VETERANS HEALTH CARE
Actions Needed to Improve the Foreign Medical Program
Report to Congressional Committees
United States Government Accountability Office
View GAO‑25‑107149. For more information, contact Alyssa M. Hundrup at (202) 512-7114 or HundrupA@gao.gov.
Highlights of GAO‑25‑107149, a report to congressional committees
Actions Needed to Improve the Foreign Medical Program
Why GAO Did This Study
Thousands of veterans live in or travel to foreign countries each year. For qualifying medical expenses incurred abroad, veterans, or the providers that deliver services, may submit claims to VHA’s Foreign Medical Program for reimbursement.
The Consolidated Appropriations Act, 2023, includes a provision for GAO to review the VHA Foreign Medical Program. This report addresses available data on program claims, VHA processes for reimbursing claims, program staffing, and the extent to which fraud risk management activities for the program are consistent with selected leading practices.
GAO reviewed data on claims processed for fiscal years 2018 through 2024 and relevant program policies and documentation; assessed the program’s processes against criteria, such as human capital management key practices and GAO’s Fraud Risk Framework; and interviewed agency officials, veterans who use the program, and five veterans service organizations. GAO conducted interviews with veterans in person and obtained written responses via email.
What GAO Recommends
GAO is making nine recommendations to VHA, including that it finalize and prioritize implementation of the steps to transition to electronic funds transfers, evaluate and implement strategies to help mitigate staffing challenges, and follow leading practices for addressing the elements for assessing fraud risks. VA concurred with the recommendations and identified steps VHA plans to take to implement them.
What GAO Found
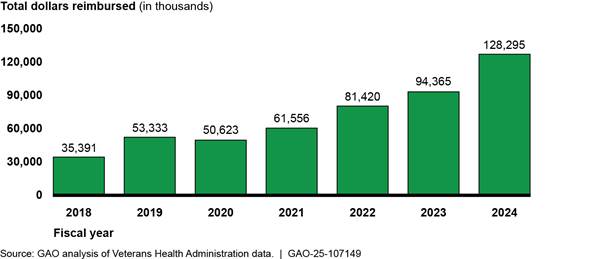
The Department of Veterans Affairs (VA) is responsible for providing benefits to veterans. Within VA, the Veterans Health Administration (VHA) provides health care benefits to eligible veterans with service-connected disabilities living or traveling abroad through its Foreign Medical Program. In fiscal year 2024, VHA data show the program paid $128.3 million in reimbursements to 8,024 veterans or their providers, representing a 263 percent increase in reimbursements since fiscal year 2018. In fiscal year 2024, the program reported processing 37 percent of claims within 45 days; its goal is to process 90 percent within that time.
Foreign Medical Program Reimbursements, Fiscal Years 2018 through 2024
The Foreign Medical Program makes reimbursements using paper checks, despite a federal law generally calling for electronic payments. Reliance on paper checks has resulted in challenges, including delayed or lost checks, according to officials. VA has begun a transition to an electronic payment method, but when or how the transition will occur is unclear. Implementing the new method will help ensure the timeliness and security of reimbursements.
VHA increased its authorized staffing in August 2023 from 25 to 38 positions for the Foreign Medical Program to help meet its timeliness goal. However, 14 positions remained vacant in 2024 due to various reasons, including a VHA zero-growth hiring policy, according to officials. VHA has taken some steps to help with hiring, such as allowing positions to be remote, but has not otherwise identified and evaluated staffing strategies. Evaluating and implementing such strategies could help the program address its staffing challenges and process claims in a timely manner.
VA has not comprehensively assessed fraud risks in the program in line with selected leading practices, despite evidence of potential fraud. This included VA suspending providers in 2024 due to their alleged involvement in a long-term fraud scheme. VHA developed two documents to outline efforts for fraud, waste, and abuse activities within VHA. However, VA has not implemented selected leading practices outlined in GAO’s Fraud Risk Framework. These include assigning an entity to lead and regularly assess fraud risks. Implementing such practices will help VA better prevent, detect, and respond to fraud.
|
Abbreviations |
|
|
|
|
|
VA |
Department of Veterans Affairs |
|
VHA |
Veterans Health Administration |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
February 19, 2025
The Honorable Jerry Moran
Chairman
The Honorable Richard Blumenthal
Ranking Member
Committee on Veterans’ Affairs
United States Senate
The Honorable Mike Bost
Chairman
The Honorable Mark Takano
Ranking Member
Committee on Veterans’ Affairs
House of Representatives
The Department of Veterans Affairs’ (VA) Veterans Health Administration (VHA) operates one of the nation’s largest health care systems, providing services to over 9 million enrolled veterans. In addition to providing services to veterans residing in the U.S., VHA provides health care benefits to eligible veterans with service-connected disabilities living or traveling abroad through its Foreign Medical Program.[1] Specifically, veterans and health care providers can submit claims to the Foreign Medical Program for services rendered abroad. The program is to then reimburse veterans or providers for qualified expenses.
VA estimates that approximately 80,000 veterans lived in foreign countries in fiscal year 2023. We previously reported that the number of disability claims for veterans living outside of the U.S. has increased, highlighting the importance of providing quality care for this population.[2]
In recent years, the Foreign Medical Program has faced challenges ensuring timely reimbursements. In 2019, we found that the program was not meeting its timeliness goal to process 90 percent of claims in 40 days; rather, we found it processed 70 percent of claims in 40 days, as of March 2019.[3] In 2024, citing concerns about inefficient and antiquated processes for submitting claims and 4 to 6 month delays for receiving reimbursements, a group of veterans began an effort to bring awareness about issues with the program.[4]
Additionally, the Foreign Medical Program has been susceptible to potential fraud. For example, in August 2024, VA suspended a group of medical providers in Panama from participating in the Foreign Medical Program due to their alleged involvement in a long-term fraud scheme, resulting in an estimated loss to VA of $67 million.[5]
The Consolidated Appropriations Act, 2023, includes a provision for us to review the VHA Foreign Medical Program.[6] In this report we
1. describe what available data show on Foreign Medical Program claims;
2. examine how the program processes and reimburses claims;
3. examine program staffing; and
4. examine the extent to which fraud risk management activities for the Foreign Medical Program are consistent with selected leading practices.
To describe available data on Foreign Medical Program claims, we obtained summary data from VHA on Foreign Medical Program claims processed for fiscal years 2018 through 2024 (the most recent data available at the time of our review). We analyzed these data by country to identify the number of claims paid, the amount reimbursed to veterans, the amount reimbursed to providers, and the total amount reimbursed. To assess the reliability of the VHA data we obtained, we interviewed relevant agency officials and reviewed related documentation, including claims processing guidance and data dictionaries. On the basis of these steps, we determined that the summary data were sufficiently reliable for the purposes of our audit objectives.
To examine how the program processes and reimburses claims, we reviewed agency documentation describing the claims review process, such as claims processing guidance and policies. We also received a claims processing system demonstration from Foreign Medical Program officials. Additionally, we examined a nongeneralizable selection of 19 claims processed during fiscal year 2023. We also assessed the program’s efforts to plan for the modernization of its claims processing system against government and industry leading practices for the modernization of legacy information technology identified in prior GAO work on modernization plans for legacy data systems.[7] We assessed the program’s reimbursement method against federal law generally requiring electronic payments.[8]
To examine staffing levels for the Foreign Medical Program, we reviewed agency documentation describing the program’s past and current organizational structures. We analyzed staffing information for positions that support the program, as of November 2024, to determine current staffing levels and vacancies. We assessed the extent to which VHA has strategies consistent with selected key practices for strategic human capital management.[9]
To examine the extent to which fraud risk management activities for the Foreign Medical Program are consistent with selected leading practices, we reviewed VA policies and fraud risk management activities related to the program.[10] We selected leading practices from the Commit and Assess components of GAO’s Fraud Risk Framework because establishing an organizational structure and identifying and assessing fraud risks are key initial steps in developing effective fraud risk management activities.[11] We reviewed relevant VA Office of Inspector General reports from fiscal years 2018 through 2024 to identify examples of fraud risks in the Foreign Medical Program. We also reviewed a report provided by VA’s Office of Business Oversight related to fraud risk management activities. We compared VA’s fraud risk management activities with selected leading practices in GAO’s Fraud Risk Framework.
Additionally, for all four objectives, we interviewed officials from the Foreign Medical Program who are responsible for managing data on program claims and for overseeing program operations, including staffing and fraud risk management activities. We interviewed officials from VHA’s Office of Integrated Veteran Care who are responsible for the provision of health care for veterans receiving care outside of VHA facilities, including through the Foreign Medical Program. We also interviewed officials from the VA Office of Information and Technology who are involved in claims processing and payment systems as well as officials from the VHA Office of Integrity and Compliance who are involved in identifying potential fraud in the Foreign Medical Program.
In addition, we interviewed representatives from five veterans service organizations (American Legion, Disabled American Veterans, Veterans of Foreign Wars, Vietnam Veterans of America, and Wounded Warrior Project) to gain their perspectives on the Foreign Medical Program. We also interviewed veterans in person at a veterans service organization convention in Germany in June 2024. We obtained and analyzed written feedback from 67 veterans representing 17 different countries on their experiences using the Foreign Medical Program. This feedback came from veterans who contacted us after we asked for input on the program in a veterans service organization newsletter. Information we obtained from these interviews and written feedback is not generalizable across veterans or veterans service organizations.
We conducted this performance audit from November 2023 to February 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Foreign Medical Program
After serving in the military, some veterans may choose to live or retire in a foreign country. For example, a veteran might decide to live abroad to be with family members, such as a spouse or child. Others may choose to live in a foreign country for a lower cost of living, including lower health care costs. In addition, other factors include career opportunities in U.S. civil service positions, foreign companies, veterans service organizations, or retiring in the location of their military service.
VHA’s Office of Integrated Veteran Care oversees the provision of health care for veterans receiving care outside of VHA facilities. Administered by the Office of Integrated Veteran Care, the Foreign Medical Program is responsible for providing benefits for eligible veterans living or traveling in a foreign country. These benefits are available to veterans with VA-rated service-connected disabilities and conditions associated with and held to be aggravating a service-connected disability (i.e., injuries or diseases incurred or aggravated in line of duty in the active military service).[12]
Generally, the Foreign Medical Program covers health care services, including hospitalization, outpatient care, emergency services, physical therapy, skilled nursing care, medications, and durable medical equipment.[13] The program can also cover prescription drugs if they are approved for marketing by the U.S. Food and Drug Administration, among other things.[14]
To raise awareness about program benefits, the program disseminates educational materials through a variety of methods, including
· a website that contains information on the program, including program eligibility, registration instructions, and instructions on how to file a claim for reimbursement;[15]
· two videos, released in 2024, that provide details on the Foreign Medical Program;[16] and
· informational briefings and brochures for veterans, providers, and veterans service organizations upon request.
