recommendations to the Secretary of Defense, the Under Secretary of Defense for Personnel and Readiness, and others; and provide oversight on matters pertaining to the military health system. The Assistant Secretary is responsible for developing a unified medical program budget for the military health system, which totaled $61.4 billion for the fiscal year 2025 budget request.[22] The Defense Health Program accounted for $40.3 billion of this requested amount and funded, among other things, the TRICARE program comprising medical facility operations in the “direct-care system” and private-sector health care from networks of civilian providers.[23]
The Director of DHA functions under the authority, direction, and control of the Assistant Secretary of Defense for Health Affairs. The Director manages, among other things, the execution of policies issued by the Assistant Secretary, the Defense Health Program appropriation, and the TRICARE program.[24] The Director’s administration and management responsibilities for medical facilities include budgetary matters; information technology; administrative policy and procedures; and military medical construction. The Director is also responsible for delivering high-quality care; meeting the military departments’ health care requirements; and providing the necessary clinical workload to meet the military departments’ medical readiness requirements, including the requirements of the senior military operational commanders of military installations.
The Secretaries of the military departments coordinate with the Assistant Secretary of Defense for Health Affairs to develop certain military health system policies, standards, and procedures and provide military personnel and other authorized resources to support the activities of DHA, among other things. They are also responsible for ensuring the readiness of military personnel and providing military personnel and authorized resources in support of the combatant commanders and DHA. Each military department maintains one or more medical headquarters organizations, which are responsible for developing and maintaining the readiness of medical personnel. The Surgeon General of each respective military department leads that medical organization and serves as the principal advisor to the Secretary of the military department concerning all health and medical matters of the military department.
Composition of Military Health System Medical Personnel
DOD’s total medical workforce comprises three main components: military medical personnel of the active and reserve components, federal civilian personnel, and private sector contractor personnel. Military medical personnel from the active components of each military department provide care to service members in deployed or “operational” settings and to service members and their qualified beneficiaries in medical facilities. Reserve component medical personnel generally provide care in operational settings. Federal civilians and contractor personnel generally provide care in medical facilities. Figure 2 shows the number of active and reserve component military medical personnel, federal civilian personnel, and estimated contractor full-time equivalent personnel that comprised DOD’s total medical workforce in fiscal year 2023.
Figure 2: DOD’s Active and Reserve Component Military Medical Personnel, Federal Civilian, and Estimated Contractor Full-Time Equivalent Personnel Comprising the Medical Workforce, by Total and as a Percentage, Fiscal Year 2023
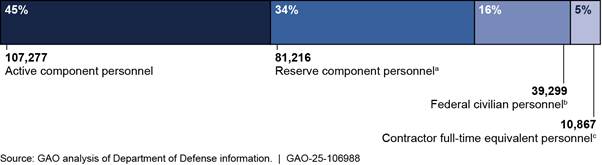
Note: This figure represents all military and federal civilian personnel with a primary medical occupation code and an estimated number of contractor personnel providing medical services funded by the Defense Health Program in fiscal year 2023. Total personnel for the active component, reserve component, and federal civilians are from GAO analysis of summary tables A2, R2, and C2 within the Health Manpower Personnel Data System report for fiscal year 2023. The actual number of personnel on board at the end of the fiscal year, as shown here, is also known as “end strength.”
aThe reserve component personnel total includes 66,055 Selected Reserve, 14,904 Individual Ready Reserve/Inactive National Guard, and 257 standby reserves.
bThe federal civilian personnel total includes only Department of Defense (DOD) civilian personnel and includes 38,939 full-time and 360 less than full-time federal civilians.
cThe contractor full-time equivalent personnel total represents the Defense Health Agency’s estimated number of contractor full-time equivalents supporting medical care contracts funded by the Defense Health Program in fiscal year 2023. The total was identified in a Defense Health Agency contract service exhibit supporting the fiscal year 2024 budget request for the Defense Health Program. Several factors limit the accuracy and completeness of contractor full-time equivalent data. See, for example, GAO, DOD Inventory of Contracted Services: Timely Decisions and Further Actions Needed to Address Long-Standing Issues, GAO‑17‑17 (Washington, D.C.: Oct 31, 2016) and GAO, Defense Acquisitions: Further Actions Needed to Improve Accountability for DOD’s Inventory of Contracted Services, GAO‑12‑357 (Washington, D.C.: Apr. 6, 2012).
Active component military medical personnel are the largest category of DOD’s medical workforce. Each department’s military medical personnel are grouped into corps of similar occupations. The officer corps include a medical corps of surgeons and other physicians, a nurse corps, a dental corps, and a medical services corps. Within the medical services corps are health care administrators, scientists, and clinicians in the Army and the Navy. In the Air Force, scientists and clinicians are part of a separate biomedical sciences corps. The Army also maintains a veterinary corps that provides DOD-wide services. The enlisted medical and dental corps include first responders, specialists who assist in medical and dental procedures, and medical materiel personnel. In this report, we use the term “military medical personnel” or “medical personnel” to refer collectively to officers and enlisted personnel of various medical occupations.
Military Medical Personnel Roles in Medical Facilities and Operational Units
Military medical personnel serve in various roles within medical facilities, from clinical care to administration and management. According to DOD Instruction 6000.19, each facility must spend most of its resources supporting wartime skills, developing and maintaining military medical personnel, or medically evaluating and treating service members.[25] Many facilities host graduate medical and dental education programs for physicians and dentists and other training and education programs for medical providers. Graduate medical education programs train student military medical personnel in physician specialties through internships, residencies, and fellowships. The facilities also train physician assistants, nurses, and enlisted technicians through non-graduate medical education programs. Day-to-day patient care helps maintain the clinical skills and readiness of military medical personnel.
Military medical personnel also serve critical roles in operational medical care, treating service members and other eligible persons in support of the full range of military operations. In operational settings outside of medical facilities (e.g., deployed environments), military medical personnel are part of Army medical brigades, Marine Corps battalions, Navy ships, and Air Force aeromedical evacuation squadrons.
Military Medical Personnel Assignment Process
Each military department maintains a personnel organization that is responsible for the distribution of its respective military personnel of all types—including medical personnel—in accordance with DOD and military department policy, guidance, and procedures.[26] These organizations include the U.S. Army Human Resources Command, Navy Personnel Command, and Air Force Personnel Center. Each organization has one or more offices that specialize in the distribution of military medical personnel, and each military service’s assignment process for military medical personnel is bifurcated into officer and enlisted assignments.
Each year a portion of the military medical personnel of each military department transitions to a new assignment. Assignments to medical facilities typically last 3 years, but the duration may vary depending on the location of the facility and the ability of family members to accompany medical personnel. According to military department officials, medical officers generally change assignments in the spring and summer—and to a smaller extent in the winter—whereas the number and timing of enlisted medical personnel movements vary by military department.
Each military department maintains its own prioritization guidance and target “fill rates” (i.e., the percentage of authorized positions filled with assigned personnel) for assigning military medical personnel when vacant positions exceed the personnel inventory. Officials from the military departments’ personnel organizations stated that they generally try to match the grade of military medical personnel to the needs of the gaining unit. The personnel organizations must also consider the professional development needs of military medical personnel and their personal circumstances, such as co-locating married service members.
Military Medical Positions and Assigned Personnel in DOD Medical Facilities Declined from Fiscal Years 2015–2023
The number of military medical positions and assigned personnel in DOD medical facilities has declined over time. Specifically, the number of authorized positions for military medical personnel in medical facilities declined by nearly 7 percent from fiscal year 2015 through fiscal year 2023, from 63,179 positions to 58,945 positions, according to our analysis of DOD data.[27] Likewise, the total number of personnel assigned to these positions declined each year over the same period by about 16 percent overall, from 60,479 personnel to 50,590 personnel. Figure 3 shows these declines in authorized positions and assigned personnel over this period.
Figure 3: Authorized Positions for Military Medical Personnel in Department of Defense Medical Facilities, and Personnel Assigned, Fiscal Years 2015–2023
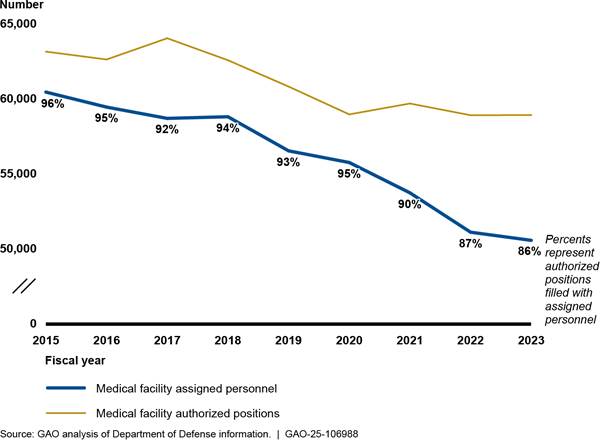
Notes: The data reflect authorized positions and assigned personnel as of September for each fiscal year except for the Army, for which assigned personnel are as of October. Medical facilities include inpatient hospitals and medical centers, ambulatory care and occupational health clinics, and dental clinics. The data for positions and assigned personnel encompass the medical corps of the active component of each military department. None of the data include non-medical authorized positions or assigned personnel, such as those for chaplains or food service workers. The Army data do not include those who are also assigned (i.e., dual-assigned) to an operational unit (i.e., Modified Table of Organization and Equipment Assigned Personnel). The Navy and Air Force data include those that are dual-assigned to an operational unit.
Figure 3 also shows the percentage of authorized positions filled with assigned personnel in medical facilities. By this measure, facility staffing levels declined from about 96 percent in fiscal year 2015 to about 86 percent in fiscal year 2023, according to our analysis.
However, based on our interviews with personnel and leaders at six selected medical facilities, we found that the overall staffing level at a point in time does not reveal staffing variations across the fiscal year or challenges in key parts of the facilities at specific times, such as spring and summer, when many military personnel are reassigned and take leave. This means the number of personnel at a facility varies throughout the year and may be higher or lower than the number assigned. For example, Naval Medical Center Portsmouth dropped from three general pediatricians to one in summer 2023, according to facility officials. Similarly, officials from the Army’s Guthrie Ambulatory Care Center stated that they fell from three obstetrician-gynecologist physicians to one (who is dual-assigned to an operational unit) in April 2024. This caused them to suspend inpatient women’s health services even with the arrival of a second, temporary physician from an Air Force medical facility through a process called a “manning assistance request.” According to the officials, they require at least three physicians for short-term labor and delivery coverage and at least four physicians to sustain the service. Military medical personnel may be reassigned or absent throughout the year for reasons such as deployments and training, retirement or separation from military service, parental leave, and providing temporary assistance at another medical facility to fill a critical vacancy.
