DEFENSE HEALTH CARE
Actions Needed to Address Long-Standing Management Challenges with Medical Facilities
Report to Congressional Committees
United States Government Accountability Office
For more information, contact Rashmi Agarwal at AgarwalR@gao.gov.
Highlights of GAO‑25‑107432, a report to congressional committees
Actions Needed to Address Long-Standing Management Challenges with Medical Facilities
Why GAO Did This Study
DOD realigned its medical facilities from the military departments to DHA in response to legislative reforms initiated in 2016. These reforms were intended to create a more efficient oversight structure for these facilities that would lower costs while improving care for military service members and eligible beneficiaries.
Section 714 of the National Defense Authorization Act for Fiscal Year 2024 includes a provision prohibiting DOD from advancing beyond phase one of DHA’s plan to establish its network structure until GAO assesses and reports on DHA’s transition efforts. Among other objectives, this report 1) describes how plans to manage medical facilities have changed, and 2) assesses the extent to which DHA has determined resources it needs to manage its facilities.
GAO reviewed policies, guidance, and other documentation related to DHA’s organizational efforts. GAO interviewed DOD and DHA officials, including those from the network structure’s nine management offices. GAO also spoke with officials from a nongeneralizable sample of six medical facilities about current and prior organizational structures.
What GAO Recommends
GAO is making seven recommendations, including that DOD provide information to Congress on how the network structure meets the intent of a statute; issue guidance and develop an implementation plan to validate personnel requirements; and study business functions and develop an implementation plan to consolidate them. DOD concurred with GAO’s recommendations.
What GAO Found
To assume responsibility for the management of medical facilities from the military departments, the Department of Defense’s (DOD) Defense Health Agency (DHA) began to implement an organizational structure called the market structure in January 2020. Subsequently, DHA replaced the market structure with the network structure in October 2023 to address challenges identified in the market structure. The similarities and differences in these structures are mainly in whether the structures are organized by military department affiliation, the number of management offices, and the rank of management office leaders.
|
Organizational structure |
Primarily organized by military department affiliation |
Number of management offices |
Number and rank of management office leaders |
|
Market |
No |
22 |
7 General or Flag Officers 15 Captains or Colonels |
|
Network |
Yes |
9 |
9 General or Flag Officers |
Source: GAO analysis of Department of Defense and Defense Health Agency (DHA) information. | GAO-25-107432
While DHA has started implementing a network structure, it has not fully determined all the resources it needs. Specifically,
·
DHA determined it needed nine offices to manage its resources
under the network structure. However, DHA has not explained to Congress how
this structure meets the intent of a statute. For example, DHA is limited to
establishing no more than two regions within the continental United States and
no more than two regions outside the continental United States to manage its
medical facilities. Until DHA provides such information, Congress risks not
having reasonable assurance that DHA is implementing an effective
organizational structure that, among other things, fully integrates the
military departments' medical capabilities and enhances joint medical
operations.
·
DHA has not fully determined and validated how many personnel
resources are required to manage and support its medical facilities. DHA has
not completed these efforts because it has not issued guidance that details the
processes needed to determine and validate personnel requirements, including by
analyzing workload. Additionally, DHA has not developed a plan to implement
such guidance, once issued, for these efforts. Without issuing detailed
guidance and developing an implementation plan, DHA lacks the information it
needs to establish personnel requirements to accomplish its objectives and
track its progress.
· DHA has not determined how it will consolidate business functions (e.g., clinical quality management and information technology) to save on costs because it has not studied them. DHA has also not developed an implementation plan for consolidating these functions. By studying its functions and developing an implementation plan to track progress in consolidating them, DHA will be better positioned to ensure these functions are structured to manage its medical facilities as efficiently and effectively as possible.
Abbreviations
|
Assistant Secretary |
Assistant Secretary of Defense for Health Affairs |
|
DHA |
Defense Health Agency |
|
DOD |
Department of Defense |
|
medical facilities |
military medical treatment facilities |
|
Under Secretary |
Under Secretary of Defense for Personnel and Readiness |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
April 10, 2025
The Honorable Roger Wicker
Chairman
The Honorable Jack Reed
Ranking Member
Committee on Armed Services
United States Senate
The Honorable Mike Rogers
Chairman
The Honorable Adam Smith
Ranking Member
Committee on Armed Services
House of Representatives
In response to sweeping legislative reforms initiated in December 2016, the Department of Defense (DOD) transferred the management of its hospitals, medical centers, and clinics—collectively referred to as military medical treatment facilities (medical facilities)—from the military departments to the Defense Health Agency (DHA).[1] These organizational reforms were intended to create a more efficient oversight structure for the medical facilities that would lower costs while improving beneficiary care.