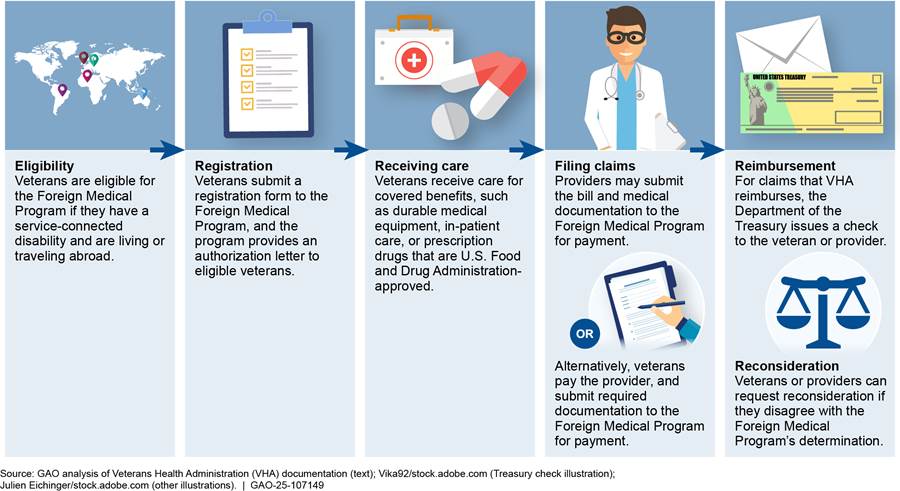
Veterans must first register with the Foreign Medical Program to determine their eligibility for reimbursement for medical services outside of the U.S. If eligible, they may then submit claims to the program office for reimbursement for covered expenses. Health care providers who treat veterans may also submit claims on behalf of the veteran for payment to the Foreign Medical Program. Veterans and health care providers submit claims to the Foreign Medical Program for reimbursement via mail or fax. The Foreign Medical Program does not have a network of providers; rather, veterans can select any health care provider to receive eligible services. The program also does not have a fee schedule or a list of prices setting limitations for how much it will reimburse providers for eligible services.[17]
All Foreign Medical Program claims require the submission of basic information, including the diagnosis, a narrative description of each service, the billed charge, and the date(s) of service.[18] The Foreign Medical Program issues an explanation of benefits to the veteran and to the provider, if benefits will be paid directly to the provider. For claims that VA reimburses, the Department of the Treasury issues a paper check to the veteran or provider.[19] If VHA does not approve reimbursement, and a veteran, provider, legal guardian, or representative for the veteran disagrees with the Foreign Medical Program’s disapproval, they can request reconsideration within 1 year of the original decision.[20] For an overview of the process to register for the Foreign Medical Program and to submit a claim, see figure 1.
To respond to individual questions and concerns about the Foreign Medical Program, including the status of submitted claims, program officials said they are available to communicate directly with veterans and providers via email. Additionally, veterans can use Ask VA, an online tool available on VA’s website to submit questions about the program. The Foreign Medical Program also lists toll-free numbers for contacting the program in their brochure, which are available to veterans in ten countries, including Costa Rica, Germany, and Spain.
Foreign Medical Program officials said they established a goal for the timeliness of claims processing. In fiscal year 2017, officials stated they established the goal of processing 90 percent of claims within 40 days. In fiscal year 2022, officials said they changed the goal to processing 90 percent of claims within 45 days, to accommodate additional time needed for translation services.
Foreign Medical Program officials stated they maintain a dashboard to track their timeliness goal and review the dashboard on a daily basis. According to the officials, the program processed
· 44.6 percent of claims within 45 days in fiscal year 2022,
· 13.8 percent of claims within 45 days in fiscal year 2023, and
· 37.4 percent of claims within 45 days in fiscal year 2024.
Additionally, program officials reported that the average number of days for processing a claim in fiscal year 2024 was 221 days and the median number of days was 182 days. Officials said the average number of days for processing a claim is high as a result of some claims being reopened. Claims may be reopened for a variety of reasons, such as receipt of additional medical documentation, correction of billed charges, or claims paid to an incorrect provider.
Fraud Risk Management
Managers of federal programs, such as the Foreign Medical Program, are responsible for managing fraud risks and implementing practices for combating those risks.[21] Effectively managing fraud risks helps to ensure that federal programs’ services fulfill their intended purpose, funds are spent effectively, and assets are safeguarded.
In July 2015, we issued a Fraud Risk Framework, which provides a comprehensive set of key components and leading practices that agency managers can use when developing efforts to combat fraud in a strategic, risk-based way.[22] As depicted in figure 2, the framework organizes the leading practices within four components: (1) commit, (2) assess, (3) design and implement, and (4) evaluate and adapt.[23]

Within VA, multiple offices and teams are responsible for fraud risk management activities and oversight of the Foreign Medical Program:
· Office of Integrated Veteran Care. This office is responsible for overseeing enterprise risk management and internal control processes specific to the Foreign Medical Program, as well as other VA family member programs within its office.[24] The office provides support to the Foreign Medical Program and is responsible for verifying that program oversight activities are occurring, such as providing reports on the timeliness of claims processing.
· Office of Integrity and Compliance. This office is responsible for VHA’s compliance and risk management functions in accordance with the Office of Management and Budget requirements.[25] VHA officials said this office provides recommendations on how to prevent and mitigate fraud in the program and produces quarterly reports with information regarding potential fraud risks and outlier claims data.
· Office of Business Oversight. This office conducts reviews and assessments of internal controls to help ensure compliance with applicable laws and regulations and provides guidance to program offices, among other responsibilities. For example, VA officials stated the office supports program offices in conducting an annual assessment required for programs ranked “high risk” for fraud in a VA-wide survey.
VHA Data Show Foreign Medical Program Claim Reimbursements More Than Tripled From 2018 through 2024
According to our analysis of VHA data, the total amount reimbursed by the Foreign Medical Program more than tripled from fiscal years 2018 through 2024. Specifically, the total amount reimbursed increased from $35.4 million in fiscal year 2018 to $128.3 million in fiscal year 2024, a 263 percent increase, according to our analysis of VHA data (see figure 3). Additionally, the average dollar value per claim increased from $572 per claim in fiscal year 2018 to $817 per claim in fiscal year 2024.[26]
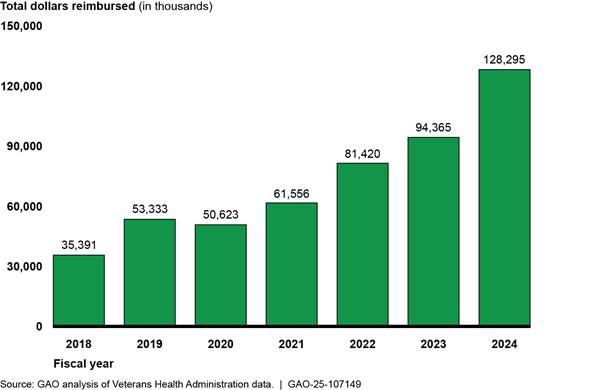
Note: Foreign Medical Program reimbursements can be made to veterans or the health care providers that treated them.
Additionally, VHA data show the total number of claims processed by the Foreign Medical Program more than doubled from fiscal year 2018 to 2024. Specifically, the number of claims processed grew from 79,373 claims in fiscal year 2018 to 204,392 claims in fiscal year 2024, representing a 158 percent increase. The increase in claims was likely due in part to an increase in veteran users. Specifically, the number of unique users of the Foreign Medical Program also more than doubled, growing from 3,259 veterans to 8,024 veterans over the same period (a 146 percent increase). See figure 4.
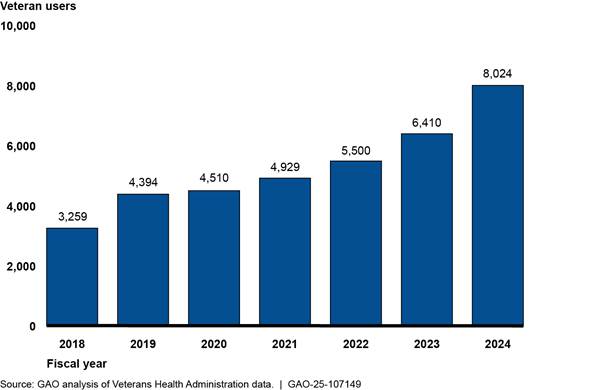
Note: Veteran users represent the veterans who submit claims, as well as providers who submit claims on behalf of the veteran.
Foreign Medical Program officials attributed the growth in the program to a variety of factors. As mentioned above, our analysis of VHA data showed an increase in veteran users across fiscal years 2018 through 2024. Program officials told us one reason for this increase is that they have observed veteran-focused interest groups in certain regions of the world, such as Central America, provide information on the program to veterans living in those regions. According to program officials, the outreach from these groups has resulted in increased veteran participation in the program. Officials also cited veterans’ use of social media as a reason for growth in the program. For example, some veterans are part of a veteran-created Facebook group focused on sharing experiences with the program.
Additionally, Foreign Medical Program officials stated program enrollment has increased due to changes in veteran eligibility. For example, officials said they observed a significant change in program enrollment in 2018 when the program began processing more claims from the Philippines. According to officials, the Manila VA Outpatient Clinic located in Pasay City, Philippines, used to provide a robust offering of health care services to Filipino veterans who supported the U.S. in wars. However, VHA scaled back the services offered in 2017, so more veterans have relied on the Foreign Medical Program.[27] Additionally, the Honoring Our PACT Act of 2022 expanded presumptive conditions associated with exposure to certain toxins.[28] Program officials said this has led to more veterans being eligible for Foreign Medical Program benefits.
Our analysis of VHA data also showed that for fiscal years 2018 through 2024, VHA paid approximately 81 percent of processed claims and rejected 19 percent. Claims may be rejected for a variety of reasons, such as a request for reimbursement of a non-U.S. Food and Drug Administration approved medication or for a service determined not related to a veteran’s service-connected disability. The percentage of claims the Foreign Medical Program rejected varied from fiscal years 2018 through 2022, with increases in 2023 and 2024 compared to the prior years. For example, in fiscal year 2023, VHA rejected 22 percent of claims (32,374 claims out of 149,162 claims), up from 16 percent (22,356 claims out of 137,132 claims) rejected in fiscal year 2022. See figure 5 for the number of claims processed by the Foreign Medical Program for fiscal years 2018 through 2024. Foreign Medical Program officials attributed the decrease in claims processed in 2020 to the COVID-19 pandemic.
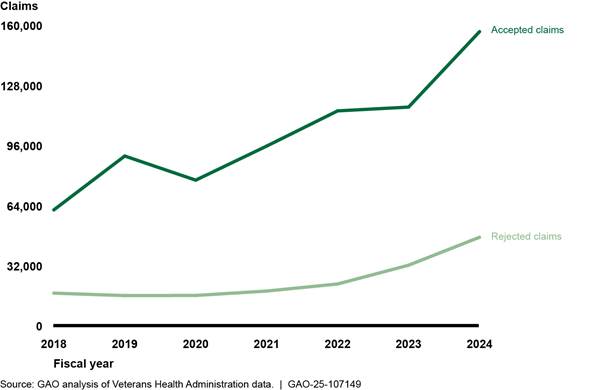
Notes: Accepted claims are claims that were paid by the Foreign Medical Program and rejected claims are claims the program did not approve for reimbursement. Claims may be rejected for a variety of reasons, such as a request for reimbursement of a non-U.S. Food and Drug Administration approved medication or for a service determined not related to a veteran’s service-connected disability.
According to our analysis of VHA data, veterans and providers in about 120 countries submitted claims to the Foreign Medical Program from fiscal year 2018 through 2024. The countries where the highest number of Foreign Medical Program claims were paid from fiscal years 2018 through 2024 was in Panama (220,968 claims), the Dominican Republic (96,561 claims), and Germany (90,006 claims).[29] Additionally, the number of paid claims within some of these countries increased over this period. For example, the number of paid claims within the Dominican Republic increased from 3,188 claims in fiscal year 2018 to 28,104 claims in fiscal year 2024, a 782 percent increase. See figure 6.