DOD also uses military medical personnel for other units outside of medical facilities, such as operational units (e.g., Army medical brigades, Marine Corps battalions, Navy ships, and Air Force aeromedical evacuation squadrons) and headquarters organizations. In these types of assignments, military medical personnel may or may not have standing duty at a medical facility. Those with standing duty work in the facilities on a periodic basis to benefit their skills sustainment and the facility’s staffing. As shown in figure 4, these other authorized positions, outside of medical facilities, for military medical personnel increased overall by 5 percent from fiscal year 2015 through fiscal year 2023, from 46,482 positions to 48,823 positions. Over this period, the number of medical personnel assigned to these other positions increased from fiscal year 2015 through 2019 (from 50,323 to 51,696 personnel), and then declined each year from fiscal year 2020 through fiscal year 2023 (from 50,598 to 49,375 personnel), according to our analysis.[28]
Figure 4: Authorized Positions for Military Medical Personnel Outside Medical Facilities, and Personnel Assigned, Fiscal Years 2015–2023
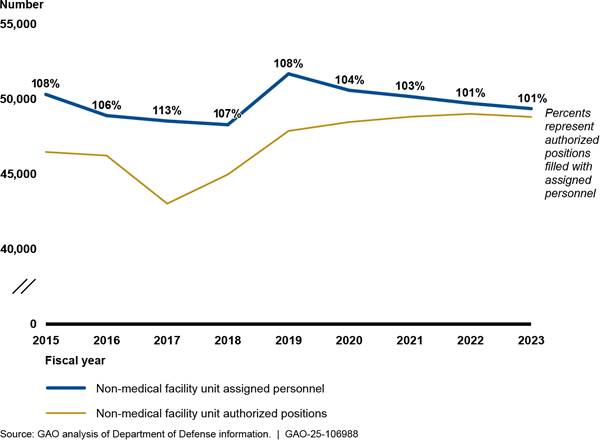
Notes: The data reflect authorized positions and assigned
personnel as of September for each fiscal year except for the Army, for which
assigned personnel are as of October. Non-medical facility units include
operational units (e.g., Army medical brigades, Marine Corps battalions, Navy
ships, and Air Force aeromedical evacuation squadrons) and headquarters
organizations. The data for positions and assigned personnel encompass the
medical corps of the active component of each military department. The Army positions
and personnel data include those that were also assigned (i.e., dual-assigned)
to an operational unit and concurrently to a medical facility (i.e., Modified
Table of Organization and Equipment Assigned Personnel from fiscal year 2019
through 2023). Navy and Air Force personnel who were dual-assigned to an
operational unit are not included because they are counted primarily as being
assigned to a medical facility. According to Army and Navy officials, staffing
levels exceeded 100 percent of authorized personnel for a few reasons. For
example, there were more assignable personnel to distribute across authorized
positions in earlier years over the period we reviewed because recruitment and
retention was better in those years than in more recent years.
Our analysis also found that the Army, Navy, and Air Force each remained generally stable over time from fiscal years 2015 through 2023, in terms of the proportions of their respective positions and assigned personnel that were allocated to medical facilities and other types of units outside the facilities. Figure 5 shows fiscal year 2023 in detail for Army, Navy, and Air Force authorized positions for military medical personnel.
Figure 5: Army, Navy, and Air Force Positions Authorized for Military Medical Personnel, Fiscal Year 2023
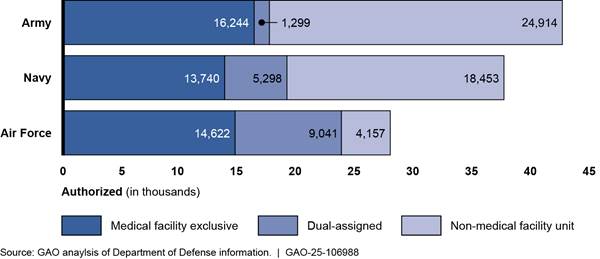
Notes: The data reflect authorized positions as of
September 2023 except for the Air Force dual-assigned positions, which are an
estimate based on requirements data as of December 2023. Air Force officials
were unable to provide fiscal year 2023 data on dual-assigned positions.
Medical facilities include inpatient hospitals and medical centers, ambulatory
care and occupational health clinics, and dental clinics. Non-medical facility
units include operational units (e.g., Army medical brigades, Marine Corps battalions,
Navy ships, and Air Force aeromedical evacuation squadrons) and headquarters
organizations, among others. Dual-assigned includes positions and personnel
concurrently aligned to an operational unit and a medical facility. The data
for positions and assigned personnel encompass the medical corps of the active
component of each military department. Data for medical facilities do not
include non-medical authorized positions or assigned personnel, such as
chaplains and food service workers.
As shown in figure 5, each military department has allocated a subset of military medical positions as dual-assigned. This means that those positions were aligned with an operational unit and a medical facility at the same time. Each military department is different in the command and control of personnel assigned to such positions.[29] According to officials from the Army, Navy, and Air Force medical headquarters, historically (i.e., since before fiscal year 2015) and through the present, a portion of their respective military medical positions or personnel for medical facilities has been dual-assigned to an operational unit. However, the military departments varied in what historical data were available; therefore, we are only reporting on fiscal year 2023 positions.
Overall decreases in the number of military medical positions at medical facilities and in the number of assigned personnel generally correspond with concurrent changes that affected the military health system. For example, the number of beneficiaries (including active duty service members and their families) enrolled in a TRICARE Prime health plan, through which they would receive most of their care in DOD medical facilities, has decreased over time, from 4.95 million in fiscal year 2015 to 4.47 million in fiscal year 2023.[30] In addition, from fiscal year 2015 through fiscal year 2019, the military departments completed downsizing initiatives for selected medical facilities. Specifically, we found that they eliminated or reduced inpatient capabilities at eight hospitals and closed or realigned some outpatient medical clinics.[31]
Alongside the reductions to medical facilities, the broader inventories of military medical personnel assigned to both medical facilities and non-medical facility units have also decreased in recent years. Overall, from fiscal year 2019 through fiscal year 2023 the total number of military medical personnel across the military departments declined about 8 percent, from 108,256 to 99,965. These totals include the numbers of military medical personnel assigned to medical facilities and non-medical facility units—as shown above in figures 3 and 4—and medical personnel who were temporarily unavailable for assignment due to factors such as a medical condition. The downward trend means there were fewer medical personnel overall who could be assigned to medical positions. In particular, enlisted medical personnel declined steadily from year to year over the period, from 74,406 to 65,443 (from 101 percent to 90 percent of authorized positions), and nurses declined from 9,165 to 8,584 (from 95 percent to 86 percent of authorized positions). DOD officials have attributed decreases in medical personnel to broader military recruitment challenges and, more specifically, to reductions in funding for military medical personnel. The military departments made those reductions in anticipation of a proposed DOD plan to realign and reduce active duty medical forces starting in fiscal year 2020. According to DOD, the plan was intended to increase the number of positions for other readiness requirements. Statutory mandates, however, required DOD to delay implementing this plan until 2027.[32] In addition, a March 2023 DOD review of the military health system’s response to the COVID-19 pandemic, which included lessons learned, found that the pandemic adversely affected recruiting, accession, and entry-level training activities.[33]
DHA and the Military Departments Implemented Collaborative Processes to Staff Medical Facilities
DHA and the Military Departments Implemented a Collaborative Staffing Process Consistent with Leading Practices to Assign Military Medical Personnel to Medical Facilities in 2025
In summer 2024, DHA and the military departments implemented a collaborative medical facility staffing process for military medical personnel. In applying this process, senior DHA officials stated they and the military departments agreed on the numbers and types of military medical personnel who would be assigned to fill clinical gaps within facilities in fiscal year 2025.[34] The collaboration and agreement were necessary because of the workforce management construct that DOD adopted when DHA assumed control of the facilities. Under the construct, the military departments retain control of their medical personnel and allocate a portion of them to DHA to staff facilities, while the other portion staffs other unit types, as discussed earlier in this report. Every year, a portion of all military medical personnel, like other military personnel, rotates to a new assignment. Thus, DOD’s June 2024 guidance calls for the collaborative staffing process to be repeated annually.
The newly implemented medical facility staffing process was consistent with guidance DOD issued in June 2024, which assigns the DHA Director responsibility for a Human Capital Distribution Plan that identifies expected vacancies of military medical positions at the facilities, prioritized by location and military occupational specialty.[35] The prioritization step is critical to the collaborative staffing process because the need for staff substantially exceeds the supply of military medical personnel who can fill them—a problem DHA senior leaders stated they expect to worsen through at least 2027 when levels of military medical personnel may begin to increase.
Subsequently, Health Affairs issued business rules in July 2024 operationalizing the new, collaborative medical facility assignment process.[36] According to the business rules, DHA should prioritize facility assignments by location and military occupational specialty and submit assignment requests to the military departments. In turn, the military departments are to review DHA’s priorities and propose a plan to meet them. Once agreed upon, the military departments will use the plan to assign military medical personnel using their existing assignment processes. To ensure that this process synchronizes with the military departments’ assignment processes, the business rules establish a timeline, by month. See figure 6 for an overview of this process.
Figure 6: Overview of DHA’s and the Military Departments’ Collaborative Process to Staff Medical Facilities
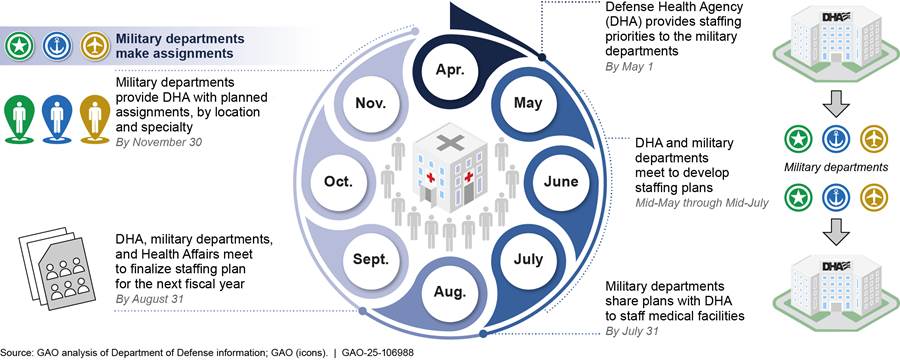
Note: These prescribed time frames are subject to change as the Defense Health Agency (DHA) and the military departments continue to refine the process, according to DHA officials. See, Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules (July 1, 2024).
Consistent with guidance and business rules, in May 2024 DHA identified for the military departments its highest priority medical facilities and occupational specialties for staffing in fiscal year 2025. According to DHA, these priorities are intended to facilitate the distribution of personnel to sustain clinical services. Using these priorities, DHA officials stated that they collaborated with military department officials from June through August 2024 to exchange information about DHA’s projected clinical gaps, the civilian employees it expected to have on board or hire, and the supply of military medical personnel who could be assigned. DHA officials added that they conducted planning sessions with the military departments from August through October 2024 in which they finalized a staffing plan for medical facilities for fiscal year 2025. Senior DHA officials stated that they and the surgeons general of the military departments jointly agreed on the staffing plan, also called the Human Capital Distribution Plan, in October 2024. A senior Health Affairs official stated that the Assistant Secretary of Defense for Health Affairs approved the plan in October 2024 through the military health system governance process.
In fiscal year 2025, the military departments are expected to identify individuals to fill gaps specified in the staffing plan and order them to report to their assigned facilities.[37] Nevertheless, DHA projects a shortfall numbering more than 8,000 clinical military medical personnel relative to DHA’s demand for health care services across its approximately 700 facilities.[38] According to a DOD briefing, the number of medical personnel that the military departments will assign to facilities for fiscal year 2025 is the most they can provide without jeopardizing the number they can assign to support operational requirements. DHA officials stated that they are unable to hire any civilian employees to help address the military medical personnel shortfall for the rest of fiscal year 2025.
Notwithstanding DOD’s continuing challenges with personnel shortfalls in its medical facilities, we found that the aforementioned steps to develop and implement a collaborative staffing process for the facilities are consistent with selected leading practices for interagency collaboration.[39] Specifically, DOD’s guidance and business rules, and efforts to implement them, address the following selected leading practices:
· Bridge organizational cultures. DOD’s business rules bridged organizational cultures by establishing procedures by which DHA and the military departments are to operate across agency boundaries. Specifically, the business rules direct that the collaborative staffing process synchronize with the military departments’ existing assignment processes.
· Identify and sustain leadership. DOD’s guidance identified Health Affairs in a sustained leadership role to review and approve staffing plans, among other things.
· Clarify roles and responsibilities. DOD’s guidance and business rules set forth the roles and responsibilities of DHA and the military departments in executing the collaborative staffing process for the facilities.