Beginning in March 2017 through June 2018, DOD provided the Senate and House Armed Services Committees with four reports containing different plans to accomplish the transfer of management for the medical facilities from the military departments to DHA.[2] In November 2022, DHA completed its multiyear transition of medical facilities from the military departments, making DHA responsible for the management of 736 medical facilities in the United States and overseas.[3] As part of the transition, DHA established the market organizational structure (hereafter referred to as the “market structure”) comprised of 22 management offices to manage its medical facilities.[4] In October 2023, DHA replaced the market structure with a new organizational structure referred to as the network organizational structure (hereafter referred to as the “network structure”) comprised of nine management offices to manage its medical facilities.
Section 714 of the National Defense Authorization Act for Fiscal Year 2024 includes a provision prohibiting DOD from advancing beyond phase one of DHA’s plan to establish the network structure until we assess and report on DHA’s transition efforts.[5] This report (1) describes how plans to manage the medical facilities have changed under DHA, (2) assesses the extent to which DHA has determined what resources it needs to manage its medical facilities under the network structure, and (3) assesses the extent to which DHA involves stakeholders to implement the network structure for managing its medical facilities.
To address our objectives, we reviewed relevant legislation, DOD and DHA policies and guidance, other documentation related to medical facilities, and our prior work related to DHA’s implementation of organizational structures to manage its medical facilities. We interviewed officials from DHA, Office of the Secretary of Defense, Office of the Joint Staff Surgeon, and military medical headquarters organizations.[6] We also interviewed officials from each of the nine network structure management offices. Additionally, we selected a nongeneralizable sample of six parent medical facilities and interviewed officials in-person and virtually.[7] We selected them based on medical facilities’ data, including geographic location, a range in the number of beneficiaries served, the management office director’s military department, and whether the medical facilities were managed by the Army, the Navy, or the Air Force prior to their transition to DHA. Additionally, we interviewed officials from two selected combatant commands—U.S. European Command and U.S. Indo-Pacific Command—which coincide with two management offices.[8]
We also took specific actions to address each of our objectives.
· Objective 1. We reviewed DOD and DHA documentation, legislation, a congressional conference report, and our prior reports to describe how DHA’s plans compare or differ.[9]
· Objective 2. We reviewed DOD and DHA reviews and assessments, legislation, and our prior work on DHA’s efforts to transition and manage its medical facilities.[10] We assessed the network structure’s consistency with the structure specified in section 712 of the John S. McCain National Defense Authorization Act for Fiscal Year 2019.[11] We also assessed DHA’s efforts on working with key stakeholders, such as Congress, to understand and fulfill their expectations for the organization of this structure in accordance with federal internal control standards.[12]
We also assessed DHA’s efforts against DOD guidance on DHA’s role in developing technical guidance, regulations, and instructions, among other responsibilities, to support the Assistant Secretary of Defense for Health Affairs in the administration of all medical and dental programs.[13] We assessed these efforts against DOD policy stating that personnel requirements are driven by workload and that existing DOD policies, procedures, and structures shall be periodically evaluated to ensure efficient and effective use of personnel resources.[14] We further assessed these efforts against DHA’s Strategic Plan on effectively managing the agency’s total workforce in a timely manner; selected leading agency reform practices, in particular the need to develop implementation plans to track progress; and DOD policy directing the DHA Director to develop appropriate processes to assume responsibility for particular functions and support the conduct of studies and research activities to manage and implement health policies.[15]
· Objective 3. We reviewed DOD and DHA documentation, including summaries of 2023 and 2024 responses to a DHA survey on the market and network structures; charters on coordinating with military department and Joint Staff Surgeon officials; and briefings, testimonies, and reports to Congress.[16] We assessed DHA’s efforts against DOD policy related to the DHA Director’s responsibilities.[17] We also analyzed DHA’s efforts against selected leading agency reform practices and, specifically, those related to the need for agencies to continuously involve stakeholders and Congress in the development of reforms and reorganizations.[18]
We assessed the reliability of the medical facilities’ data from July 2024 by interviewing DHA officials to determine how data are collected, analyzed, and reported, and to obtain their perspectives on any associated limitations as well as on efforts to address these limitations. We found these data to be sufficiently reliable for our purposes. As a result, we used the data to support our selection of parent medical facility directors to interview and to report the total number and military department affiliation of the parent medical facilities under DHA’s management offices.