Figure 6: Top Countries Where Foreign Medical Program Claims Were Paid, Fiscal Years 2018 through 2024
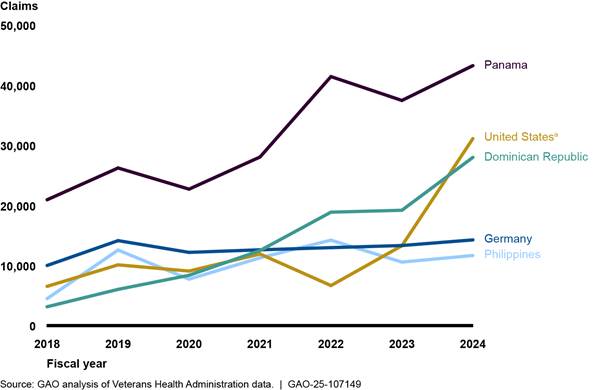
Notes: We included the five countries where the highest total number of claims were paid in from fiscal year 2018 through 2024. As reported by the VA Office of Inspector General in August 2023, a joint VA Office of Inspector General and U.S. Department of State investigation resulted in charges against 12 individuals and 24 companies in Panama for a long-term scheme where the defendants allegedly created a network of medical providers that submitted thousands of false claims to the Foreign Medical Program for services that were double billed, overpriced, unnecessary, or never provided. The VA Office of Inspector General estimated a loss to VA of approximately $67 million. Therefore, amounts reimbursed to providers in Panama are likely inflated. For more information, see https://www.va.gov/health/foreign_medical_program_alerts.asp, accessed on October 3, 2024. See also VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights (Washington, D.C.: August 2023).
aAccording to VHA officials, amounts VHA reimbursed to providers in the U.S. were likely foreign medical providers who have reimbursements sent to U.S. post office boxes due to unreliable mail systems in other countries, as Foreign Medical Program reimbursements are sent through paper checks.
As noted above, Foreign Medical Program reimbursements can be made to veterans or to the health care providers that treated them. VHA data show that the total amount reimbursed to veterans increased from $3.6 million in fiscal year 2018 to $9.1 million in fiscal year 2024 (a 151 percent increase). Over the same period, the total amount reimbursed to health care providers increased from $31.8 million to $119.2 million (a 275 percent increase).
Starting in 2021, the majority of Foreign Medical Program reimbursements to health care providers were concentrated in a small number of countries; in fiscal year 2024 Panama, the U.S., and the Dominican Republic accounted for most of these reimbursements. VHA officials said they are taking steps to determine why reimbursements to providers increased significantly in some countries. Officials acknowledged that it is possible that significant increases in reimbursements could be indicative of potential fraud, such as the fraud identified in Panama. According to VHA officials, amounts VHA reimbursed to providers in the U.S. were likely foreign medical providers who have reimbursements sent to U.S. post office boxes due to unreliable mail systems in other countries, as program reimbursements are sent through paper checks. See figure 7.
Figure 7: Total Amount Reimbursed through the Foreign Medical Program to Health Care Providers, Fiscal Years 2018 through 2024
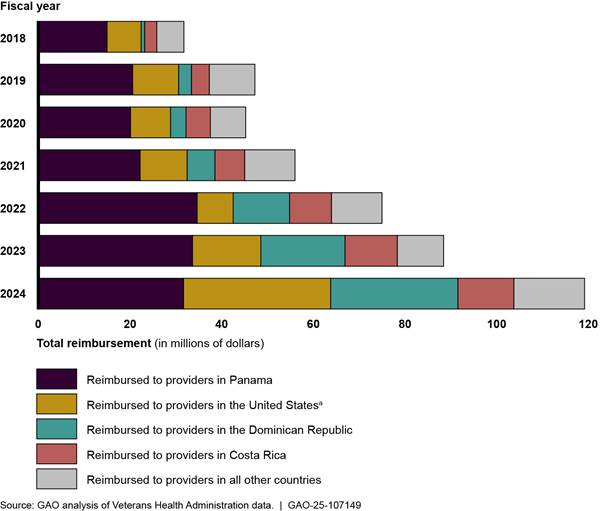
Notes: We included the four countries where the highest total amounts were paid to providers from fiscal year 2018 through 2024. As reported by the VA Office of Inspector General in August 2023, a joint VA Office of Inspector General and U.S. Department of State investigation resulted in charges against 12 individuals and 24 companies in Panama for a long-term scheme where the defendants allegedly created a network of medical providers that submitted thousands of false claims to the Foreign Medical Program for services that were double billed, overpriced, unnecessary, or never provided. The VA Office of Inspector General estimated a loss to VA of approximately $67 million. Therefore, amounts reimbursed to providers in Panama are likely inflated. For more information, see https://www.va.gov/health/foreign_medical_program_alerts.asp, accessed on October 3, 2024. See also VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights (Washington, D.C.: August 2023).
aAccording to VHA officials, amounts VHA reimbursed to providers in the U.S. were likely foreign medical providers who have reimbursements sent to U.S. post office boxes due to unreliable mail systems in other countries, as Foreign Medical Program reimbursements are sent through paper checks.
Outpatient and pharmacy services accounted for almost all of the reimbursements paid by the Foreign Medical Program for fiscal years 2018 through 2024, according to our analysis of VHA data.[30] Outpatient services accounted for approximately three-fourths of paid claims over this period. Some of the most common outpatient services in fiscal year 2024 were physical therapy and therapeutic massage. Pharmacy services represented about one-fifth of paid claims over this period. Inpatient and durable medical equipment claims combined represented a small fraction (about 2.5 percent) of claims paid over this period. See figure 8. See appendix I for additional information on Foreign Medical Program claims from fiscal years 2018 through 2024.
Figure 8: Number of Foreign Medical Program Claims Paid by Service Type, Fiscal Years 2018 through 2024
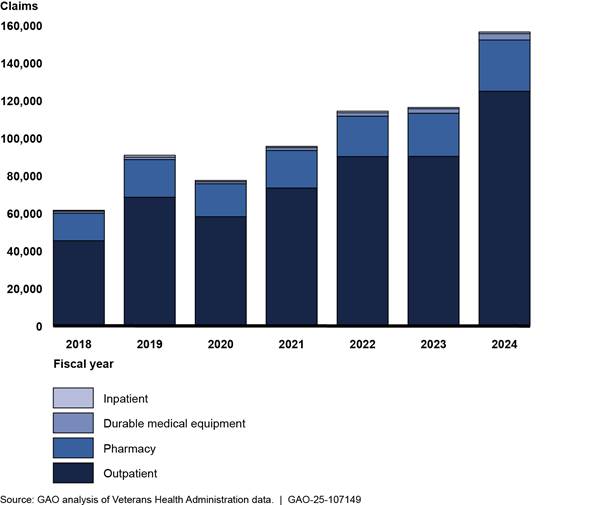
Note: Categories that represented less than one percent of claims across all seven fiscal years are excluded, such as dental services.
|
Reported Examples of Veterans’ Experiences Using the Foreign Medical Program We interviewed veterans in person in Germany and obtained written feedback from 67 veterans representing 17 different countries on their experiences using the Foreign Medical Program. Information we obtained from these interviews and written feedback is not generalizable. Multiple veterans shared examples of challenges they faced related to receiving reimbursement from the Foreign Medical Program for certain types of services. For example, one veteran described treatments for a traumatic brain injury. The veteran said it was challenging to obtain and submit sufficient documentation showing the need for the service, based on a service-connected disability. Ultimately, the veteran said they did receive reimbursement under the program after submitting multiple claims with documentation. Veterans also described challenges finding foreign providers willing to accept Foreign Medical Program coverage as payment. For example, several veterans said their providers were unwilling to bill the Foreign Medical Program directly for services because of the length of time it can take to receive payment. In such instances, a veteran may pay the provider directly and seek reimbursement from the program. Several veterans we heard from said this can be a real financial hardship, especially when costs can be thousands of dollars. Source: GAO analysis of interviews with veterans and written feedback from veterans. | GAO‑25‑107149 |
Some veterans service organization officials and veterans we interviewed noted the importance of the Foreign Medical Program, as well as challenges in using it to access various types of care in foreign countries. For example, some veterans rely on the Foreign Medical Program for coverage of needed services that otherwise may not be covered. One veteran we interviewed in Germany explained that without benefits through the program, it would have been necessary to pay a significant amount of money for a triple bypass surgery that the veteran described as lifesaving. However, officials from four of the five veterans service organizations we interviewed described differences in the standard of care veterans abroad may receive, in comparison to what is provided or available in the U.S. Some of these officials also said that accessing drugs that are U.S. Food and Drug Administration-approved (a requirement for reimbursement eligibility under the program) as well as accessing mental health services is often a challenge for veterans living or traveling in foreign counties. See sidebar for examples we heard from veterans.
The Foreign Medical Program Uses an Outdated System to Process Claims and Provides Reimbursements through Paper Checks
The Foreign Medical Program Has Not Modernized Its Claims Processing System
We found that the Foreign Medical Program uses an outdated claims processing system, called the Claims Processing and Eligibility system, which relies on manual data entry to process claims. Processing claims includes determining whether veterans and providers should be reimbursed. VHA officials described the system, developed in the 1990s, as a legacy system in need of modernization. VA has initiated steps to transition to a new system but has not developed a modernization plan for doing so.
According to Foreign Medical Program officials, the Claims Processing and Eligibility system relies on manual processes. That is, claims examiners manually enter information into the system and make decisions on approving or rejecting claims. When the program receives a claim, staff are to scan the documentation into a system called the Document and Process Enabled Repositories. Claims examiners then use that scanned documentation to enter the information on the veteran, provider, and health care service into the Claims Processing and Eligibility system to process the claim. According to program training documentation for claims examiners, there are 33 steps claims examiners are to conduct to process each claim. If a claims examiner needs guidance or clarification on a claim, such as to determine if a treatment can be associated with a veteran’s service-connected disability, the examiner can consult a nurse review team for clinical review. After a claims examiner goes through each of the steps, such as entering the veteran’s address, assigning a tracking number, and reviewing the substance of the claim information filed, the examiner either approves or rejects the claims.[31]
Foreign Medical Program officials stated that because of manual data entry and system limitations, sometimes data quality issues can arise. According to program officials, to ensure reliable data for a given claim, program staff must examine it on a claim-by-claim basis. If an error is made during the processing of a claim or if a claim has to be reopened after initial processing, staff must generate a new claim number for that claim. As a result, officials stated that it can be difficult to track the progress of individual claims over time, which could make it challenging to respond to veteran inquiries about a claim’s status.
Additionally, Foreign Medical Program officials told us the claims processing system can accommodate three lines of text in the address field in addition to the country name, but sometimes foreign addresses extend beyond this length. Officials said that claims examiners will sometimes enter a third line of text, but that information will not appear on a generated check, which can cause problems when mailing checks to veterans or providers. Officials estimated that the text line limitation in the system results in 10-50 undeliverable checks per week.[32] Undeliverable checks may result in a delayed payment to a veteran or provider, or the need for them to resubmit a claim for reimbursement.
Veterans service organizations and veterans we interviewed described challenges being able to track claims. For example, one veteran explained that reimbursement checks are sometimes sent to the wrong location because the system includes five-digit zip codes that some foreign addresses may not have, creating a barrier for veterans who are seeking reimbursement. Furthermore, some veterans stated that they are not able to track the status of submitted claims because there is no electronic system that veterans can use to look up the status of a claim. According to veterans service organizations and veterans we interviewed, this is particularly problematic when they are often waiting months for reimbursement. One veterans service organization official said that the ability to see the status of a claim is important for veterans as they may bear the financial burden of covering the upfront costs of services.