· Include relevant participants. DOD included relevant participants in developing the guidance and business rules by creating a working group for this purpose that comprises representatives from DHA, the military departments, and Health Affairs. Additionally, DHA and the military departments collaboratively developed a staffing plan for fiscal year 2025 in accordance with the business rules, as described above.
· Develop and update written guidance and agreements. DOD’s guidance states that the Assistant Secretary of Defense for Health Affairs is responsible for maintaining business rules for DOD’s collaborative staffing process. Additionally, DOD’s business rules direct DHA and the military departments to execute the collaborative staffing process annually, with the Assistant Secretary of Defense for Health Affairs approving staffing agreements reached between the parties each year.
DHA and the Military Departments Are Collaborating to Update Medical Facility Personnel Requirements for Future Years
DHA and the military departments are collaborating to comprehensively study and update medical facility personnel requirements—an essential precursor of the staffing process. While the staffing process distributes personnel to fill positions the following fiscal year, the identification of medical facility personnel requirements occurs 2 years or more in advance. As of March 2025, the parties had not finalized the new personnel requirements for future years, although DHA officials expect this step will be accomplished near the end of fiscal year 2025. According to a senior DHA official, this will mark the first time that DOD-wide requirements for facility personnel will have been cooperatively developed since the transition to DHA was completed in November 2022. In the meantime, the military departments have continued to independently identify and document their own military medical personnel requirements, including those for the facilities, while DHA has been responsible for developing the facilities’ civilian medical personnel requirements. However, DHA and the military departments have taken significant steps toward new facility personnel requirements by reaching consensus among key stakeholders on a methodology and an annual process for doing so.
DHA and the military departments began collaborating in November 2023 to develop updated facility personnel requirements, according to DHA officials. These efforts responded in part to concerns from DOD leaders who recognized that delays in the development of these requirements were one of many factors needing attention before the department could address medical facility staffing shortfalls across the military health system. The Deputy Secretary of Defense described these concerns in a memorandum issued in December 2023 calling for collaborative planning among DHA and the military departments in response to the staffing challenges.[40] DHA and military department officials formed a working group to address this aspect of the memorandum and accelerated efforts to develop guidance and a process for agreeing on facility requirements, among other aspects of workforce management.
The working group members drafted guidance that the Under Secretary of Defense for Personnel and Readiness signed in June 2024. The guidance directed DHA and the military departments to collaborate regarding projected medical facility staffing needs for future years as part of their existing planning and budgeting processes.[41] These processes are to be executed annually and cover a 5-year period. For example, in 2024, DHA and the military departments were responsible for establishing their personnel and fiscal resource requirements for fiscal year 2026 through fiscal year 2030, in accordance with the guidance. DHA is to identify its overall future facility requirements no later than June 30 each year.[42] Subsequently, the military departments should identify which of those requirements must be set aside for military medical personnel.
In September 2024, DHA leaders approved the last grouping of standardized, analytical models for personnel requirements that would calculate the specific numbers and types of clinical and administrative personnel needed to deliver health care services at each medical facility. According to DHA officials, in October 2024 DHA analysts finished applying these models to identify the personnel requirements for each facility, and then the military departments determined which of those requirements should be supported with military medical personnel.[43] In meeting these new personnel requirements, the officials also stated that each medical facility will retain its previous composition of military department personnel—that is, a facility on an Air Force base will continue to require and be staffed with Air Force personnel, and facilities that serve multiple military services (e.g., Walter Reed National Military Medical Center) will retain a mix of multi-service personnel. Finally, DHA officials stated that they shared a draft version of the facility personnel requirements and methodology with a broad group of stakeholders across the military health system in October 2024, including other military department officials, Defense Health Network directors, and facility directors. According to these officials, these stakeholders are to review the draft personnel requirements and provide input to DHA before they are finalized and documented in DOD’s official system of record. According to DHA officials, these stakeholders are to review the draft personnel requirements and provide input to DHA. This process is scheduled to be completed by September 2025. After personnel requirements are finalized, they are to be documented in DOD’s official system of record.
DOD Is Taking Steps to Monitor Military Medical Personnel Availability but Does Not Have Some Key Information or Fully Accurate and Complete Data
To improve the availability of military medical personnel at medical facilities, DOD established notification timelines for their absences from medical facilities and expectations for their work time. These actions were needed, according to DOD documents, because other military duties reduce the amount of time military medical personnel are available to work at medical facilities. Within DOD, Health Affairs plans to use a new tool to monitor the work time of military medical personnel at these facilities against work time expectations. The expectations vary depending on assignment type, otherwise known as personnel category. However, we found that the tool does not include key information that distinguishes between facility and non-facility work time or among military medical personnel categories. Furthermore, we identified issues with the accuracy and completeness of timecard data that the tool uses to monitor personnel availability.
DOD Established Notification Timelines and Work Time Expectations to Improve the Availability of Medical Facility Personnel
DOD has taken steps to improve the availability of military medical personnel to work at medical facilities following their transition from the military departments to DHA. Specifically, DOD leaders issued memorandums establishing that predictability and transparency are priorities for the military health system and directing steps to achieve those ends.[44] Those steps culminated in DOD’s issuance of guidance, in the form of a directive-type memorandum and business rules, in June and July 2024, respectively, as discussed earlier in this report.[45] These guidance documents established advance notification timelines for military medical personnel absences and expectations for facility work time, among other things. According to the business rules, this was necessary to ensure sufficient staffing because, unlike civilian employees, military medical personnel may work variable hours depending on their assignment type, military duties, and training. Specifically, the guidance establishes that the following expectations apply to the military departments, DHA, and Health Affairs:
· Notification timelines for personnel absences. The military departments are to notify DHA of expected absences of military medical personnel from their assigned facility due to trainings and deployments.[46] Specifically, the military departments should notify DHA at least 90 days in advance of absences for trainings lasting a week or longer, and at least 180 days in advance of rotational deployments.
· Expectations for personnel’s facility work time. The business rules established categories of military medical personnel by assignment type. These include 1) personnel assigned exclusively to a facility; 2) personnel dual-assigned to a facility and an operational unit; and 3) personnel who are assigned to an operational unit but work in facilities on a periodic or intermittent basis.[47] Military medical personnel in these three personnel categories—the largest categories working in medical facilities—are responsible for meeting hourly expectations set forth in the business rules, which vary by category. Differences in the expectations for facility work time reflect the variable hours that each personnel category can and should be expected to contribute to the facility versus other commitments, such as training and leave. According to a senior Health Affairs official, military department representatives used their judgment to set achievable expectations, basing them on an estimated number of hours devoted per month to military duties and training. Figure 7 shows the expectations for facility work time, by personnel category.
Figure 7: Categories of Military Medical Personnel Working in DOD Medical Facilities and Expectations for Available Work Time, as Established in DOD Business Rules
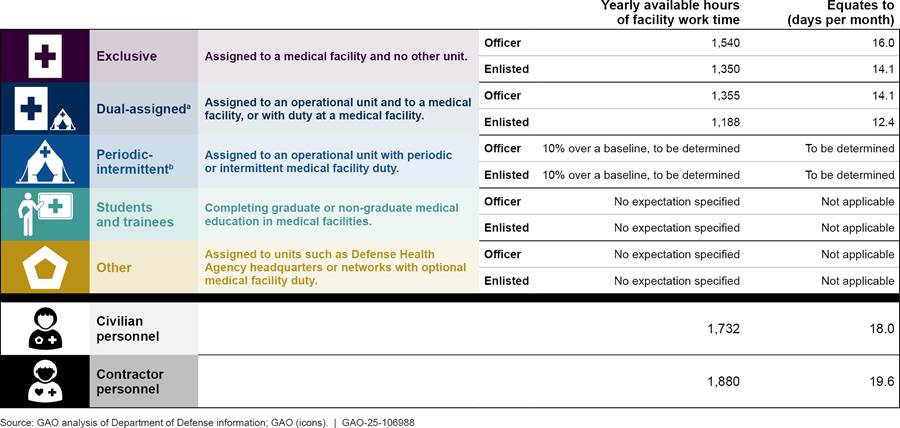
Notes: The personnel category names, descriptions, and related facility work time expressed in days per month are based on GAO analysis of Department of Defense (DOD) business rules, which present work time expectations in terms of yearly available hours of work time as shown. Estimates of days per month are based on an 8-hour workday. See Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules (July 1, 2024) and Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Staffing Transparency and Resourcing Impact Business Rules (July 1, 2024).
aSubject to vary based on exigent or validated operational requirements.
bPeriodic staff provide medical services to
support their unit or to enhance their readiness skills, whereas intermittent
staff have no recurring or standing duty or clinical time at a medical facility
but may work in a medical facility to sustain their medical readiness skills.
These actions were necessary because other military duties, including training, deployments, and collateral installation support responsibilities, reduce the time that military medical personnel are available to work in medical facilities. However, the timing and duration of the duties—and the resulting facility absences—vary depending on occupational specialty and the needs of operational units and the military installation the facility supports. Specifically,
· Individual training. Military medical personnel, regardless of their assignment, perform physical fitness training to meet service standards. They also complete sustainment training for their occupational specialty.[48] For example, military medical personnel assigned to the medical facility at Joint Base Elmendorf-Richardson—the Air Force 673rd Medical Group Hospital—were required to complete between 21 and 524 hours of medical readiness training in fiscal year 2024, depending on their occupational specialty. Personnel who provide clinical care may perform rotations in civilian hospitals periodically to meet clinical currency requirements of their military service, depending on their occupational specialty. Yet another subset of military medical personnel responsible for installation emergency response duties must complete additional training for those specific purposes.
· Unit training and deployments. Military medical personnel assigned to an operational unit participate in unit activities, such as training exercises and deployments. Personnel with an operational unit assignment include those who are dual-assigned with orders to a medical facility, and those without orders to a medical facility but who perform duty there on a periodic or intermittent basis. These unit activities limit the availability of these personnel to work in the facilities.
· Installation support duties. Military medical personnel assigned to medical facilities may be tasked with performing duties in support of their host installation. According to a facility director, their ability to decline such requests from commanders outside the facility is limited even in times of staffing shortfalls because certain taskings are a shared responsibility among all tenant units on an installation. Taskings to medical personnel may include gate security, medical coverage at firing ranges, and medical support at special events, among other things.
Competing demands for military medical personnel have been a long-standing workforce management challenge for medical facilities that predates the transition of facilities to DHA management. For example, in a 2016 report to Congress on military health system modernization, DOD acknowledged that operational missions and training demands constrain the efficiency and effectiveness of medical facilities.[49] Accordingly, DOD’s report recommended productivity standards for selected military physician specialties as a mitigation strategy to improve efficiency, based in part on estimates of personnel absences for military duties. These challenges persisted following the transition of medical facilities from the military departments to DHA in 2022. For example, in August 2023, we reported that DHA faced challenges in mitigating shortfalls of military medical personnel from the facilities due to factors such as deployments and training, which predated the transition of facility management responsibility.[50]
DOD’s Monitoring Tool Does Not Have Some Key Information or Fully Accurate and Complete Data Needed to Determine Medical Personnel Availability
Medical Workforce Monitoring Tool Consolidates Staffing Data Sources
According to DOD’s July 2024 business rules, on a quarterly basis Health Affairs will analyze actual facility work time relative to expected work time for the categories of military medical personnel described previously, such as those exclusively assigned to a medical facility or dual-assigned to a facility and to an operational unit (see fig. 7).[51] The analysis informs DOD’s collaborative facility staffing process and its oversight of the military health system, described later in this report.
To perform this analysis, a senior Health Affairs official stated that the office has begun using a monitoring tool designed to improve transparency of the distribution of the military medical workforce.[52] The tool consolidates, among other things, data on staffing requirements and personnel assignments, to include occupational specialty and location. The tool also incorporates data from DHA’s medical facility timecard system, in which personnel (military, civilian, and contractor) self-report their time from the preceding 2 weeks. In completing a timecard, personnel use activity codes that describe how they allocated their time each day that they worked or took leave.[53] The activity codes range from those denoting time spent in specific parts of the facility (e.g., intensive care unit), to continuing education, various types of training, deployment, and more. For illustrative purposes, figure 8 shows a notional example of a timecard for a military medical provider that reported a range of activity codes during the 2-week period.