We conducted this performance audit from February 2024 to April 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Overview of DOD’s Military Health System and Key Organizations
DOD’s military health system is a complex enterprise overseen by the Secretary of Defense. Within this enterprise, DHA is responsible for health care delivery and shares the responsibility for medical readiness with the three military departments. Figure 1 illustrates the leadership and organizational structure of DOD’s military health system.
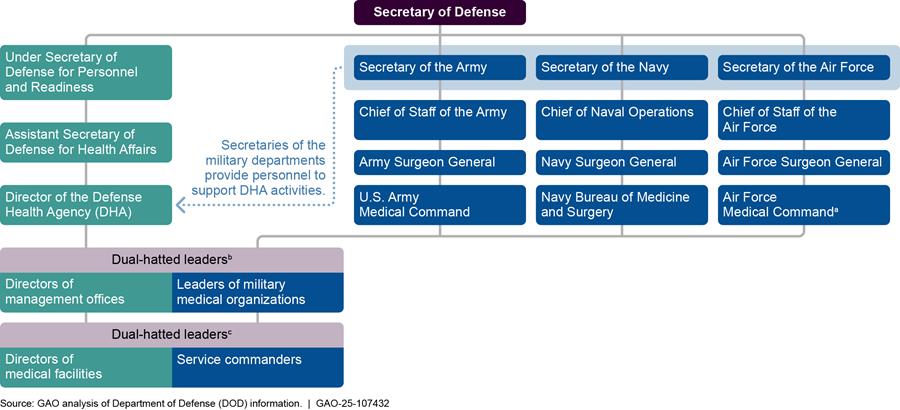
aAir Force Medical Command was established on August 15, 2024, according to Air Force officials, and achieved its initial operational capability on March 12, 2025. Air Force, “Air Force Medical Command reaches initial operating capability” (Falls Church, VA: March 13, 2025), accessed on March 27, 2025. https://www.af.mil/News/Article-Display/Article/4119515/air-force-medical-command-reaches-initial-operating-capability/.
bEight of the nine directors of the management offices are dual-hatted, that is, they also hold a leadership position in their respective military medical organization, according to DHA officials. Specifically, the directors of the Atlantic, Central, Continental, East, Europe, Indo-Pacific, Pacific Rim, and West management offices are dual-hatted. The management office director for the ninth office, the National Capital Region, does not hold a leadership position in a military medical organization, according to these officials.
cDual-hatted medical facility directors or service commanders are military service officers. As facility directors, they exercise authority, direction, and control of all facility operations and over all personnel assigned or performing work duties at the facility, among other responsibilities. As service commanders, they exercise administrative control in the facilities; exercise command and control over military medical personnel assigned to DOD medical facilities executing military service duties (e.g., planned and unplanned deployments, military operations, training, and exercises); establish personnel training requirements; and provide advanced notice to the DHA Director of personnel participation therein, among other responsibilities.