Foreign Medical Program officials said that in partnership with VA’s Office of Information Technology, they have initiated steps to modernize the claims processing system but have yet to finalize their approach. Specifically, Foreign Medical Program officials told us they initially intended to move claims processing to a system called Claims XM that could be operational sometime in late 2024 or 2025. However, Office of Information and Technology officials said funding was not available for moving to the Claims XM system. Subsequently, in August 2024, Office of Integrated Veteran Care officials told us that claims processing would instead move to a system housed within VA’s Financial Services Center called the Electronic Claims Administration and Management System. The officials said they expect improvements in claims processing once it is within the Financial Services Center. Specifically, officials said they anticipate the new system will allow for a better operating environment to handle claims at a granular level, including auto-adjudication and scanning abilities, rather than the current system that relies on the manual processing of claims.
Office of Integrated Veteran Care officials said they anticipate migrating Foreign Medical Program claims processing to the Financial Services Center system in 2026. The officials said they have established a project team for this effort, but the team has not developed a modernization plan with specific project milestones and time frames for migrating to the new system and retiring the legacy system. Foreign Medical Program officials explained that the project team was delayed in developing milestones for the migration due to unplanned contractual considerations. Officials provided documentation of the decision to move Foreign Medical Program claims processing to VA’s Financial Services Center rather than to procure an external processing system. However, the documentation did not include milestones for the project, a description of the work to be done, or related time frames for moving to the new system.
We have previously reported that, given the age of the hardware and software in legacy systems, the systems’ criticality to agency missions, and the security risks posed by operating aging systems, it is imperative that agencies carefully plan for their successful modernization.[33] Documenting modernization plans in sufficient detail increases the likelihood that modernization initiatives will succeed. Specifically, agencies should have documented plans for legacy systems that include, at a minimum, (1) milestones for completing the modernization, (2) a description of the work necessary to modernize the legacy system, and (3) details regarding the disposition of the legacy system, such as steps agencies should take to retire the system.[34]
Developing and implementing a modernization plan for the claims processing system—to include milestones, a description of the work necessary to modernize the system, and details on the disposition of the legacy system—will help ensure that VA succeeds in updating its legacy claims processing system. In the meantime, data errors such as those associated with incorrect addresses may continue to persist when relying on claims examiners to manually enter in information. A modernization plan that is then fully executed will help the program achieve its timeliness goal, ultimately allowing VHA to improve veterans’ experience, such as through better transparency and tracking of submitted claims and reduced opportunities for errors.
The Foreign Medical Program Has Begun Steps to Transition to Electronic Payments, But When or How the Transition Will Be Completed Is Unclear
After it processes claims, the Foreign Medical Program provides reimbursements for approved claims using paper checks, though a long-standing law requires agencies to use electronic funds transfers when making federal payments. Program officials said they have taken initial steps to transition to electronic payments, but we found VA has not finalized the last implementation steps or prioritized their implementation.
Under the existing process, Foreign Medical Program claims examiners review and approve claims, and then the U.S. Department of the Treasury issues paper checks in U.S. dollars to veterans and providers. However, federal law generally requires that all federal payments made after January 1, 1999, be made by electronic funds transfer unless an agency seeks a waiver from the Department of the Treasury.[35] Foreign Medical Program officials stated that the Department of the Treasury and VA’s Financial Services Center are aware that the Foreign Medical Program uses paper checks.
The use of paper checks to reimburse veterans and providers has resulted in a variety of challenges, according to program officials. For instance, the officials said some mail systems in other countries are not consistently reliable and trustworthy and paper checks can get lost. This may result in delayed receipt of payment or veterans and providers not receiving payment for a claim. The officials stated that because the program reimburses claims using paper checks, some providers in foreign countries elect to use post office boxes in the U.S. to receive reimbursement because that is a more reliable means to receive the checks.[36] Additionally, Foreign Medical Program officials said that some countries are phasing out the use of paper checks as a deposit option. For example, according to these officials, Australia will be phasing out its paper check system; therefore, veterans and providers living in Australia may not be able to receive reimbursement using the program’s existing payment structure in the future.
Some veterans service organizations and veterans we interviewed also identified various challenges with using paper checks. Officials from four of the five veterans service organizations we interviewed described how paper checks can be difficult to cash overseas because foreign banks may not process U.S. checks quickly, banks may charge a fee to cash a foreign check, or the length of time it takes for their bank to clear a check may add to the wait time for reimbursement. For example, officials from one veterans service organization said the fee to cash a check overseas could be as much as 15 percent of the transaction. One veteran said they have to pay 20 dollars each time they cash a U.S. check at a German bank if they do not have a U.S. bank account, and it is an administrative and financial burden to do so. Twenty of the 67 veterans who sent us feedback also described difficulties with receiving paper checks. For example, one veteran stated they paid nearly $3,000 for a 10-hour ambulance ride and overnight hospital stay, but the paper reimbursement check was lost in the mail. The veteran said that as of July 2024 they are still awaiting reimbursement, despite submitting the claim in December 2023 and receiving approval.
Foreign Medical Program officials stated they are working towards developing a new method of payment to offer electronic funds transfers, including reaching out to the Department of the Treasury. Officials said that transitioning to an electronic funds transfer system will have several benefits including modernizing the system, reducing reliance on paper checks, and increasing timeliness of payments through avoiding issues attributed to the mail systems in foreign countries. Foreign Medical Program officials contacted the Department of the Treasury in February 2024 to inquire about working with the department to institute electronic funds transfer capabilities for the Foreign Medical Program.[37]
Office of Integrated Veteran Care officials told us that they have a project team in place to work on a new payment system. Specifically, they said they anticipate their electronic funds transfer project occurring in three phases. The first phase will be converting paper checks to electronic payments to veterans who have domestic bank accounts. According to Foreign Medical Program officials, this work will involve various activities such as building a new interface to collect and store veterans’ direct deposit information from the Veterans Benefits Administration, as well as developing new payment information instructions for the International Treasury Services.[38] Foreign Medical Program officials said they have secured funding for the first phase and expect it to be complete in early 2025; however, they are unsure about funding for phases two and three.
For phases two and three, Office of Integrated Veteran Care officials said they have yet to finalize designated activities and milestones. They anticipate that the second phase will enable electronic payments for veterans with foreign bank accounts and the third will enable electronic payments to health care providers with foreign bank accounts. Their estimated completion date for the final phase is fiscal year 2027, but the officials acknowledged these are rough estimates.
Foreign Medical Program officials said the transition to electronic payments will take a significant effort. The officials explained that not only will payment information need to shift from a physical address to electronic banking information, but they will also need to ensure payments can be shifted from U.S. dollars to local currencies for about 100 countries. These complexities, along with multiple, competing priorities across VA have contributed to uncertainty over the timing of the transition.
Finalizing all of the steps needed to convert reimbursements to electronic payments, in coordination with the Department of the Treasury, and prioritizing their immediate implementation will bring the Foreign Medical Program into compliance with federal law. It will also improve the timeliness of reimbursements, as well as reduce veterans’ administrative and financial burden and help ensure they receive complete, accurate, and secure payments for the care they need to treat their service-connected disabilities.
VHA Took Steps to Begin Adding Staff to Support the Foreign Medical Program but Has Faced Persistent Staffing Challenges
VHA has taken steps to increase the staffing levels of the Foreign Medical Program, but the program continues to face staffing challenges. In October 2021, the Foreign Medical Program employed 20 claims examiners, three leads who verify processed claims, and two supervisors for a total of 25 staff, according to program organizational charts.[39] To improve the timeliness of claims processing, in April 2023, Foreign Medical Program officials stated the program received VHA approval to increase its staffing levels. Specifically, the program’s staffing authorization increased by 13 additional staff, from 25 to 38. However, as of November 2024, the Foreign Medical Program employed 24 of 38 authorized staff, or 63 percent of its authorized staffing level, with 14 positions vacant, according to program officials.
Additionally, in October 2023, VHA introduced two new units to help support the Foreign Medical Program. Housed within the Office of Integrated Veteran Care, the units are (1) the Eligibility, Enrollment, and Verification unit and (2) the Escalation unit. Foreign Medical Program officials stated these units provide support to the program, among other responsibilities, and are intended to improve veterans’ experience with the program.[40] As of February 2024, the Eligibility, Enrollment, and Verification and Escalation units had nine and eight staff, respectively.
Staff in the Eligibility, Enrollment, and Verification unit are to process Foreign Medical Program pre-determination requests for treatments and services and respond to veteran inquiries about eligibility.[41] The Escalation unit is responsible for providing analysis and feedback on foreign provider claim reconciliation requests and conducting status checks on submitted claims. According to Foreign Medical Program officials, the Escalation unit clarifies the program’s scope, such as providing education, to veterans and foreign providers who reach out about the program. Program officials stated that the Escalation unit is responsible for processing veteran inquiries submitted through the Ask VA portal and may also provide claims processing support when needed.[42]
More specifically, our review of agency documentation and interviews with Foreign Medical Program officials show that as of November 2024, VHA had vacancies in a variety of roles for staff within the Foreign Medical Program and among units that support the program. Within the Foreign Medical Program, one lead position and 13 claims examiner positions are vacant. Foreign Medical Program officials told us that the program requested program claims examiner positions as one of its top two staffing priorities. See table 1.
Table 1: Number and Types of Staff Who Support the Veterans Health Administration’s Foreign Medical Program, as of November 2024
|
|
Number of authorized full-time equivalent staff (Vacancies in parentheses) |
|||
|
Program or unit |
Total authorized |
Supervisory program analyst |
Lead staff |
Staff |
|
Foreign Medical Program |
38 |
2 |
5 claims
examiners |
17 claim examiners |
|
Eligibility, Enrollment, and Verificationa |
9 |
1 |
0 |
5 specialists |
|
Escalationa |
8 |
1 |
N/A |
6 analysts |
|
Total |
55 |
4 |
5 |
28 |
Source: GAO analysis of interviews with Foreign Medical Program officials and Veterans Health Administration documentation. | GAO‑25‑107149
Note: Authorized full-time equivalent staff includes filled and vacant positions, and all authorized full-time equivalent staff are fully funded, meaning budgetary resources are sufficient to cover the authorized level.
aForeign Medical Program officials stated these units also serve other VA family member programs, in addition to serving the Foreign Medical Program.