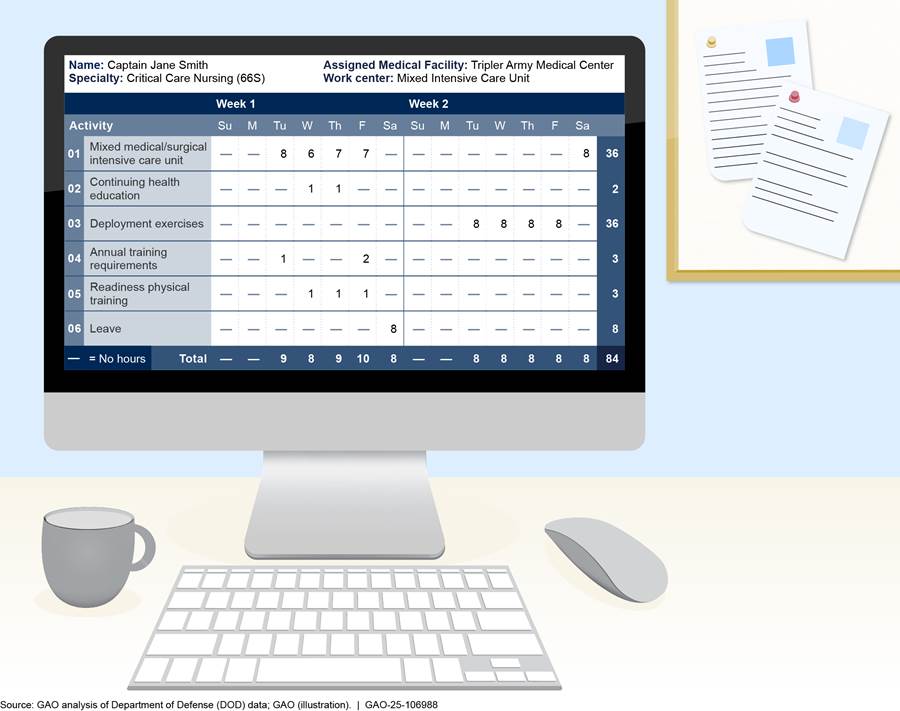
According to a senior Health Affairs official, coupling assignment data with
timecard data will enable comparisons between expected and actual facility work
time, pursuant to the July 2024 business rules. As of March 2025, a senior
official from Health Affairs stated that the office began high-level monitoring
that month by reviewing hours of service member work time according to
groupings of occupational specialties, facility, and military department.
Health Affairs’ Monitoring Tool Does Not Have Some Key Information
Notwithstanding DOD’s progress in developing facility work time expectations and its tool for monitoring, we found that the monitoring tool is missing key information needed to identify actual facility work time for personnel by category (i.e., exclusive, dual-assigned, and periodic-intermittent) in accordance with the July 2024 business rules.
First, the monitoring tool does not include key information that distinguishes medical facility work time from non-facility work time. According to the business rules, expectations for facility work time include the hours an individual is present for work at the direction of the medical facility; thus, training and activities performed with operational units should not count towards facility work time. As noted above, the tool incorporates source data from DHA’s timecard system to monitor facility work time against expectations. However, we found that the tool counts all recorded work time as facility work time even when accounting codes in the source data signify time spent on military duties outside the facility, including deployments.[54]
Second, we found that the monitoring tool does not distinguish among military medical personnel by category as the July 2024 business rules directed. As described previously and shown in figure 7, the business rules established personnel categories and facility work time expectations for officers and enlisted personnel in three categories: exclusive, dual-assigned, and periodic-intermittent. The monitoring tool can differentiate officers from enlisted personnel because timecard data and personnel assignment data consolidated within the tool include these variables. Based on our interviews and reviews of military department documents, we found that additional data from military departments’ personnel systems could be used to categorize each service member (exclusive, dual-assigned, or periodic-intermittent) in its tool. However, as discussed below, this has not been done. The personnel categories are needed to compare actual time worked against an appropriate expectation. For example, a medical officer exclusively assigned to a medical facility is expected to work 16 days per month in the facility, compared to a dual-assigned medical officer, who is expected to work approximately 14 days per month.
Federal internal control standards state that agency management should use quality information to achieve the entity’s objectives.[55] In doing so, management processes the data into quality information that is appropriate, current, complete, accurate, accessible, and provided on a timely basis. Then, management uses the quality information to make informed decisions and evaluate the agency’s performance in achieving key objectives and addressing risks. Applied to efforts to analyze military medical personnel availability, this means that Health Affairs needs to use available data sources to distinguish between facility and non-facility work time and among categories of military medical personnel so that its monitoring tool can facilitate the sort of information tracking required in the business rules.
We found two reasons why Health Affairs does not have the key information needed in its monitoring tool. First, Health Affairs has not evaluated activity codes in DHA’s timecard system to determine which should count toward expectations for medical facility work time versus those that should not. Without this step, Health Affairs could miscount the number of hours that personnel are performing work at medical facilities, putting at risk DOD’s ability to achieve the military medical personnel availability necessary to ensure sufficient staffing levels.
Second, Health Affairs officials confirmed to us they have not worked with military department officials to categorize individual military medical providers in their monitoring tool with a variable identifying them by personnel category (e.g., exclusive, dual-assigned, periodic-intermittent). Until it does so, Health Affairs cannot know the extent to which military medical personnel are meeting or exceeding expectations for facility work time, which is necessary to ensure sufficient staffing levels.
Monitoring Tool Uses Timecard Data That Are Not Fully Accurate or Complete
Beyond the limitations of the monitoring tool described above, the tool uses timecard data that are not fully accurate or complete. This is a longstanding issue, and prior DOD reports have identified concerns with the reliability of the timecard data, citing limitations in their accuracy and completeness. For example, a 2016 DOD report to Congress on military health system modernization found that timecard data were not reliable for the purposes of identifying time that military medical personnel work in facilities as opposed to time spent on other activities.[56] Similarly, a 2024 Army report found that the Army was unable to accurately measure the facility work time of its military medical personnel using timecard data.[57]
Echoing the concerns raised in these reports, DHA senior leaders acknowledged issues with the accuracy and completeness of timecard data, including issues identified from their data reliability checks. For example, in August 2024, DHA senior leaders told us that they continue to observe data quality issues in timecards submitted by enlisted medical personnel in particular, such as enlisted personnel underreporting time spent on non-medical facility work. Instead, according to DHA senior leaders, they believe enlisted medical personnel are reporting time spent performing non-facility work as facility work time.
In addition to concerns with time charges being misallocated between medical facility and non-facility tasks, DHA senior leaders stated that they have identified military medical personnel working in facilities who were not completing a required timecard. Specifically, based on an analysis of 2024 timecard data, DHA senior leaders estimated that approximately 15 percent of Army personnel who worked in a facility over the period did not submit a required timecard. By comparison, senior leaders estimated that about 1 percent of Air Force and Navy personnel who worked in a medical facility did not submit a required timecard.[58] The underreporting of timecards would mean that both hours spent on facility work and non-facility work would be underreported. According to DHA officials, they collaborated with the Army and facility officials to resolve technical issues with the timecard system that contributed to the problems with underreporting.
We also identified areas of concern with the accuracy and completeness of timecard data by interviewing military medical personnel at the six selected facilities. Concerns from military medical personnel we spoke with included the following:
· Personnel at all six facilities believed timecard data do not accurately reflect work hours at the facility or on military duties outside facilities for many reasons. For example, personnel stated that completing a timecard is a low priority to them or others because it is not tied to their pay. Another reason cited is that some personnel complete their timecard at the end of a 2-week period when they do not accurately remember what tasks they performed or for how long.
· Personnel at all six facilities were unsure about the purpose of the system or the importance of their data being accurate.
· Personnel at four of the six facilities stated that they or others have reported hours that they were expected to work on various tasks as opposed to the actual number of hours worked, such as allocating a set number of hours each week to military activities.
· Personnel at four of the six facilities stated that they have underreported their work time in the past. One of the reasons for this was that personnel believed certain tasks did not need to be recorded, such as additional time spent at home on administrative tasks after normal duty hours.
Leadership or timekeeping personnel at three medical facilities stated that military medical personnel who work intermittently in the facility (i.e., those in the periodic-intermittent personnel category from figure 7 above) do not always complete a timecard. In addition, data quality issues are not always identified and corrected before timecard data are finalized and sent to DHA. For example, timekeeping personnel at one facility described instances where military medical personnel away on field training exercises erroneously submitted timecards reporting that they worked full-time hours at their assigned facility. These instances of overreporting facility work time were not noticed and corrected before the facility submitted the timecard data to DHA.
Our analysis of fiscal year 2023 timecard data from four selected medical facilities corroborated concerns about accuracy and completeness cited in our interviews with DHA officials and facility personnel.[59] For example:
· Of 342 military personnel assigned to one facility, 22 percent of them recorded all their time to a single activity during November 2022. Among the other three facilities we analyzed, the percentage of personnel recording all their time to a single activity during November 2022 ranged from 6 to 10 percent. According to DHA officials, this is a “red flag” for inaccurate data, as personnel generally spend time on more than one activity per month.
· Of 563 military personnel assigned to another facility, 67 percent of them recorded 6 or fewer hours spent on mandatory annual DHA training during fiscal year 2023. Among the other three facilities we analyzed, the percentage of personnel that recorded 6 or fewer hours spent on mandatory annual DHA training during fiscal year 2023 ranged from 39 to 66 percent. In fiscal year 2023, the estimated time commitment for this training totaled over 11 hours. This means some staff who reported 6 or fewer hours may have underreported their training hours or misallocated the balance of hours to another activity. Some staff may have accurately reported their time if they completed the training more quickly or did not complete it.
· At one facility and its associated clinics, 44 out of 152 military medical personnel that had primary care appointments with patients during October 2022 did not complete a timecard.[60]
DHA senior leaders and other officials we spoke with were aware of the types of issues we identified, and officials stated they work routinely with medical facilities to address them and improve compliance with a DHA procedures manual that prescribes guidance for reporting work hours in the timecard system.[61] These officials also described data quality steps they take on an ongoing basis. Among other things, these steps include manually reviewing timecards and testing the data at the facilities; providing facilities a tool to identify personnel who report inaccurate data; assigning DHA analysts to support facilities’ data quality efforts; creating templates for timecards to make data entry quicker and easier; and offering instructional materials to facility personnel responsible for approving timecards. These are positive examples of control activities, which agencies design to achieve objectives and respond to risks in their internal control systems.[62] Yet, DHA leaders noted that issues with accuracy and completeness of the data persist despite the efforts described above.
A DOD instruction states that the quality of military health system data is critical to the effectiveness of performance-based management, resource allocation, decision-making at all levels, and many other operations and management activities across the system.[63] Similarly, federal internal control standards state that agency management should use quality information to achieve its objectives, including by obtaining relevant data from reliable sources that are reasonably free from error and bias.[64] Applied to efforts to monitor military medical personnel availability, this means that Health Affairs needs accurate and complete timecard data to ensure that personnel are meeting expectations for facility work time and, moreover, helping address the demand for health care services while personnel remain in short supply.
We found that Health Affairs does not have accurate and complete timecard data for its monitoring tool because DHA and the military departments have not taken action to address several underlying data quality issues. First, DHA is responsible for the timecard system but does not have a clear communication strategy for all military medical personnel—including those in dual-assigned and periodic-intermittent personnel categories—to understand the importance of timely and accurate timecard data. For example, although medical facility leaders and timekeeping staff at multiple facilities emphasized to us the importance of the timecard data for facility management, other facility personnel we interviewed were not sure how timecard data are used or why they are important, as described above.