Since 2011, Foreign Medical Program officials said that understaffing has been a challenge, leading to their inability to process claims in a timely manner. In particular, the program’s goal is to process 90 percent of claims within 45 days, but it has not met that goal for the last several fiscal years. As described earlier in this report, program officials said they were able to process 37.4 percent of claims within 45 days in fiscal year 2024, up from 13.8 percent in fiscal year 2023; officials explained that took an “all hands on deck” approach as well as receiving help from others outside the program.[43] Officials noted that the significant increases in claims in recent years have only exacerbated their challenges meeting the timeliness goal.
|
Selected Veteran and Veterans Service Organization Perspectives on Timeliness of Foreign Medical Program Reimbursements We interviewed veterans in person in Germany and obtained written feedback from 67 veterans representing 17 different countries on their experiences using the Foreign Medical Program. Information we obtained from these interviews and written feedback is not generalizable. Veterans and veterans service organizations described their experiences related to timeliness in receiving reimbursement for submitted claims. Three veterans described the reimbursement process as easy or straightforward. In contrast, 41 of the 67 veterans we received written feedback from explained that timeliness of reimbursements is a challenge they face when receiving care through the program. In addition, one veterans service organization we interviewed stated that the lack of timeliness of reimbursements is the challenge they hear most often from veterans regarding the Foreign Medical Program. Several veterans described waiting more than 6 months to over a year to receive payments ranging from hundreds to several thousand dollars for health care services. For example, one veteran we spoke with said it takes between 6 and 12 months to be reimbursed by the Foreign Medical Program and that the veteran was waiting on $3,000 in reimbursements. Veterans indicated waiting for such payments was a financial burden. Of the 41 of 67 veterans who expressed concerns around timeliness of reimbursements, several provided examples. For example, one veteran said the program’s current wait time for reimbursement risks interest accruing if they or other veterans use a credit card to pay for care. Source: GAO analysis of interviews with veterans and veterans service organizations and written feedback from veterans. | GAO‑25‑107149 |
When the Foreign Medical Program posted job announcements in August 2023 to increase its staffing levels to help address its workload, program officials established some milestones for hiring additional staff. However, these milestones were not met. For example, the Foreign Medical Program developed a claims examiner hiring timeline with milestones to hire these positions from August 2023 to April 2024 to fill outstanding vacancies. The timeline included a projected “get-well” date of April 2024, when they expected to consistently and permanently process 90 percent of claims within the program’s goal of 45 days. In addition, program officials told us they received authorization for all claims examiner positions to be remote rather than in person, which they expect could help fill the vacant positions.
However, in February 2024, VHA’s central office instituted a zero-growth policy across the agency.[44] As a result, the program did not meet this get-well date and instead the vacancies remained. Foreign Medical Program officials stated as of November 2024, the program had not received permission to recruit and fill current vacancies, in part due to VHA’s hiring review process and agency-wide prioritized hiring controls in place.[45]
Foreign Medical Program officials said they have communicated to VHA their staffing challenges; however, we found VHA does not have strategies to mitigate those challenges. According to VHA officials, smaller programs like the Foreign Medical Program must compete with other larger programs seen as higher priority, which has contributed to the persistent understaffing in the program. VHA officials we spoke with stated that they post the position announcements for claims examiners but have not otherwise identified any specific strategies to bring additional staff into the Foreign Medical Program.
In light of a zero-growth policy, an evaluation of staffing strategies for the Foreign Medical Program, and implementing them as appropriate, would be consistent with selected key practices we have identified for effective strategic human capital management.[46] These practices state that effective organizations develop strategies to address human capital gaps and achieve programmatic goals and results. In addition, leaders provide resources and incentives that support new ways of working to achieve program goals, drawing from personnel and information technology for resources. Examples for acquiring, developing, and retaining staff could include opportunities for a combination of formal and on-the-job training, rotational assignments, recruitment bonuses and retention allowances, and mentoring relationships with other employees.
Evaluating and implementing as appropriate staffing strategies could help the Foreign Medical Program better address its staffing challenges. The Foreign Medical Program has taken steps such as allowing claims examiners to be remote; however, evaluating potential strategies, such as rotational assignments, could assist the program with filling the open positions. To the extent that such strategies are effective, the Foreign Medical Program would be better positioned to meet its processing timeliness goal and reduce the amount of time veterans wait for reimbursements for care.
Several VA Offices Conduct Fraud Risk Management Activities, but VA Has Not Followed Selected Leading Practices
Several offices within VA support fraud risk management activities for the Foreign Medical Program. However, we found that VA has not followed selected leading practices outlined in our Fraud Risk Framework. Specifically, VA has not designated an entity to lead fraud risk management and does not comprehensively assess fraud risks using elements identified in our framework.
Several Offices Conduct Fraud Risk Management Activities, but No Entity Leads These Activities in the Foreign Medical Program
Within VA, multiple offices and teams support fraud risk management activities in the Foreign Medical Program. For example, the Office of Integrated Veteran Care oversees the program’s operations, including to ensure the processing of registration, authorization of benefits, and reimbursement of claims consistent with applicable laws, regulations, and Foreign Medical Program requirements. In addition, VHA officials stated the Office of Integrity and Compliance’s fraud, waste, and abuse team provides the program with recommendations on how to prevent fraud and works with the program if it discovers a potential case of fraud. Lastly, VA officials said its Office of Business Oversight supports program offices in conducting an annual assessment for VA programs ranked “high risk” for fraud.
Our review found that VA has not followed selected leading practices in fraud risk management in the Foreign Medical Program. These practices call for program managers to designate an antifraud entity with defined responsibilities and necessary authority for leading and overseeing fraud risk management activities (see sidebar).[47] For example, the dedicated entity could be an individual or a team that works with staff to implement fraud controls, manages the fraud risk assessment process, and leads or assists with fraud awareness activities.
|
Leading Practices for Creating a Structure to Lead Fraud Risk Management Activities Leading practices in GAO’s Fraud Risk Framework include creating a structure with a dedicated entity to lead fraud risk management activities. Specifically, the leading practices call for designating a dedicated entity to design and oversee fraud risk management activities that · understands the program and its operations, as well as the fraud risks and controls throughout the program; · has defined responsibilities and the necessary authority across the program; · has a direct reporting line to senior-level managers within the agency; and · is located within the agency and not the Office of Inspector General, so the latter can retain independence to serve its oversight role. In carrying out this role, the antifraud entity, among other things, · serves as the repository of knowledge on fraud risks and controls, · manages the fraud risk assessment process, · leads or assists with trainings and other fraud awareness activities, and · coordinates antifraud initiatives across the program. Source: GAO | GAO‑25‑107149 |
While various offices have involvement in fraud risk management for the Foreign Medical Program, VA has not defined and documented roles and responsibilities for a designated entity with authority to lead and oversee fraud risk management activities for the program. In February 2024, the Office of Integrated Veteran Care drafted an internal controls playbook for programs within the office, including the Foreign Medical Program.[48] This draft playbook provides programs within the Office of Integrated Veteran Care with a guide for establishing internal controls, such as monitoring. However, this draft playbook does not outline roles and responsibilities for an entity to lead fraud risk management in specific programs, including the Foreign Medical Program.
In addition, officials from the Office of Integrated Veteran Care developed an enterprise risk management playbook in March 2024 to help identify potential fraud in their programs, including the Foreign Medical Program. This playbook outlines how VHA’s enterprise risk management will collaborate on fraud, waste, and abuse activities within VHA and highlights fraud risk management principles integrated with internal controls.[49] However, the playbook does not specify roles and responsibilities for an entity to lead fraud risk management specific to the Foreign Medical Program. GAO’s Fraud Risk Framework which provides leading practices for developing efforts to combat fraud, acknowledges that some agencies may incorporate fraud risk management activities into other initiatives, like enterprise risk management. That, however, does not eliminate the need for separate and independent fraud risk-management efforts, in a complementary manner. Specifically, GAO’s Fraud Risk Framework identifies leading practices to manage fraud risks at the program level to support program integrity and ensure the program fulfills its intended purpose.
We found that the Foreign Medical Program does not have a dedicated entity to lead fraud risk management activities. Specifically, VA has not defined responsibilities for leading and coordinating fraud risk management activities in the Foreign Medical Program. Officials from the Office of Integrated Veteran Care stated that subject-matter experts within the fraud, waste, and abuse team and risk management team moved to the Office of Integrity and Compliance when VHA created the Office of Integrated Veteran Care.[50] They added that the Office of Integrated Veteran Care hired a fraud, waste, and abuse lead in 2024 to assess fraud issues across the Office of Integrated Veteran Care. However, officials explained there are some decisions that need to be made regarding who is fully responsible for fraud-related processes for the program. In addition, VA did not have documentation that assigns roles or responsibilities for leading fraud risk management activities in the Foreign Medical Program. Until those decisions are made, an entity like the Office of the Integrity and Compliance’s fraud, waste, and abuse team cannot implement a fraud oversight process for the program.
By designating an entity with specific roles, responsibilities, and authorities to lead and oversee fraud risk management, VA could position itself to more strategically manage fraud risk in the Foreign Medical Program. Establishing such an entity would support an organizational structure conducive to fraud risk management in that the entity would be responsible for implementing strategies for preventing, detecting, and responding to fraud.
VA Does Not Comprehensively Assess Fraud Risks in Line with Selected Leading Practices
VA has taken some steps to detect potential fraud in the Foreign Medical Program through developing program policies and addressing risks identified by other VA offices. For example, Foreign Medical Program officials stated lead claims examiners are to audit all claims over $20,000, and the Office of Integrity and Compliance reviews claims from veterans or providers on the program’s Watch List, according to our review of
program documentation.[51] In addition, in 2024, VA officials identified two fraud risks in the program—veterans or providers overcharging for services or submitting claims for services that were not medically necessary or not rendered—by reviewing relevant press releases or external audit reports, according to officials. However, we found that VA and the Foreign Medical Program did not complete a fraud risk assessment consistent with leading practices.
|
Leading Practices for Regular Fraud Risk Assessments That Are Tailored to the Program Leading practices in GAO’s Fraud Risk Framework include planning regular fraud risk assessments that are tailored to the program. Specifically, the leading practices call for · tailoring fraud risk assessments to its programs; · planning to conduct fraud risk assessments at regular intervals; · identifying tools, methods, and sources for gathering information on fraud risks; and · involving relevant stakeholders in the assessment process. Source: GAO | GAO‑25‑107149 |
Leading practices in fraud risk management call for agencies to plan regular fraud risk assessments that are then used to develop a fraud risk profile (see sidebar).[52]
The Fraud Risk Framework includes five key elements for assessing fraud risks in federal programs (see figure 9). These key elements include (1) identifying inherent fraud risks affecting the program, (2) assessing the likelihood and impact of inherent fraud risks, (3) determining a fraud risk tolerance, (4) examining the suitability of existing fraud controls and prioritizing residual fraud risks, and (5) documenting the program’s fraud risk profile.
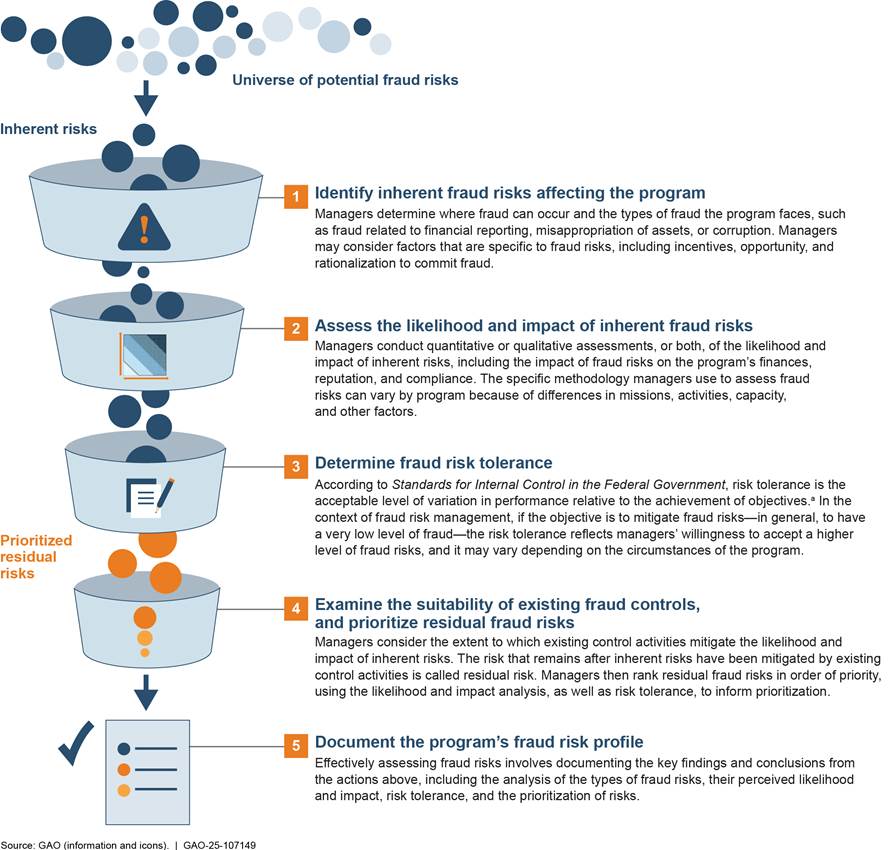
aGAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: Sept. 10, 2014), 6.08.
A comprehensive fraud risk assessment in alignment with leading practices, as described in our Fraud Risk Framework, would involve assessing all inherent fraud risks, rather than focusing solely on the two fraud risks VA identified to date. Leading practices call for involving relevant stakeholders in developing a list of fraud risks for analysis, whereas officials from VA’s Office of Business Oversight stated they identified these two fraud risks without coordination with the Foreign Medical Program. Further, leading practices call for assessing the likelihood and impact of inherent fraud risks, determining a fraud risk tolerance, examining the suitability of existing fraud controls, and prioritizing residual fraud risks, and documenting the program’s fraud risk profile. VA has not taken any of these steps to date.
The Office of Integrity and Compliance recommended that the Office of Integrated Veteran Care implement a fraud risk assessment within its internal control processes. In November 2024, officials estimated they would complete a fraud risk assessment by September 2026. However, as of November 2024, the Office of Integrated Veteran Care had not identified steps it would take to begin such an assessment, such as preparing documentation.
As the Office of Integrated Veteran Care looks to conduct a fraud risk assessment, the office could partner with external stakeholders, such as the Department of the Treasury. Leading practices in GAO’s Fraud Risk Framework state that program managers should involve relevant internal and external stakeholders in the assessment process to reflect a complete understanding of fraud risks and vulnerabilities. For example, the Department of the Treasury’s Office of Payment Integrity uses enhanced fraud detection processes, including machine learning artificial intelligence, to help prevent fraud across programs within the federal government.[53]
Comprehensively assessing fraud risks consistent with leading practices will help VA determine whether or to what extent it should respond to the large increases in claims activity the program has experienced in recent years. Large, unexplained increases in claims activity, such as what the Foreign Medical Program experienced from 2018 to 2024, could signal that a program is susceptible to fraud. As discussed earlier, a joint VA Office of Inspector General and U.S. Department of State investigation charged 12 individuals and 24 companies in Panama where the defendants allegedly created a network of medical providers that submitted thousands of false claims to the Foreign Medical Program for services that were double billed, overpriced, unnecessary, or never provided.[54] As a result of the investigation’s findings, the VA Under Secretary for Health suspended a group of 36 medical providers in August 2024 at the recommendation of the VA Office of the Inspector General. In a media statement, VA stated the suspensions affected approximately 1,030 veterans living in Panama who had been notified and advised to seek care from other Panamanian medical providers not included on the suspension list.
Without regularly and comprehensively assessing Foreign Medical Program fraud risks, VA may not be able to effectively prevent, detect, or respond to fraud in the program. As described in our Fraud Risk Framework, regular fraud risk assessments that address all five key elements would better enable the Foreign Medical Program to document its fraud risk profile and inform the design and implementation of effective fraud controls. Further, implementing selected leading practices for fraud risk management will help VA ensure its Foreign Medical Program is meeting its intended purpose to provide reimbursement for care to veterans living and traveling abroad.
Conclusions
The Foreign Medical Program plays a key role in reimbursing the thousands of veterans living or traveling abroad for health care services related to their service-connected disabilities. With significant growth in the program in recent years, ensuring the program provides valid and timely payments to qualifying veterans or their providers is important.
Along those lines, the Foreign Medical Program intends to transition to a new claims processing system, replacing its legacy system dating back to the 1990s. By developing and implementing a modernization plan for the claim processing system that includes milestones, a description of the work necessary to modernize the legacy system, and details regarding the disposition of the legacy system, the program could better ensure a successful transition to a new claims processing system. The new system could also help the program improve veterans’ experiences.
The Foreign Medical Program has also outlined initial steps to transition its claims reimbursement from paper checks to electronic funds transfers. However, it is unclear when or how the transition will be completed because VHA has not finalized all of the steps needed to convert reimbursements to electronic payments or prioritized their immediate implementation. Prioritizing and taking immediate steps to implement the transition to electronic funds transfers, in coordination with the Department of the Treasury, will provide for a more timely and secure payment process to veterans and providers seeking reimbursement.
The Foreign Medical Program received approval to increase its authorized staffing levels to help meet its timeliness goal for claims processing. But it continues to face persistent staffing challenges in light of its zero-growth policy with multiple positions remaining vacant, hindering the program’s ability to process claims in a timely manner. By evaluating and implementing strategies as appropriate to mitigate staffing challenges, VHA would be better positioned to help ensure that the Foreign Medical Program can more efficiently reimburse veterans for their service-connected health care needs.
Although several VA offices conduct fraud risk management
activities for the Foreign Medical Program, we found VA’s efforts are not
consistent with selected leading practices for fraud risk management. Given
that fraud has been detected in the program and the volume of claims has grown
in recent years, VA would benefit from taking steps to assess fraud risks and
implement selected leading practices for effective fraud risk management.
Specifically, designating a dedicated antifraud entity would better position VA
to strategically manage fraud risks in the Foreign Medical Program. Further,
conducting regular fraud risks assessments—covering the five key elements of
such assessments and coordinating with stakeholders such as the Department of
the Treasury, as appropriate—would help ensure that the Foreign Medical Program
effectively prevents, detects, and responds to fraud.
Recommendations for Executive Action
We are making the following nine recommendations to VHA:
The Under Secretary for Health should, in coordination with the Foreign Medical Program, develop and implement a modernization plan for the program’s legacy claims processing system, including milestones, a description of the work necessary, and details on the disposition of the legacy system. (Recommendation 1)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, finalize the necessary steps to transition to electronic funds transfers and immediately prioritize their implementation in coordination with the Department of the Treasury, as appropriate. (Recommendation 2)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, evaluate and implement as appropriate strategies to help mitigate staffing challenges that affect the Foreign Medical Program. (Recommendation 3)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, designate a dedicated entity for managing the process of assessing fraud risks to the program, consistent with leading practices. This entity should have, among other things, clearly defined and documented responsibilities, and authority for managing fraud risk assessment for the program. (Recommendation 4)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, regularly identify inherent fraud risks in the program and coordinate with external stakeholders, such as the Department of the Treasury, as appropriate. (Recommendation 5)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, assess the likelihood and impact of inherent fraud risks in the program. (Recommendation 6)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, determine a fraud risk tolerance for the program. (Recommendation 7)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, examine the suitability of existing fraud controls and prioritize residual fraud risks in the program. (Recommendation 8)
The Under Secretary for Health should, in coordination with the Foreign Medical Program, document a fraud risk profile for the program. (Recommendation 9)
Agency Comments and Our Evaluation
We provided a draft of this report to VA for review and comment. In its written comments, reproduced in appendix II, VA concurred with our recommendations and identified actions VHA plans to take to address them.
Regarding our first recommendation, VA stated the Foreign Medical Program’s claims processing system is part of a larger modernization portfolio plan and the estimated completion date for transition to a new system is May 2027. VA stated it would provide a detailed transition plan with milestones, a description of the necessary work, and details of the legacy system sunsetting plan by May 2026.
With respect to our second recommendation, VA stated that it initiated the Foreign Medical Program electronic funds transfer project in September 2023, and is on track to implement the first phase of the transition in April 2025. VA stated that it anticipates a completion date of March 2026 and December 2026 for the final two phases, respectively.
For our third recommendation, VA stated that the Foreign Medical Program has implemented a range of strategies to address staffing challenges, such as authorizing performance awards and launching an employee mentorship program. VA stated that the program has allocated a budget for voluntary overtime and that claims examiners will be staffed at authorized levels, in alignment with VHA’s strategic hiring guidance.
However, VA did not provide information on how it plans to increase staffing to reach authorized levels. As we reported, understaffing has been a challenge for the Foreign Medical Program since 2011 and it has struggled to fill advertised positions. By further identifying and implementing staffing strategies, VHA can better ensure it is able to reach authorized levels, as well as other possible means of efficiently reimbursing veterans through the program.
Regarding our fourth recommendation, VA stated that the Office of Integrated Veteran Care, in collaboration with the Office of Integrity and Compliance and financial stakeholders, will continue advancing the development of a comprehensive internal control program. According to VA, the initiative will include the identification, assessment, and management of fraud risk, and it will be aligned with leading practices and tailored to meet the needs of the Foreign Medical Program.
With respect to our fifth through ninth recommendations, relating to each of the five key elements for conducting regular fraud risk assessments, VA stated that the Office of Integrated Veteran Care, in collaboration with the Office of Integrity and Compliance and financial stakeholders, will continue advancing the development of a comprehensive internal control program. According to VA, the initiative will include steps such as the identification of inherent fraud risk in the program, coordination with external stakeholders, developing a fraud risk assessment, and examination of the suitability of existing fraud controls, among other steps in alignment with the key elements for regular fraud assessments. VA anticipates completing these efforts by July 2026.
VA also provided technical comments, which we incorporated as appropriate.
We are sending copies of this report to the appropriate congressional committees, the Secretary of Veterans Affairs, and other interested parties. In addition, the report is available at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions about this report, please contact me at (202) 512-7114 or hundrupa@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix III.

Alyssa M. Hundrup
Director, Health Care
Appendix I: Supplemental Information on Veterans Health Administration Foreign Medical Program Claims
This appendix presents supplemental information on Foreign Medical Program claims from fiscal years 2018 through 2024. Data presented are based on our analysis of summary data provided by the Veterans Health Administration (VHA) on Foreign Medical Program claims processed during these years (see tables 2 through 4).
|
|
2018 |
2019 |
2020 |
2021 |
2022 |
2023 |
2024 |
|
Accepted claims |
61,905 |
90,676 |
77,793 |
95,973 |
114,776 |
116,788 |
157,080 |
|
Rejected claims |
17,468 |
16,164 |
16,242 |
18,581 |
22,356 |
32,374 |
47,312 |
|
Total |
79,373 |
106,840 |
94,035 |
114,554 |
137,132 |
149,162 |
204,392 |
Source: GAO analysis of summary data from the Veterans Health Administration. | GAO‑25‑107149
Notes: Accepted claims are claims that were paid by the Foreign Medical Program and rejected claims are claims the program did not approve for reimbursement. Claims may be rejected for a variety of reasons, such as a request for reimbursement of a non-prescription medication or for a service determined not related to a veteran’s service-connected disability.