Second, while DHA has taken some actions to address challenges with capturing accurate timecard data, problems persist. DHA has not analyzed and addressed root causes of the long-standing data quality issues and, according to DHA senior leaders, is not planning to do so until the agency completes other tasks deemed as higher priorities, including the completion of facility personnel requirements discussed previously. DHA officials described some of their efforts to address challenges with capturing accurate timecard data, such as standardizing timecard activity codes across medical facilities, reviewing and adjusting them annually, providing instructional materials to facility personnel on completing a timecard, and developing timecard templates. However, military medical personnel we interviewed at all six selected facilities described challenges to completing an accurate timecard. For example, personnel stated that they believe there are too many activity codes, and that the system is difficult to use.
Third, we found that military medical personnel from the periodic-intermittent personnel category may not always complete a timecard—despite DHA guidance directing them to do so—because the military departments have not issued policies to clarify and reinforce the DHA requirement.[65] Periodic-intermittent medical personnel are accountable to two separate authorities when working within a medical facility: 1) the commander of their assigned operational unit, who maintains command and control of these personnel and serves as their primary rater; and 2) the DHA Director, who exercises authority, direction, and control of these personnel when they work within a facility.[66] Leadership personnel from two of the six medical facilities we interviewed stated that they struggle to enforce timecard compliance among periodic-intermittent personnel. Leadership from one of the six facilities explained that these personnel focus on meeting the priorities of their unit commanders, which may not include timecard compliance.
To ensure that all military medical personnel complete a timecard when working in a facility, an August 2022 memorandum from the Under Secretary of Defense for Personnel and Readiness directed the military departments to issue a policy requiring their respective personnel to complete a timecard when working in a facility, regardless of their assignment.[67] However, as of January 2025, an Air Force official stated that the Air Force did not have such a policy and did not plan to issue one. The official stated that it was not appropriate to issue an Air Force policy concerning a DHA data system. Army and Navy officials stated that as of January and February 2025, respectively, the Army and Navy were each developing a policy, but the officials did not provide a time frame for issuance.
Senior leaders from DHA stated that they understand improvements to the accuracy and completeness of the data are necessary for the timecard system to improve monitoring and, by extension, compliance with the business rules. According to DHA senior leaders, medical facility personnel requirements and staffing plans have taken precedence over timecard system improvements. However, a program management official for the timecard system stated that DHA leaders have begun discussing plans to modernize the system by 2027.
As DHA begins modernization planning for the timecard system, Health Affairs needs accurate information on work time to make tradeoffs between military personnel’s time spent in facilities versus time spent on military activities. Establishing a clear and consistent communication strategy with military departments’ medical personnel will be important to help ensure an understanding of why accurately recording time worked in and outside of medical facilities is important. Further, analyzing and addressing root causes of data quality issues would help improve the quality of information DOD obtains through the system to help manage its medical facility workforce. Without taking these actions, Health Affairs will not be able to accurately calculate whether military department personnel are meeting the facility work time expectations set forth in DOD’s July 2024 business rules. In addition, until the military departments issue policies requiring all their personnel to complete a timecard for time worked in a facility, regardless of their personnel category, some military medical personnel are likely to remain noncompliant with DHA’s guidance.
DOD’s Framework to Oversee Medical Facility Staffing Meets Leading Practices
We found that DOD’s framework to oversee military medical personnel staffing at medical facilities meets leading practices as the department takes steps to address persistent and historic shortfalls in meeting the demand for health care services. Specifically, DOD’s actions have addressed each key element of effective business and financial systems oversight established in our prior work, including establishing oversight processes, sustaining leadership commitment, managing risk, and using and communicating quality information.[68]
Oversight processes. DOD policy and guidance describe oversight processes for the military health system, including medical facility staffing issues.[69] Together, they establish the Assistant Secretary of Defense for Health Affairs as the oversight authority for personnel policy and staffing, among other issues. In updating medical workforce management guidance in June 2024, DOD reaffirmed and expanded the Assistant Secretary’s oversight responsibilities.[70] Among other things, the Assistant Secretary is responsible for overseeing the new and collaborative process to develop annual medical facility staffing plans and performing quarterly reviews of staffing, as discussed previously.[71] Officials from Health Affairs also review the military departments’ proposed yearly allocations of positions between facilities and non-facility units, according to a senior official, and recommend the military departments adjust the balance of positions when needed.
For oversight purposes, DOD maintains a military health system governance process comprising deliberative bodies of stakeholders from Health Affairs, the military departments, DHA, and the Joint Staff, among others. For example, the Deputy Military Medical Action Council, chaired by the Principal Deputy Assistant Secretary of Defense for Health Affairs, is responsible for resource planning and allocation, among other things. The Senior Military Medical Advisory Committee, chaired by the Assistant Secretary, is the next-highest body that adjudicates and resolves challenges with policy and the Defense Health Program appropriation.[72]
Our review of meeting minutes from these two governance bodies from fiscal year 2023 showed that medical facility staffing was a recurring topic as they deliberated ongoing staffing challenges and the future of the military health system under a constrained budget.
Leadership commitment. In recent years, workforce management challenges in the medical facilities, including staffing shortfalls, have received senior leadership attention from the Secretary of Defense and the Deputy Secretary of Defense, in addition to receiving attention from the previously-discussed governance councils. By directing studies, monitoring progress, and issuing memorandums, senior leaders have demonstrated a sustained commitment to facility staffing oversight. For example, the Secretary and Deputy Secretary have directed studies of facility staffing issues, including one the Secretary directed to Health Affairs in 2023 to evaluate recruiting and retention of military and civilian personnel by conducting focus groups. In addition, periodic meetings of the Deputy’s Workforce Council—a senior DOD governance forum chaired by the Deputy Secretary of Defense—have reviewed facility staffing-related topics.
The Deputy Secretary of Defense issued a memorandum in August 2023 that formalized “medical reform,” including the use of medical staffing information, as one of DOD’s “Priority Cross-Cutting Performance Improvement Initiatives” for fiscal year 2023 through fiscal year 2024.[73] DOD’s Performance Improvement Officer is responsible for assessing medical reform and other initiatives and providing written assessments to the Deputy Secretary of Defense. In December 2023, the Deputy Secretary of Defense issued a memorandum to leaders across the department that established a strategy and implementation steps to stabilize the military health system and mitigate ongoing challenges, including staffing shortfalls.[74]
Managing risk. Health Affairs and its supporting governance councils have used a risk management approach in their oversight of military health system staffing by identifying challenges and developing solutions. Health Affairs and the councils have identified limitations on military and civilian personnel and fiscal resources for the Defense Health Program as a risk to the military health system. DOD imposed these limitations—including a plan to reduce the size of the military medical force by more than 12,000 personnel and budget reductions to the Defense Health Program—on the military health system for fiscal year 2020 through fiscal year 2027 as DOD leaders sought to reallocate personnel and fiscal resources to other readiness priorities. As discussed previously, the National Defense Authorization Acts for Fiscal Year 2020 through Fiscal Year 2023 delayed the medical personnel reductions until December 2027.[75]
Meanwhile, however, the Military Health System Executive Review Board commissioned a team of representatives from Health Affairs, other Office of the Secretary of Defense components, the Joint Staff, DHA, and the military departments to study options for reshaping the military health system. The study was to consider various personnel and fiscal resource scenarios, such as consolidating or expanding medical facilities and identifying the cost and risks of each option. The study team presented its findings and recommendations through the military health system governance process in 2023. The Deputy Secretary then endorsed a strategy for the military health system and set forth implementing guidance in a December 2023 memorandum, as previously discussed.[76]
More recently, the governance councils have considered gaps between health care supply and demand at medical facilities, and the risk to delivering safe patient care. According to senior DHA officials, the ability to supply health care across the military health system remains constrained by insufficient military and civilian medical personnel and fiscal resources. These officials stated that the Military Health System Executive Review Board would decide which facilities should temporarily discontinue certain types of health care services in 2025 due to insufficient staffing levels.
Quality information. As discussed earlier in this report, DOD developed a new tool to facilitate the monitoring of system-wide military health system staffing and medical facility work time. We identified concerns with the accuracy and completeness of data that Health Affairs will use to monitor facility work time of military medical personnel in facilities. Notwithstanding concerns about particular data elements, the overall monitoring approach is effective in combination with other information sources used for oversight because Health Affairs and military health system governance councils use a variety of other data sources from DHA and the military departments to monitor staffing. These sources include the military departments’ data on their respective numbers of positions authorized for military medical personnel at medical facilities and those authorized for operational and other unit types.
Health Affairs also uses the military departments’ data to validate information from DOD’s Health Manpower and Personnel Data System. Health Affairs then produces annual statistical reports with these data to illustrate any shortfalls or surpluses among military medical personnel by occupational specialty, and by corps and military service, among other characteristics.
Conclusions
Military medical personnel staffing at DOD’s medical facilities has declined since 2015. Moreover, a series of challenges facing DOD have exacerbated long-standing facility staffing issues. Namely, the historic transition of facilities from the military departments to DHA resulted in a complex workforce management structure with competing demands for a constrained military medical personnel supply needed to staff more than 700 DHA-managed facilities, along with operational and other unit types. Concurrently, inflationary pressures and a challenging health care economy have further strained the military health care system by limiting the ability to augment military medical personnel with civilian and contractor personnel.
In the face of these challenges, DOD has made progress toward improving its workforce management by implementing a new and collaborative staffing process to help identify the personnel needed at medical facilities and reach agreement on their distribution. DOD has also taken steps to monitor available work time for personnel in the facilities by, for example, setting expectations for work time based on personnel categories—that is, whether military medical personnel are assigned exclusively to facilities or are also assigned to other units.
However, DOD’s medical workforce monitoring tool is missing key information and accurate and complete source data from the timecard system. By making key distinctions between facility and non-facility work time and among personnel categories in the tool, DOD can better ensure that military medical personnel are meeting their expected available work time. DOD needs this information to make tradeoffs between military personnel time spent in its facilities versus time spent on military activities. In addition, taking actions to improve data quality by establishing a clear and consistent communication strategy with military departments’ medical personnel on timecard data importance, analyzing and addressing root causes of data quality issues, issuing policy, and requiring all personnel to complete a timecard in compliance with a 2022 DOD memorandum, will help provide DOD the information it needs to better monitor staffing. In combination with DOD’s broader oversight framework, the department will be better positioned to ensure it achieves its goal of stabilizing and improving the health system.
Recommendations
We are making the following seven recommendations to DOD:
The Secretary of Defense should ensure that the Assistant Secretary of Defense for Health Affairs, in coordination with the Director, DHA, evaluates activity codes used in DHA’s timecard system to determine which ones will count towards expectations for medical facility work time versus those that will not. (Recommendation 1)
The Secretary of Defense should ensure that the Assistant Secretary of Defense for Health Affairs works to categorize military medical personnel working within medical facilities within its monitoring tool with a variable to identify them by personnel category (e.g., exclusive, dual-assigned, periodic-intermittent). (Recommendation 2)
The Secretary of Defense should ensure that the Director, DHA, develops and disseminates a clear and consistent communication strategy, geared toward medical personnel from the military departments, to increase their understanding of the importance of timecard data and how it is used. (Recommendation 3)
The Secretary of Defense should ensure that the Director, DHA, analyzes and addresses root causes of data quality issues with military medical facility timecard data and implements any findings. (Recommendation 4)
The Secretary of the Army should issue a policy requiring all military medical personnel to complete a timecard when working in a medical facility. (Recommendation 5)
The Secretary of the Navy should issue a policy requiring all military medical personnel to complete a timecard when working in a medical facility. (Recommendation 6)
The Secretary of the Air Force should issue a policy requiring all military medical personnel to complete a timecard when working in a medical facility. (Recommendation 7)
Agency Comments
We provided a draft of this report to DOD for review and comment. The department’s comments are reprinted in appendix II. In written comments, DOD concurred with our recommendations and identified steps it plans to take. DOD also provided technical comments, which we incorporated as appropriate.
We are sending copies to the appropriate congressional committees, the Secretary of Defense, the official Performing the Duties of the Under Secretary of Defense for Personnel and Readiness, the Acting Assistant Secretary of Defense for Health Affairs, the Acting Director of the Defense Health Agency, and the Secretaries of the Army, the Navy, and the Air Force. In addition, the report is available at no charge on the GAO website at http://www.gao.gov.
If you or your staff have any questions about this report, please contact me at agarwalr@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix III.

Rashmi Agarwal
Acting Director, Defense Capabilities and Management
The Senate Report accompanying a bill for the National Defense Authorization Act for Fiscal Year 2024 includes a provision for us to review military medical personnel staffing at the Department of Defense’s (DOD) medical facilities.[77] In this report, we describe (1) trends in staffing military medical personnel to DOD medical facilities from fiscal year 2015 through fiscal year 2023; and evaluate the extent to which DOD has (2) a collaborative process to staff facilities, (3) taken steps to monitor the availability of personnel to work in medical facilities, and (4) an effective framework to oversee military medical personnel staffing at its facilities.
For objective one, we analyzed data from the Army, Navy, and Air Force on their assigned active component military medical personnel, comparing them with data on authorized active component positions (i.e., positions identified in DOD data as approved and funded) for military medical personnel from fiscal year 2015 through fiscal year 2023. We selected fiscal year 2015 to provide 2 years of data before the enactment of a statutory requirement transferring administration and management of medical facilities to the Defense Health Agency (DHA). Fiscal year 2023 was the most recent year of complete staffing data available from the military departments during our review. DOD also authorizes medical facility positions for civilian employees and uses contractors to fill vacant positions authorized for military or civilian personnel. Data on civilian employees and contractors were outside our scope, as were non-medical positions for military personnel in medical facilities (e.g., chaplains and food service workers).
For authorized military medical positions and assigned military medical personnel, we obtained and used record-level data sets from military department databases for fiscal year 2015 through fiscal year 2023. Each fiscal year dataset reflected a point in time at the end of the fiscal year in September except for the Army, for which assigned personnel are as of October. Further, each dataset we reviewed included military medical positions in active component units that are part of medical facilities and non-medical facility units. Medical facilities include inpatient hospitals and medical centers, ambulatory care and occupational health clinics, and dental clinics. Non-medical facility units include operational units (e.g., Army medical brigades; Navy ships; Air Force aeromedical evacuation squadrons; Marine Corps battalions), and headquarters organizations. The authorized positions and assigned personnel databases are shown in table 1 by military department.
|
Military department |
Authorized positions database |
Assigned personnel database |
|
Armya |
Force Management System Web |
Medical Operational Data System electronic Total Officer Personnel Management Information System |
|
Navy |
Total Force Manpower Management System |
Navy Standard Integrated Personnel System |
|
Air Force |
Manpower Programming and Execution System |
Military Personnel Data System |
Source: GAO analysis of military department database information. | GAO‑25‑106988
aFor the Army, we calculated counts of personnel records using both provided datasets, which varied in their level of detail and completeness. We compared the results from each dataset for consistency and selected the Medical Operational Data System dataset for assigned personnel counts for all but fiscal year 2019 because of its completeness for our purposes of reporting counts by category, including dual-assigned. We selected the electronic Total Officer Personnel Management Information System to calculate a subset of personnel assignment counts—specifically those for officers—for fiscal year 2019 because data that year were more complete, with fewer missing values.
For each data set, we excluded any reserve personnel, civilian medical employees, and non-medical personnel.[78] For records within our scope (i.e., active component medical personnel), we used input from military department officials to assign each record (position and assigned personnel) to one of the following three categories based on unit name: (1) medical facility; (2) non-medical facility; and (3) dual-assigned. Medical facility and non-medical facility units are described above. Dual-assigned is a term we use to describe the subset of positions and assigned personnel that were aligned with an operational unit and a medical facility at the same time.[79]
We calculated counts of position records and personnel records for each military department by category (i.e., medical facility, dual-assigned, non-medical facility) and for each fiscal year. For each military department, we shared the results with medical headquarters officials for review and incorporated their feedback as appropriate.
We combined the military department counts of positions and personnel by category and by fiscal year to calculate department-wide totals. In doing so, we grouped positions and personnel from the dual-assigned subcategory into the medical facility category for the Navy and the Air Force or the non-medical facility category for the Army. According to medical headquarters officials, doing so is consistent with the administrative grouping of these positions and personnel in their respective military departments.
To assess the reliability of the positions and personnel data, reviewed documentation on the source databases, interviewed military department officials about the data and any limitations, tested the data for any errors or omissions, and compared the data with other sources. We determined the data were sufficiently reliable for determining staffing trends over time by unit type.
To understand the extent to which shortfalls have occurred among personnel in military medical occupational specialties, we obtained and analyzed DOD’s Health Manpower Personnel Data System Fiscal Year Statistics reports. Specifically, we reviewed reports for fiscal year 2019 through fiscal year 2023 to analyze trends over time for the more recent half of our in-scope time period for the medical position and personnel (i.e., staffing) analysis described above. We used these reports instead of the military departments’ position and personnel data because the reports provide common groupings and names of specialties that vary among the military departments. We compared the authorized positions for each medical occupational specialty with the numbers of personnel serving in the specialties to identify any consistent gaps over the time period. We assessed the reliability of the data by reviewing DOD guidance about the database and reports, reviewing our prior reports that used the data, and asking questions of officials from the Office of the Secretary of Defense for Health Affairs, which oversees the database and reports. We found the data to be sufficiently reliable for reporting shortages in military medical specialties.
To supplement our understanding of staffing trends and inform our other objectives, we visited, in person, a nongeneralizable sample of six US-based medical facilities and interviewed approximately 350 facility personnel, including doctors, nurses, x-ray and laboratory technicians, pharmacists, administrative staff, and facility leaders. The selected facilities included Tripler Army Medical Center (Hawaii), Guthrie Ambulatory Care Center (Ft. Drum, New York), Naval Medical Center Portsmouth (Virginia), Naval Medical Center Camp Lejeune (North Carolina), the 673rd Medical Group (Joint Base Elmendorf-Richardson, Alaska), and the 27th Special Operations Medical Group (Cannon Air Force Base, New Mexico). We selected these six facilities to provide variation across multiple characteristics, including the market type of each facility; military department affiliation; the presence of graduate medical education; the presence of co-located operational units; patient volume; and facility size.[80] At each facility, we spoke with personnel in clinical, management, and administrative positions. The findings from these interviews are not generalizable to other personnel at these facilities or personnel at other facilities.
For objective two, we examined actions taken by DHA and the military departments to implement collaborative processes to staff medical facilities. We reviewed guidance directing DHA and the military departments to implement a collaborative process for making facility assignments as well as business rules outlining the process.[81] We reviewed documentation of actions taken to implement this staffing distribution process and results from fiscal year 2024 through fiscal year 2025 for facility assignments, including DHA’s analysis of facility staffing gaps and its communication of priority facility locations and specialties to the military departments. We also interviewed DHA and military department officials regarding their actions to implement the process and its results. We compared DHA and military department actions against selected leading practices for interagency collaboration, including the need for agencies to include relevant participants, clarify roles and responsibilities, identify and sustain leadership, bridge organizational cultures, and update written guidance and agreements in their collaborative efforts.[82]
We also examined DHA and military department efforts to develop updated medical facility staffing needs. Specifically, we reviewed guidance that outlines a process by which DHA and the military departments shall develop updated staffing needs for facilities.[83] We reviewed documentation on DHA’s development of planning models to identify facility staffing needs, and on its efforts to solicit feedback regarding facilities’ updated staffing needs. In addition, we reviewed a DHA planning document outlining a timeline for finalizing and documenting facility staffing requirements in accordance with guidance. We interviewed DHA and military department officials regarding these efforts.
For objective three, we examined factors affecting the availability of military medical personnel to work in their assigned medical facilities. Specifically, we analyzed locally maintained data on individual training requirements for fiscal year 2024 and deployments between January 2022 and December 2024 for personnel assigned to the 673rd Medical Group. We also analyzed locally maintained data on absences during fiscal year 2023 among dual-assigned military medical personnel at Tripler Army Medical Center due to operational unit training requirements. Furthermore, we reviewed prior DOD and GAO reports that have examined the impacts of these requirements. To understand the actions taken by DOD to improve military medical personnel availability to the facilities, we reviewed business rules issued by Health Affairs that establish notification requirements for military medical personnel absences from facilities and expectations for facility work time.
We also examined DOD’s ability to monitor military medical personnel medical facility work time against expectations outlined in DOD’s July 2024 business rules for managing and monitoring medical facility personnel work time.[84] Specifically, we reviewed Health Affairs’ monitoring tool to determine if it includes information that distinguishes 1) facility work time from non-facility work time and 2) between categories of military medical personnel working within medical facilities (e.g., exclusive, dual-assigned, and periodic-intermittent). We also interviewed Health Affairs officials about the development of the monitoring tool and the information it presents. We compared the information included in the monitoring tool against Standards for Internal Control in the Federal Government.[85] Specifically, we determined that the Information and Communication component of internal control was relevant to our review, including the principle that management should use quality information to achieve agency objectives by, for example, processing data into quality information that is appropriate, current, complete, accurate, accessible, and provided on a timely basis.
We also examined the accuracy and completeness of timecard data to be used in the tool to monitor availability. Specifically, we reviewed prior DOD reports on the reliability of DHA timecard data. We also analyzed timecard data to identify examples of inaccurate and incomplete data. Specifically, we analyzed record-level timecard data for fiscal year 2023 for personnel we interviewed who were assigned at four of the six selected facilities to identify recent data accuracy issues.[86] To identify examples of inaccuracies, we analyzed the data to identify facility-assigned military personnel that recorded time to a single activity during November 2022. We also analyzed timecards to identify facility-assigned military personnel that recorded less than or equal to 6 hours towards mandatory DHA training during fiscal year 2023. We limited our analyses to records of active duty, facility-assigned military personnel and excluded those of military personnel working in the facility on a temporary basis, as well as those of students, fellows, interns, residents, dental personnel, veterinary personnel, and personnel regularly performing activities unrelated to the facilities’ direct care mission. For our analysis of timecard data to identify facility-assigned personnel that recorded time to a single activity, we excluded personnel that charged fewer than 40 hours during November 2022. For our analysis of training hours, we excluded personnel that deployed during fiscal year 2023. To identify examples of incomplete timecard data, we identified military medical personnel that scheduled primary care appointments at Naval Medical Center Camp Lejeune or one of its associated clinics during October 2022 but did not submit a corresponding timecard. We found the scheduling data to be sufficiently reliable for this purpose but not for the purposes of describing hours worked by military medical personnel at medical facilities.
In addition to the work described above, we interviewed officials from Health Affairs and DHA regarding the accuracy and completeness of timecard data. We also interviewed personnel at all six medical facilities we visited regarding their perceptions of timecard data accuracy and completeness and challenges in completing a timecard. Included in these interviews were facility personnel who oversee timekeeping and are responsible for submitting the facilities’ timecard records. To understand actions taken to improve the accuracy and completeness of timecard data, we spoke with senior DHA officials and personnel responsible for managing the timekeeping system. We also interviewed military department officials regarding their efforts to ensure all military medical personnel complete a timecard when working in a facility.