Table 3: Percentage of Foreign Medical Program Claims Paid by Service Type, Fiscal Years 2018 through 2024
|
|
2018 |
2019 |
2020 |
2021 |
2022 |
2023 |
2024 |
|
Durable medical equipment |
1.6 |
1.5 |
1.4 |
1.6 |
1.7 |
2.1 |
2.1 |
|
Inpatient |
0.9 |
1.1 |
0.9 |
0.8 |
0.7 |
0.6 |
0.6 |
|
Outpatient |
73.6 |
75.8 |
75.0 |
76.7 |
78.8 |
77.5 |
79.7 |
|
Pharmacy |
23.7 |
22.2 |
22.6 |
20.9 |
18.8 |
19.7 |
17.5 |
Source: GAO analysis of summary data from the Veterans Health Administration. | GAO‑25‑107149
Notes: Categories that represented less than 1 percent of claims across all seven fiscal years are excluded, such as dental services. Due to rounding, percentages may not add to 100.
Table 4: Top 10 Countries Where Foreign Medical Program Claims Were Paid by Total Amount Reimbursed, Fiscal Years 2018 through 2024
In thousands of dollars
|
|
2018 |
2019 |
2020 |
2021 |
2022 |
2023 |
2024 |
Total |
|
Panama |
15,101 |
20,796 |
20,368 |
22,446 |
34,879 |
33,800 |
31,792 |
179,182 |
|
United Statesa |
7,851 |
11,053 |
9,774 |
11,115 |
9,114 |
16,768 |
35,529 |
101,204 |
|
Dominican Republic |
767 |
2,995 |
3,653 |
6,262 |
12,423 |
18,382 |
27,895 |
72,377 |
|
Costa Rica |
2,713 |
4,103 |
5,536 |
6,528 |
9,243 |
11,438 |
12,401 |
51,961 |
|
Philippines |
1,306 |
4,408 |
2,793 |
5,889 |
6,043 |
4,599 |
7,673 |
32,711 |
|
Germany |
3,938 |
4,554 |
3,449 |
3,960 |
4,162 |
3,545 |
4,194 |
27,802 |
|
Thailand |
1,216 |
2,154 |
1,820 |
2,216 |
2,503 |
1,982 |
2,613 |
14,504 |
|
Colombia |
125 |
51 |
594 |
289 |
207 |
1,067 |
2,792 |
5,126 |
|
Mexico |
474 |
688 |
405 |
689 |
398 |
417 |
162 |
3,233 |
|
Japan |
295 |
374 |
254 |
551 |
398 |
414 |
408 |
2,693 |
Source: GAO analysis of summary data from the Veterans Health Administration. | GAO‑25‑107149
Notes: We included the 10 countries where the highest total amounts were reimbursed from fiscal year 2018 through 2024. As reported by the Department of Veterans Affairs (VA) Office of Inspector General in August 2023, a joint VA Office of Inspector General and U.S. Department of State investigation resulted in charges against 12 individuals and 24 companies in Panama for a long-term scheme where the defendants allegedly created a network of medical providers that submitted thousands of false claims to the Foreign Medical Program for services that were double billed, overpriced, unnecessary, or never provided. The VA Office of Inspector General estimated a loss to VA of approximately $67 million. Therefore, amounts reimbursed to providers in Panama are likely inflated. For more information, see https://www.va.gov/health/foreign_medical_program_alerts.asp, accessed on October 3, 2024. See also VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights (Washington, D.C.: August 2023).
aAccording to VHA officials, amounts VHA reimbursed to providers in the U.S. were likely foreign medical providers who have reimbursements sent to U.S. post office boxes due to unreliable mail systems in other countries, as Foreign Medical Program reimbursements are sent through paper checks.
GAO Contact
Alyssa M. Hundrup, (202) 512-7114 or hundrupa@gao.gov.
Staff Acknowledgments
In addition to the contact named above, Rebecca Rust Williamson (Assistant Director), Alison Granger (Analyst-in-Charge), Megan Knox, and Haley Samuel-Jakubos made key contributions to this report. Also contributing were Dean Campbell, Madeline Day, Jacquelyn Hamilton, David Jones, Diona Martyn, Jennifer Stavros-Turner, Jeanne Sung, Jeff Tamburello, and Cathleen Whitmore.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, X, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]The Foreign Medical Program is responsible for providing health care benefits for veterans living or traveling in a foreign country with VA-rated service-connected disabilities and conditions associated with and held to be aggravating a service-connected disability (i.e., injuries or diseases incurred or aggravated in line of duty in the active military service). For the purpose of this report, we define a “foreign country” as any place other than each of the several states, territories, and possessions of the United States, the District of Columbia, and the Commonwealth of Puerto Rico.
[2]Specifically, we found that the number of disability claims increased from 16,082 claims to 18,287 claims, a 14 percent increase, from fiscal years 2014 to 2019. See GAO, VA Disability Benefits: VA Should Continue to Improve Access to Quality Disability Medical Exams for Veterans Living Abroad, GAO‑20‑620 (Washington, D.C.: Sept. 21, 2020). We made five recommendations to VA to improve foreign veterans’ access to quality disability exams. VA agreed with those recommendations and has since implemented them.
[3]See GAO, Immigration Enforcement: Actions Needed to Better Handle, Identify, and Track Cases Involving Veterans, GAO‑19‑416 (Washington, D.C.: June 6, 2019). From fiscal years 2013 through 2018, VA reported receiving 373,916 claim reimbursements from veterans and providers and awarding over $169 million in claim reimbursements. In fiscal year 2022, VHA changed its timeliness goal of processing 90 percent of Foreign Medical Program claims within 40 days to processing 90 percent of claims within 45 days, according to officials.
[4]For more information, see https://fixourfmp.org/news/about-us/, accessed October 24, 2024.
[5]For more information, see https://www.va.gov/health/foreign_medical_program_alerts.asp, accessed on October 3, 2024. See also VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights (Washington, D.C.: August 2023).
[6]Pub. L. No. 117-328, § 172, 136 Stat. 4459, 5434-35 (2022).
[7]General Services Administration, Unified Shared Services Management, Modernization and Migration Management (M3) Playbook (Aug. 3, 2016); M3 Playbook Guidance (Aug. 3, 2016); American Technology Council, Report to the President on Federal IT Modernization (Dec. 13, 2017); Office of Management and Budget, Strengthening the Cybersecurity of Federal Agencies by Enhancing the High Value Asset Program, M-19-03 (Washington, D.C.: Dec. 10, 2018); American Council for Technology-Industry Advisory Council, Legacy System Modernization: Addressing Challenges on the Path to Success (Fairfax, Va.: Oct. 7, 2016); and Dr. Gregory S. Dawson, Arizona State University, IBM Center for The Business of Government, A Roadmap for IT Modernization in Government (Washington, D.C.: 2018). GAO, Information Technology: Agencies Need to Develop Modernization Plans for Critical Legacy Systems, GAO‑19‑471 (Washington, D.C.: June 11, 2019).
[8]31 U.S.C. § 3332.
[9]GAO, A Model of Strategic Human Capital Management, GAO‑02‑373SP, (Washington, D.C.: Mar. 15, 2002). We selected key practices related to acquiring, developing, and retaining talent. More specifically, we selected the following two practices: (1) targeted investments in people and (2) human capital approaches tailored to meet organizational needs.
[10]Fraud involves obtaining something of value through willful misrepresentation. Fraud risk (which is a function of likelihood and impact) exists when people have an opportunity to engage in fraudulent activity, have an incentive or are under pressure to commit fraud, or are able to rationalize committing fraud. Although the occurrence of fraud indicates there is a fraud risk, a fraud risk can exist even if fraud has not yet occurred or been identified. The Payment Integrity Information Act of 2019 authorizes the Office of Management and Budget, in consultation with GAO, to maintain guidelines for agencies to conduct a fraud risk evaluation using a risk-based approach to design and implement financial and administrative controls to mitigate identified fraud risks. See 31 U.S.C. § 3357(b).
[11]GAO, A Framework for Managing Fraud Risks in Federal Programs, GAO‑15‑593SP (Washington, D.C.: July 28, 2015). The Commit component states managers commit to combating fraud by creating an organizational culture and structure conducive to fraud risk management. The Assess component states managers plan regular fraud risk assessments and assess risk to determine a fraud risk profile.
[12]For a veteran to receive reimbursement for health care services through the Foreign Medical Program, the veteran must first submit a disability claim with VA. To help determine a veteran’s entitlement to benefits, Veterans Benefits Administration staff may request that the veteran undergo a disability medical exam to obtain additional medical evidence. Disability ratings are awarded in 10-percent increments up to 100 percent to determine severity of a service-connected disability. Disability percentages have no bearing on determining eligibility for Foreign Medical Program services. In addition, a veteran is not entitled to medical care for any period during which the veteran is a fugitive felon or during any period of incarceration.
[13]The Foreign Medical Program does not cover the cost of travel for health care services. Other examples of general health benefit exclusions include any service, procedure, treatment, drug, or device that is experimental or investigational; assisted living; dental care (unless service-connected); durable medical equipment with deluxe or luxury features; nursing homes; and physical therapy not under the supervision of a licensed physician. For care provided in Canada, claims must be submitted to Veterans Affairs of Canada, Foreign Countries Operations.
[14]However, the Foreign Medical Program does not send medicines by mail or cover mail-order medicines from the U.S.
[15]See https://www.va.gov/health‑care/foreign‑medical‑program/, U.S. Department of Veterans Affairs, accessed on September 10, 2024. According to VA officials, in October 2024, the Foreign Medical Program instituted a modernized online registration site for the program that simplified and improved the registration process for veterans. For more information, see https://www.va.gov/health-care/foreign-medical-program/register-form-10-7959f-1/introduction, U.S. Department of Veterans Affairs, accessed on January 29, 2025.
[16]See VA Health Care, theSITREP, “VA’s Foreign Medical Program with Dirk Rasnic,” accessed August 15, 2024, https://www.youtube.com/watch?v=OhsMMBjnesg; See VA Health Care, theSITREP, “VA’s Foreign Medical Program with Leticia Diaz,” accessed August 15, 2024, https://www.youtube.com/watch?v=wH2qjNOb7tI.
[17]Foreign Medical Program officials stated the program does not have the authority to establish a fee schedule or list of prices setting limitations for how much it will reimburse for eligible services. In July 2024, a bill was introduced in the House of Representatives that would require the Secretary of VA to assess the feasibility and implications of entering into a contract to build a network of community providers to provide hospital care or medical services under the Foreign Medical Program. H.R. 9177, 118th Cong. § 2(c) (2024).
[18]Claims for reimbursement for expenses of medical care or services must be filed no later than 2 years after (1) the date the care or service was rendered or (2) the date of discharge for inpatient hospitalizations. Foreign Medical Program claims should also include the patient’s full name and address; Social Security Number and VA file number; the provider’s name and address; proof of the veteran’s payment; and a copy of treatment notes to support reimbursement for medical treatment of the service-connected disability, among other information. Veterans are to provide this information using a Foreign Medical Program claim cover sheet.
[19]Reimbursements are to be based on the currency exchange rate at the date of service.
[20]The request for reconsideration must also include why the provider, veteran, legal guardian, or veteran’s representative believes the decision was made in error and include any new and relevant information not previously considered. After reviewing the reconsideration request, VHA issues a written determination. Subsequent appeals can be made through the Director of Program Administration at Purchased Care at the Health Administration Center or the Board of Veterans’ Appeals.