We compared the accuracy and completeness of timecard data with a DOD instruction that states the quality of MHS data is critical to the effectiveness of performance-based management, resource allocation, decision-making at all levels, and many other operations and management activities across the system.[87] We also compared the reliability of timecard data with Standards for Internal Control in the Federal Government.[88] Specifically, we determined that the Information and Communication component of internal control was relevant to our review, including the principle that management should use quality information to achieve agency objectives by, for example, using relevant data from reliable sources. We determined the timecard data were not sufficiently accurate or complete to describe hours worked by military medical personnel at medical facilities. Therefore, we are not using the data to report how military medical personnel spend their time.
For our fourth objective, we reviewed and analyzed DOD guidance, memorandums, and reports. We also reviewed meeting minutes and briefings from military health system governance councils, and interviewed senior officials from the Office of the Assistant Secretary of Defense for Health Affairs and DHA. We compared this information with key elements of business and financial management systems oversight. These include establishing oversight processes, sustaining leadership commitment, managing risk, and using and communicating quality information.[89]
We conducted this performance audit from July 2023 to July 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
GAO Contact
Rashmi Agarwal, agarwalr@gao.gov
Staff Acknowledgments
In addition to the contact named above, Lori Atkinson (Assistant Director), Melissa Blanco (Analyst in Charge), Sharon Ballinger, Vincent Buquicchio, Caitlin Cusati, Alexandra Gonzalez, Joyce Harvey, Jesse Jordan, Tara Porter, Stephanie Santoso, and Lillian Moyano Yob made key contributions to this report.
Related GAO Products
Defense Health Care: DOD Should Reevaluate Market Structure for Military Medical Treatment Facility Management. GAO‑23‑105441. Washington, D.C.: August 21, 2023.
Defense Health Care: Additional Assessments Needed to Determine Effects of Active Duty Medical Personnel Reductions. GAO‑23‑106094. Washington, D.C.: July 11, 2023.
Defense Health Care: Improved Monitoring Could Help Ensure Completion of Mandated Reforms. GAO‑23‑105710. Washington, D.C.: June 22, 2023.
Defense Health Care: Actions Needed to Define and Sustain Wartime Medical Skills for Enlisted Personnel. GAO‑21‑337. Washington, D.C.: June 17, 2021.
Defense Health Care: Additional Information and Monitoring Needed to Better Position DOD for Restructuring Medical Treatment Facilities. GAO‑20‑371. Washington, D.C.: May 29, 2020.
Defense Health Care: DOD Should Collect and Use Key Information to Make Decisions about Incentives for Physicians and Dentists. GAO‑20‑165. Washington, D.C.: January 15, 2020.
Defense Health Care: Additional Assessments Needed to Better Ensure an Efficient Total Workforce. GAO‑19‑102. Washington, D.C.: November 27, 2018.
Military Personnel: Additional Actions Needed to Address Gaps in Military Physician Specialties. GAO‑18‑77. Washington, D.C.: February 28, 2018.
Defense Health Care Reform: DOD Needs Further Analysis of the Size, Readiness, and Efficiency of the Medical Force. GAO‑16‑820. Washington, D.C.: September 21, 2016.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on X,
LinkedIn, Instagram, and YouTube.
Subscribe to our Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System (Dec. 6, 2023). The total number of medical facilities includes 45 inpatient hospitals and medical centers, 574 ambulatory care and occupational health clinics, and 117 dental clinics. For the purposes of this report, unless otherwise specified, we use the term “medical facilities” to include both medical and dental facilities. DOD refers to its medical facilities as “military medical treatment facilities.”
[2]DOD found that the deployment of military medical personnel from its medical facilities during the COVID-19 pandemic created gaps in staffing that resulted in the reduction of clinical and public health services. The COVID-19 pandemic also stressed DOD’s overseas facilities that relied heavily on local private sector care networks. Under Secretary of Defense for Personnel and Readiness, Report to the Congressional Defense Committees: COVID-19 Military Health System Review Panel (Mar. 10, 2023), in response to Pub. L. No. 116-283, § 731 (2021).
[3]Section 702 of Public Law 114-328 (codified as amended at 10 U.S.C. § 1073c) was enacted December 23, 2016 and required the transfer of administration and management of medical facilities to DHA.
[4]Since fiscal year 2016, the Defense Health Program budget, including medical facility operations, has remained generally constant when adjusted for inflation. In addition, DOD leaders have continued to apply budget constraints for future years that DHA must operate within by further reducing operating costs during a period of rising inflation.
[5]GAO, Defense Health Care: Additional Assessments Needed to Determine Effects of Active Duty Medical Personnel Reductions, GAO‑23‑106094 (Washington, D.C.: July 11, 2023). In November 2018, as DOD was planning to carry out the transition of medical facilities to DHA, we reported that the military departments faced challenges implementing their workforce mix of military, civilian, and contractor personnel in the facilities. We found that several challenges, such as lengthy hiring and contracting processes, affected DOD’s ability to use federal civilians and contractors to fill facility positions. We recommended that the DHA Director develop a strategic total workforce plan. As of March 2025, DHA had not yet developed a plan. GAO, Defense Health Care: Additional Assessments Needed to Better Ensure an Efficient Total Workforce, GAO‑19‑102 (Washington, D.C.: Nov. 27, 2018).
[6]TRICARE is DOD’s regionally structured health care program, allowing beneficiaries to obtain health care services through DOD’s direct care system of medical facilities or through private-sector care comprising civilian network providers.
[7]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System. In May 2020, we reported that a DOD plan to reduce capabilities at 43 medical facilities and close five other facilities was based on incomplete and inaccurate information, including that DOD may have overestimated the adequacy of civilian health care providers in proximity to some facilities and overestimated the cost-effectiveness of such care. GAO, Defense Health Care: Additional Information and Monitoring Needed to Better Position DOD for Restructuring Medical Treatment Facilities, GAO‑20‑371 (Washington, D.C.: May 29, 2020).
[8]GAO, Defense Health Care: DOD Should Reevaluate Market Structure for Military Medical Treatment Facility Management. GAO‑23‑105441 (Washington, D.C.: Aug. 21, 2023).
[9]Specifically, the transition plans did not include the development of policies and procedures for assigning military personnel to the facilities or mitigating the effect of deployments on facility operations. GAO‑19‑102.
[10]S. Rep. No. 118-58, at 166-67 (2023).
[11]In this report, we use the term “staffing” to mean assigning military medical personnel from the military departments with orders for primary duty at a medical facility to fill a vacant position for a length of time, or generally 3 years. We use the term “workforce management” to include information and decisions about staffing and personnel availability for medical facilities (i.e., the amount of time personnel spend working in facilities).
[12]Pub. L. No. 114-328 was enacted December 23, 2016.
[13]We interviewed military medical personnel from the following medical facilities: Tripler Army Medical Center (HI), Guthrie Ambulatory Care Center (Ft. Drum, NY), Naval Medical Center Portsmouth (VA), Naval Medical Center Camp Lejeune (NC), the 673rd Medical Group (Joint Base Elmendorf-Richardson, AK), and the 27th Special Operations Medical Group (Cannon Air Force Base, NM). The findings from these interviews are not generalizable to other personnel at these facilities or personnel at other facilities.
[14]On October 1, 2023, DHA began efforts to replace the market structure with a network organizational structure to manage its medical facilities. Section 714 of the National Defense Authorization Act for Fiscal Year 2024 delayed DOD’s implementation of the network structure until we report on DHA’s transition efforts to date.
[15]GAO, Government Performance Management: Leading Practices to Enhance Interagency Collaboration and Address Crosscutting Challenges, GAO‑23‑105520 (Washington, D.C.: May 24, 2023).
[16]To ensure a large number of timecard records after applying parameters to our analysis, we limited our analysis to medical centers and hospitals by excluding the two outpatient clinics, which have a smaller number of personnel.
[17]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: September 2014).
[18]Department of Defense Instruction 6040.40, Military Health System (MHS) Data Quality Management Control (DQMC) Program (Dec. 27, 2019).
[19]GAO, Financial Management: DOD Needs to Improve System Oversight, GAO‑23‑104539 (Washington, D.C.: Mar. 7, 2023).
[20]Department of Defense Directive 5124.02, Under Secretary of Defense for Personnel and Readiness (USD(P&R)) (June 23, 2008) (incorporating change 1, Dec. 11, 2024).
[21]Department of Defense Directive 5136.01, Assistant Secretary of Defense for Health Affairs (ASD(HA)) (Sept. 30, 2013) (incorporating change 1, Aug. 10, 2017).
[22]The DOD unified medical program consists of the Defense Health Program appropriation request, military personnel costs, military construction costs, and the estimated payments to the DOD Medicare-Eligible Retiree Health Care Fund.
[23]TRICARE offers a variety of plan options, and most beneficiaries are enrolled in either TRICARE Prime or TRICARE Select. While active duty service members are automatically enrolled in TRICARE Prime, others may select a plan option during an annual open enrollment period. TRICARE Prime is a health maintenance organization-style option in which beneficiaries typically receive most of their care through a primary care manager at a local DOD medical facility. If the facility is unable to provide a necessary service, the primary care manager refers the beneficiary to obtain this care from TRICARE’s network of civilian providers. TRICARE Select is a self-managed, preferred provider organization option that allows beneficiaries flexibility in managing their own health care. Beneficiaries with TRICARE Select may obtain covered services from any TRICARE-authorized provider.
[24]Department of Defense Directive 5136.13, Defense Health Agency (Sept. 30, 2013) (incorporating change 2, Sept. 12, 2023).
[25]Department of Defense Instruction 6000.19, Military Medical Treatment Facility Support of Medical Readiness Skills of Health Care Providers (Feb. 7, 2020).
[26]Each military department’s assignment processes must observe broader DOD requirements, such as standardized lengths of overseas assignments and time on station requirements.
[27]These numbers represent the combined total positions and personnel of each military department’s medical positions and personnel in medical facilities. The scope of our data analysis was limited to positions authorized for and filled by military medical personnel. DOD also authorizes medical facility positions for civilian personnel and uses contractor personnel to fill vacant positions authorized for military or civilian personnel, where appropriate. Data on civilian employees and contractors were outside our scope, as were non-medical positions for military personnel in medical facilities (e.g., chaplains and food service workers).
[28]According to Army and Navy officials, staffing levels sometimes exceeded 100 percent of authorized personnel for a few reasons. For example, there were more assignable personnel to distribute across authorized positions in earlier years over the period we reviewed because recruitment and retention were better in those years than in more recent years.
[29]In fiscal year 2019, the Army began aligning its dual-assigned positions and personnel primarily to an operational unit, such as a combat support hospital or medical brigade. These personnel are known as Modified Table of Organization and Equipment Assigned Personnel. They are assigned duty at a medical facility, where they are expected to spend most of their time when not deployed. Prior to the change, the Army sourced its medical personnel for operational units by selecting from medical personnel who were assigned to medical or research facilities. Unlike the Army, according to Navy officials, the Navy’s dual-assigned medical personnel are assigned primarily to a medical facility position with an operational unit association, and report to a dual-hatted facility director/Navy Medicine Readiness and Training Command commander until they mobilize for deployment with an operational unit. Once “dual-assigned” personnel are deployed, they report to a combatant commander. Likewise, Air Force dual-assigned personnel are assigned to a medical facility position and report to a dual-hatted facility director/Air Force medical group commander until they mobilize for deployment with an operational unit.
[30]Defense Health Agency, Evaluation of the TRICARE Program: Fiscal Year 2016 Report - Access, Cost, and Quality, Fiscal Year 2016 Report to Congress (Feb. 24, 2016) and Defense Health Agency, Evaluation of the TRICARE Program: Fiscal Year 2024 Report, Access, Cost, and Quality Data through Fiscal Year 2023 (Feb. 29, 2024).