[21]Fraud risk (which is a function of likelihood and impact) exists when people have an opportunity to engage in fraudulent activity, have an incentive or are under pressure to commit fraud, or are able to rationalize committing fraud. Although the occurrence of fraud indicates there is a fraud risk, a fraud risk can exist even if fraud has not yet occurred or been identified. The Payment Integrity Information Act of 2019 authorizes the Office of Management and Budget, in consultation with GAO, to maintain guidelines for agencies to conduct a fraud risk evaluation using a risk-based approach to design and implement financial and administrative controls to mitigate identified fraud risks. See Pub. L. No. 116-117, §§ 2(a), 3(a)(4) 134 Stat. 113, 131–132, 133 (2020), codified at 31 U.S.C. § 3357.
[23]In its 2016 Circular No. A-123 guidelines, the Office of Management and Budget directed agencies to adhere to the Fraud Risk Framework’s leading practices. See Office of Management and Budget, Management’s Responsibility for Enterprise Risk Management and Internal Control, Office of Management and Budget Circular No. A-123 (Washington, D.C. July 15, 2016). In October 2022, the Office of Management and Budget issued a Controller Alert reminding agencies that they should adhere to the leading practices in the Fraud Risk Framework as part of their efforts to effectively design, implement, and operate an internal control system that addresses fraud risks. See Office of Management and Budget, Establishing Financial and Administrative Controls to Identify and Assess Fraud Risk, CA-23-03 (Washington, D.C.: Oct. 17, 2022).
[24]According to the Office of Management and Budget, enterprise risk management is defined as an effective agency-wide approach to addressing the full spectrum of the organization’s significant internal and external risks by understanding the combined impact of risks as an interrelated portfolio, rather than addressing risks only within silos. Conversely, internal control is a process used by management to help an entity achieve its objectives.
The Office of Integrated Veteran Care is responsible for operating enrollment and customer service functions through other veteran family member programs, including the Camp Lejeune Family Member Program, Children of Women Vietnam Veterans, and the Spina Bifida Health Care Benefits Program. According to VA officials, the Office of Integrity and Compliance identified a need for the Office of Integrated Veteran Care to routinely assess compliance with applicable laws and regulations and to evaluate internal controls and risk management activities. The Office of Integrated Veteran Care established a new office in 2023, the Office of internal Review and Oversight, to respond to this need.
[25]See Office of Management and Budget Circular No. A-123. The Office of Integrity and Compliance is responsible for various other compliance activities, such as VHA’s anti-fraud, waste, and abuse, statement of assurance, and internal controls assessment responsibilities.
[26]To calculate the average dollar value per claim, GAO used the total amount reimbursed on claims and divided that number by the total number of claims paid. We calculated this value for both fiscal years 2018 and 2024.
[27]The Manila VA Outpatient Clinic in the Philippines is the only VA health care facility located in a foreign country and is located on U.S. Embassy property. VHA Directive 1521 and 38 U.S.C. § 1724 provides the authority that veterans residing in or visiting the Philippines may receive care and services for a service-connected disability or certain rehabilitation at the Manila VA Outpatient Clinic. A veteran with a service-connected disability may be treated for non-service-connected disabilities within the limits of the Manila VA Outpatient Clinic.
[28]Title 1 of the Honoring Our PACT Act of 2022 (PACT Act) expanded VA health care and benefits for veterans exposed to specific categories of toxins, such as burn pits, Agent Orange, and other toxic substances. Starting in March 2024, VA expanded eligibility to enroll in VA health care for veterans if they meet basic service and discharge requirements and certain descriptions during their time in service or exposure to specific toxins or hazards. Title IV of the PACT Act expanded presumptive conditions associated with exposure to burn pits and other toxins. This resulted in a potential increase in eligibility for certain health care and benefits. See Pub. L. No. 117-168, 136 Stat. 1759 (2022).
[29]As reported by the VA Office of Inspector General in August 2023, a joint VA Office of Inspector General and U.S. Department of State investigation resulted in charges against 12 individuals and 24 companies in Panama for a long-term scheme where the defendants allegedly created a network of medical providers that submitted thousands of false claims to the Foreign Medical Program for services that were double billed, overpriced, unnecessary, or never provided. The VA Office of Inspector General estimated a loss to VA of approximately $67 million. Therefore, amounts reimbursed to providers in Panama are likely inflated. For more information, see https://www.va.gov/health/foreign_medical_program_alerts.asp, accessed on October 3, 2024. See also VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights.
[30]According to our review of Foreign Medical Program documentation, outpatient claims include, but are not limited to, office visits, ambulatory surgery, supplies, physical therapy, psychotherapy, professional services in an inpatient setting, or any other procedure that does not require hospitalization or fall into one of the other types of service. Conversely, inpatient claims must have an admission and discharge date for processing. In addition, inpatient submissions may also include professional fees for room visits and physical therapy.
[31]If a claims examiner does not approve the claim, for example because the services do not qualify as eligible expenses, the Foreign Medical Program is to send an explanation of benefits to the veteran and the provider, if the provider submitted the claim.
[32]Foreign Medical Program officials said that 10-50 undeliverable checks per week was not high compared to the number of processed claims. For example, according to VHA data, the program processed about 204,000 claims in fiscal year 2024. Based on estimates from Foreign Medical Program officials, the annual number of undeliverable checks could be up to 2,600 checks per year.
[34]Our prior work identified government and industry leading practices for documenting plans for legacy systems. For more information, see General Services Administration, Unified Shared Services Management, Modernization and Migration Management (M3) Playbook; M3 Playbook Guidance; American Technology Council, Report to the President on Federal IT Modernization; Office of Management and Budget, Strengthening the Cybersecurity of Federal Agencies; American Council for Technology-Industry Advisory Council, Legacy System Modernization; and Dawson, Arizona State University, IBM Center for The Business of Government, A Roadmap for IT Modernization in Government.
[35]31 U.S.C. § 3332 requires all federal payments, except for payments under the Internal Revenue Code, to be made through electronic funds transfer unless the Secretary of the Treasury issues a waiver.
[36]For example, Foreign Medical Program officials told us that many providers in Central America and the Caribbean use U.S. post office box and courier services to receive reimbursements rather than have payments sent directly to their foreign addresses. According to these officials, the majority of Foreign Medical Program payments sent to post office boxes are reimbursements to providers, particularly in Central America.
[37]The Department of the Treasury set a goal to increase electronic payments by converting 4.5 million paper checks to electronic payment options by fiscal year 2025. For more information, see https://fiscal.treasury.gov/agency‑priority‑goal/, U.S. Department of the Treasury, Bureau of the Fiscal Service, accessed on December 10, 2024. To reach this goal, the Department of the Treasury partners with agencies to identify challenges and to support agencies in issuing electronic payments to improve speed and security.
[38]International Treasury Services, a program of the Bureau of the Fiscal Service within the Department of the Treasury, is a web application that enables federal agencies to make international payments to over 240 countries in 150 different currencies. There is no cost to federal agencies to use this system and multiple payment methods are available including electronic payment.
[39]Foreign Medical Program officials provided documentation outlining tasks and competencies that claims examiners need to carry out their respective functions. According to our review of the documentation, these tasks include interpreting rules and regulations, and how to apply them to medical claims; coding medical diagnoses and procedures from descriptions with coding software or other applications; and reviewing claims to ensure processing information is present, among other responsibilities. In addition, competencies for claims examiners include attention to detail, computer skills, and knowledge of medical information and terminology related to diagnoses.
[40]Foreign Medical Program officials told us that these are specialty units that serve in multi-functional capacities—that is, that staff also assist with other VA family member programs, such as the Camp Lejeune Family Member Program, Children of Women Vietnam Veterans, and the Spina Bifida Health Care Benefits Program.
[41]According to Foreign Medical Program officials, the pre-determination process allows veterans to determine if they are able to receive reimbursement for treatment for a specific condition. Officials stated they expect the pre-determination process to improve predictability and help alleviate veterans’ concerns as to whether certain treatments will be covered, as well as improve transparency among veterans who use the Foreign Medical Program.
[42]VA’s Ask VA portal allows veterans, their families, caregivers, beneficiaries, dependents, or the general public to ask questions related to their VA benefits and services. For more information, see https://ask.va.gov/, U.S. Department of Veterans Affairs, accessed on October 2, 2024.
[43]We previously reported on claims processing timeliness in the Foreign Medical Program. See GAO‑19‑416 where we found that the Foreign Medical Program processed 53.8 percent of claims in 40 days in October 2018, compared to 70 percent of claims in 40 days in March 2019. However, we found that as of March 2019, VA was not meeting its timeliness goal to process 90 percent of claims reimbursements through the Foreign Medical Program in 40 days.
[44]VHA leadership set a zero-growth goal for its central office, which requires the Under Secretary for Health to approve any position requests that will result in the Assistant Under Secretary for Health and central office organization adding to its headcount level as of October 7, 2023. If hired, VHA officials said the 14 Foreign Medical Program positions would result in an increase to this non-cumulative full-time equivalent level as of October 7, 2023.
[45]Officials from the Office of Integrated Veteran Care stated that their office has limited resources to allocate in terms of staffing. In addition to the VHA central office’s zero-growth goal, officials said that the Foreign Medical Program first submits a staffing request through the Office of Integrated Veteran Care. Officials said that the staffing approval process takes time to move through approving teams, such as human resources and budget liaisons. Officials from the Office of Integrated Veteran Care noted the budget group determines whether funding is available for positions, and requests are then routed through the Deputy Assistant Under Secretary for Health and must be approved by the Acting Assistant Under Secretary for Health in the Office of Integrated Veteran Care.
[46]See GAO‑02‑373SP.
[48]Officials from the Office of Integrated Veteran Care told us they hope to have their internal controls framework in place by March 2025.
[49]Office of Integrated Veteran Care directorates coordinate enterprise risk reporting through their designated risk manager, according to the playbook. The playbook outlines enterprise risk management principles and approaches to integrate with fraud, waste, and abuse, such as control and monitoring activities. According to VA officials, since 2022, VHA has begun maturing programs, policies, and systems to address the fragmented management and governance functions that impede its ability to perform risk-informed decision making and proactive problem resolution. Part of this effort includes long term strategy development for programs to address fraud, waste, and abuse risk assessment and internal control needs.
[50]VHA established the Office of Integrated Veteran Care in June 2022. Prior to the establishment of this office, the fraud, waste, and abuse team was situated under the Office of Community Care, the predecessor to the Office of Integrated Veteran Care.
[51]Foreign Medical Program officials said supervisors and leads are to perform audits of claims over $20,000. Program officials told us the program raised the threshold for this audit of claims in August 2023, from $5,000 to $20,000, due to capacity issues and volume of the claims. According to Office of Integrity and Compliance officials, the office monitors veterans or providers for suspected fraud. Office of Integrity and Compliance officials said reviews of a payment to a veteran or provider can occur before or following payment. According to the Watch List policy, claim submissions from a veteran or provider on the list are to be printed out and sent to the Office of Integrity and Compliance for review. According to VA officials, as of January 2025, ownership of the Watch List is in transition to the Foreign Medical Program.
[52]Effectively assessing fraud risks involves documenting the key findings and conclusions from the key elements of a fraud risk assessment in a fraud risk profile, including the analysis of the types of fraud risks, their perceived likelihood and impact, risk tolerance, and the prioritization of risks. The fraud risk profile is an essential piece of an overall antifraud strategy and can inform the specific control activities managers design and implement.
[53]The Department of the Treasury’s Office of Payment Integrity helps federally funded programs make decisions to identify, prevent, and recover fraud and improper payments. For more information, see https://paymentintegrity.treasury.gov/paymentintegrity/, accessed December 16, 2024.
[54]VA Office of Inspector General, Department of Veterans Affairs Office of Inspector General: August 2023 Highlights.