[31]Each military department implemented its own downsizing initiatives prior to the transition of medical facilities to DHA from 2019 through 2022. These initiatives preceded a February 2020 DOD plan to decrease capabilities at 43 medical facilities and close five. That plan was put on hold at the start of the COVID-19 pandemic and has not been implemented.
[32]DOD first proposed its plan to Congress in its budget request for fiscal year 2020. The National Defense Authorization Act for Fiscal Year 2020 set forth certain conditions that DOD must satisfy prior to reducing or realigning any military medical billets not listed as exceptions in the statute. Pub. L. No. 116–92, § 719 (2019). The act also required DOD to develop a plan for such reductions. In response, in fiscal year 2021, DOD submitted a revised plan to Congress describing proposed reductions and realignments of 12,801 medical facility positions. This number included 10,739 military medical positions that would be reduced and 375 positions that would be realigned as a different medical position. The remaining positions were for non-medical personnel (e.g., chaplains, law enforcement, food service workers) or students. The National Defense Authorization Acts for Fiscal Year 2021 through Fiscal Year 2023 delayed the reductions until December 2027. Pub. L. No. 116-283, § 717 (2021); Pub. L. No. 117-81, § 731(a)(1) (2021); and Pub. L. No. 117-263, § 741(a)(1) (2022). In July 2023, we reported that DOD had not fully or consistently assessed the effects the potential reductions may have on its medical facilities and on the TRICARE networks and did not fully define active duty medical personnel requirements prior to determining military medical personnel reductions. We made nine recommendations to DOD. DOD concurred with the recommendations but has not implemented them as of February 2025. GAO‑23‑106094.
[33]Under Secretary of Defense for Personnel and Readiness, Report to the Congressional Defense Committees, COVID-19 Military Health System Review Panel (Mar. 10, 2023).
[34]A DHA official explained that the collaborative process does not determine individual assignments of military medical personnel. Rather, DHA and the military departments collaborate to determine the military departments’ ability to provide military medical personnel to fill clinical gaps in medical facilities. These gaps are measured as full-time equivalents, which DHA defines as one employee working full-time for a specified period that can be made up of several part-time individuals or one full-time individual.
[35]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Assignment (June 28, 2024).
[36]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules (July 1, 2024).
[37]The military departments record military medical personnel assignments—including assignments to medical facilities—in their respective personnel management databases. DHA records military medical personnel assignments to medical facilities in its timekeeping system.
[38]DHA’s estimated shortfall is based on full-time equivalents and does not include gaps in civilian personnel or administrative, logistics, or clerical military medical personnel.
[39]Our prior work established eight leading practices to help enhance and sustain collaboration among federal agencies: (1) define common outcomes; (2) ensure accountability; (3) bridge organizational cultures; (4) identify and sustain leadership; (5) clarify roles and responsibilities; (6) include relevant participants; (7) leverage resources and information; and (8) develop and update written guidance and agreements. We assessed DHA and the military departments against practices 3, 4, 5, 6, and 8 because we determined that they were most relevant to aspects of the medical facility staffing process described in our report. GAO‑23‑105520.
[40]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System.
[41]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Assignment. DOD’s process to plan for the resources it will need across the 5-year period is known as “programming.”
[42]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System.
[43]According to DHA leaders, because DHA and the military departments have completed budget and program inputs for fiscal year 2026, they will use the results of these efforts for the first time to inform the budget and programming processes for fiscal year 2027 and thereby develop the authorized personnel.
[44]Under Secretary of Defense for Personnel and Readiness Memorandum, Transparency of Military Medical Personnel and Clinical Readiness Data (Aug. 8, 2022); Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System.
[45]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Assignment. The Under Secretary of Defense for Personnel and Readiness issued Directive-Type Memorandum 24-003 in response to the Deputy Secretary of Defense’s memorandum, Stabilizing and Improving the Military Health System. Directive-Type Memorandum 24-003 directed Health Affairs to develop business rules to execute procedures for military medical personnel absences from medical facilities and their availability. Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Notification Business Rules (July 1, 2024). Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Staffing Transparency and Resourcing Impact Business Rules (July 1, 2024). Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules.
[46]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Notification Business Rules. While the Army previously maintained notification requirements for its dual-assigned personnel, the new business rules implement notification requirements for all military medical personnel assigned to a medical facility.
[47]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules. Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Staffing Transparency and Resourcing Impact Business Rules.
[48]Military medical personnel can meet some of their sustainment training requirements through the performance of normal duties within a medical facility.
[49]Department of Defense, Report on Military Health System Modernization: Response to Section 713 of the Carl Levin and Howard P. “Buck” McKeon National Defense Authorization Act for Fiscal Year 2015 (P.L. 113-291) (Feb. 8, 2016).
[51]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Staffing Transparency and Resourcing Impact Business Rules. As a part of its monitoring, Health Affairs will also stratify its analysis by medical occupational specialty, military service, and location.
[52]A workgroup began developing the tool in 2023 pursuant to a memorandum from the Under Secretary of Defense for Personnel and Readiness. Under Secretary of Defense for Personnel and Readiness Memorandum, Transparency of Military Medical Personnel and Clinical Readiness Data.
[53]DOD’s timecard system is called the “Defense Medical Human Resources System – internet.” DHA Procedures Manual 6010.13, Volume 1 states that medical facility personnel must ensure their labor hours are distributed to the appropriate work center, which is accomplished in DHA’s timecard system. Defense Health Agency Procedures Manual 6010.13, Volume 1, Medical Expense and Performance Reporting System (MEPRS) for Fixed Military Medical and Dental Treatment Facilities (DTFs): Business Rules (Sept. 27, 2018).
[54]For fiscal year 2024, there were more than 1,000 unique activity codes in the timecard system for facility personnel to choose from and record hours of work or leave.
[56]Department of Defense, Report on Military Health System Modernization: Response to Section 713 of the Carl Levin and Howard P. “Buck” McKeon National Defense Authorization Act for Fiscal Year 2015 (P.L. 113-291).
[57]U.S. Army Audit Agency, Tracking Army Medical Personnel Time at Medical Treatment Facilities, Report A-2024-0076-FIZ (Sept. 12, 2024). As a part of its review, the Army Audit Agency reviewed a nongeneralizable sample of timecard data from five medical facilities for Army military medical personnel only. Therefore, findings from the review cannot be generalized to data from other facilities or non-Army military medical personnel.
[58]The Health Affairs’ monitoring tool also provides such data from month-to-month, showing the percentages of assigned medical facility personnel that did not complete a timecard, broken out by military department and by officer, enlisted, and civilian personnel.
[59]To ensure a large number of timecard records after applying parameters to our analysis, we limited our analysis to medical centers and hospitals by excluding the two clinics, which have a smaller number of assigned military medical personnel.
[60]All 44 of these personnel were in the periodic-intermittent personnel category as described above and were not assigned to the facility.
[61]Defense Health Agency Procedures Manual 6010.13, Volume 1.
[63]DOD Instruction 6040.40, Military Health System (MHS) Data Quality Management Control (DQMC) Program.
[65]Defense Health Agency Procedures Manual 6010.13, Volume 1.
[66]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules.
[67]Under Secretary of Defense for Personnel and Readiness Memorandum, Transparency of Military Medical Personnel and Clinical Readiness Data.
[69]DOD Directive 5136.01, Assistant Secretary of Defense for Health Affairs (ASD(HA)). According to DOD Directive 5136.01, the Assistant Secretary of Defense for Health Affairs exercises authority, direction, and control over DOD medical and dental personnel authorizations and policy, as well as funding. For example, the Assistant Secretary serves as resource manager for the department by preparing and submitting annually to the DOD Comptroller a DOD Unified Medical Program budget to provide resources for the military health system.
[70]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Assignment.
[71]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules; and Assistant Secretary of Defense for Health Affairs Memorandum Military Health System Staffing Transparency and Resourcing Impact Business Rules.
[72]If the Senior Military Medical Advisory cannot reach consensus on an issue, the Assistant Secretary and military departments may raise it to the Under Secretary of Defense for Personnel and Readiness for review and decision through the Military Health System Executive Review Board, which is the highest-level governing body.
[73]Deputy Secretary of Defense Memorandum, Department of Defense Fiscal Year 2023-2024 Priority Cross-Cutting Performance Improvement Initiatives (Aug. 4, 2023).
[74]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System.
[75]In July 2023, we reported on deficiencies in DOD’s planning for potential military medical personnel reductions and made nine recommendations to inform its decision-making. DOD concurred with the recommendations but had not implemented them as of April 2025. GAO‑23‑106094.
[76]Deputy Secretary of Defense Memorandum, Stabilizing and Improving the Military Health System.
[77]S. Rep. No. 118-58, at 166-67 (2023). For the purposes of this report, unless otherwise specified, we use the term “medical facilities” to include both medical and dental facilities. DOD refers to these facilities as “military medical treatment facilities.”
[78]Non-medical personnel include those serving in occupational specialties outside the health care corps of the military departments, such as chaplains and food service workers, that are part of medical facilities.
[79]Each military department has different terms for dual-assigned medical positions and personnel, or their units, which include Modified Table of Organization and Equipment Assigned Personnel (Army); Expeditionary Medicine System (Navy); and operational medical Unit Type Codes (Air Force). The Air Force was unable to provide data on which positions and personnel were dual-assigned because, according to officials, the data are recorded in separate systems and historical records are not maintained. To approximate the dual-assigned positions in fiscal year 2023, the Air Force provided a spreadsheet that was current as of December 2023 showing the number of dual-assigned positions by location, which we used to estimate fiscal year 2023 positions aligned to medical facilities. The Air Force was unable to provide data with which to estimate the number of personnel assigned to those positions in fiscal year 2023.
[80]DOD defined a market as a group of medical facilities that operate as a system, sharing patients, health care providers, functions, budgets, and a market office for management, across facilities. On October 1, 2023, DHA began efforts to replace the market structure with a network organizational structure to manage its medical facilities. Section 714 of the National Defense Authorization Act for Fiscal Year 2024 delayed DOD’s implementation of the network structure beyond its current phase until we report on DHA’s transition efforts to date.
[81]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Alignment (June 28, 2024). Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Human Capital Distribution Plan Business Rules (July 1, 2024).
[82]Our prior work established eight leading practices to help enhance and sustain collaboration among federal agencies: (1) define common outcomes; (2) ensure accountability; (3) bridge organizational cultures; (4) identify and sustain leadership; (5) clarify roles and responsibilities; (6) include relevant participants; (7) leverage resources and information; and (8) develop and update written guidance and agreements. We assessed DHA and the military departments against practices 3, 4, 5, 6, and 8 because we determined that they were most relevant to aspects of the medical facility staffing process described in our report. GAO, Government Performance Management: Leading Practices to Enhance Interagency Collaboration and Address Crosscutting Challenges, GAO‑23‑105520 (Washington, D.C.: May 24, 2023).
[83]Under Secretary of Defense for Personnel and Readiness Directive-Type Memorandum 24-003, Military Health System Manpower Requirements Determination, Resourcing, and Assignment.
[84]Assistant Secretary of Defense for Health Affairs Memorandum, Military Health System Staffing Transparency and Resourcing Impact Business Rules (July 1, 2024).
[85]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: September 2014).
[86]DOD’s timecard system is called the “Defense Medical Human Resources System – internet.” To ensure a large number of timecard records after applying parameters to our analysis, we limited our analysis to medical centers and hospitals by excluding the two clinics, which have a smaller number of assigned military medical personnel.
[87]Department of Defense Instruction 6040.40, Military Health System (MHS) Data Quality Management Control (DQMC) Program (Dec. 27, 2019).
[89]GAO, Financial Management: DOD Needs to Improve System Oversight, GAO‑23‑104539 (Washington, D.C.: Mar. 7, 2023).