The leaders and supporting organizations listed in the figure above have unique roles in DOD’s military health system. For example:
· The Under Secretary of Defense for Personnel and Readiness (the Under Secretary) is the principal staff assistant and advisor to the Secretary of Defense for health-related matters, and, in that capacity, is responsible for developing policies, plans, and programs for health and medical affairs.[19]
· The Assistant Secretary of Defense for Health Affairs (the Assistant Secretary) serves as the principal advisor to the Under Secretary for all DOD health-related policies, programs, and activities.[20] The Assistant Secretary has the authority to develop policies; conduct analyses; issue guidance; provide advice and make recommendations to the Secretary of Defense, the Under Secretary, and others; and provide oversight on matters pertaining to the military health system. Further, the Office of the Assistant Secretary is responsible for preparing and submitting a DOD unified medical program budget for the military health system, which totaled $61.4 billion for the fiscal year 2025 budget request.[21]
· The Director of DHA is a three-star General or Flag Officer who functions under the authority, direction, and control of the Assistant Secretary.[22] As such, the Director manages, among other things, the execution of policies issued by the Assistant Secretary and the Defense Health Program appropriation.[23] In December 2016, the National Defense Authorization Act for Fiscal Year 2017 expanded the role of DHA by directing the transfer of responsibility for the administration of each medical facility from the military departments to DHA.[24] Specifically, the Director of DHA is responsible for budgetary matters, information technology, health care administration and management, administrative policy and procedure, and military medical construction, among other things.
In addition, the Director of DHA is to coordinate with the Joint Staff Surgeon to ensure the Director most effectively carries out the responsibilities of DHA as a combat support agency.[25] The Director is also responsible for ensuring the medical facilities deliver high-quality care, meeting the military departments’ health care requirements and providing the necessary clinical workload to meet the military departments’ medical readiness requirements.[26]
· The Secretaries of the military departments coordinate with the Assistant Secretary to develop certain military health system policies, standards, and procedures. They also provide military personnel and other authorized resources to support the activities of DHA, among other things.[27] They are also responsible for ensuring the readiness of military personnel and providing military personnel and authorized resources in support of the 11 combatant commanders and DHA.[28]
Each military department maintains one or more medical headquarters organizations, which are responsible for developing and maintaining the readiness of medical personnel. These organizations include the U.S. Army Medical Command, the Navy Bureau of Medicine and Surgery, and the Air Force Medical Command.[29] The Surgeon General of each respective military department leads the medical headquarters organization and serves as the principal advisor to the Secretary of the military department concerning all health and medical matters of that military department, with the support of their respective Deputy Surgeon General, according to military department officials.
Establishment of DHA and Overview of Medical Facilities
DHA was established on October 1, 2013, as a defense agency under the authority, direction, and control of the Under Secretary through the Assistant Secretary.[30] At that time, DHA’s mission was to manage shared services, such as pharmacy, health information technology, and medical research and development.[31] Legislative reforms expanded DHA’s mission in December 2016 to include managing the department’s medical facilities.[32] The John S. McCain National Defense Authorization Act for Fiscal Year 2019 further expanded the responsibilities of DHA by establishing additional requirements for the transition of medical facilities and mandating the reorganization of public health, medical research, and development capabilities from the military departments to DHA, among other things.[33]
In fiscal year 2023, there were 736 medical facilities in the United States and overseas supporting health care delivery and the readiness of military health care providers and service members.[34] These facilities vary in size and capabilities and consist of large “parent facilities”—such as ambulatory surgery centers, hospitals, and medical centers—and small “child facilities,” such as behavioral health clinics.[35] Medical facility workforces include health care providers such as physicians (both primary and specialty care providers), nurses, and enlisted specialists who assist with medical procedures, as well as administrative and support personnel. In fiscal year 2023, DOD’s medical facility workforces included approximately 49,000 active-duty military personnel, augmented by nearly 41,000 federal civilian employees and about 14,500 contractor personnel.
The primary purpose of medical facilities is to support the readiness of military health care providers and service members, according to DOD Instruction 6000.19.[36] Specifically, each medical facility must spend most of its resources supporting wartime skills, the development and maintenance of military medical personnel, or the medical evaluation and treatment of service members.[37] To that end, medical facilities serve as training and readiness platforms for active-duty medical providers.[38]
DHA’s Plans for Managing Its Medical Facilities Have Changed in Affiliation with Military Departments, Number of Offices, and Rank of Leaders of These Offices
DHA developed plans for four different organizational structures—named the component, intermediate management, market, and network structures—at various points in time, to assume the responsibility for the management of medical facilities from the military departments as directed by Congress in 2016. DHA did not implement the component and intermediate management structures but did implement the market and network structures. See figure 2 for a timeline of DHA and DOD efforts to develop these four organizational structures.
Figure 2: Transition of Medical Facilities to DHA and DOD Efforts to Develop Organizational Structures Since 2016
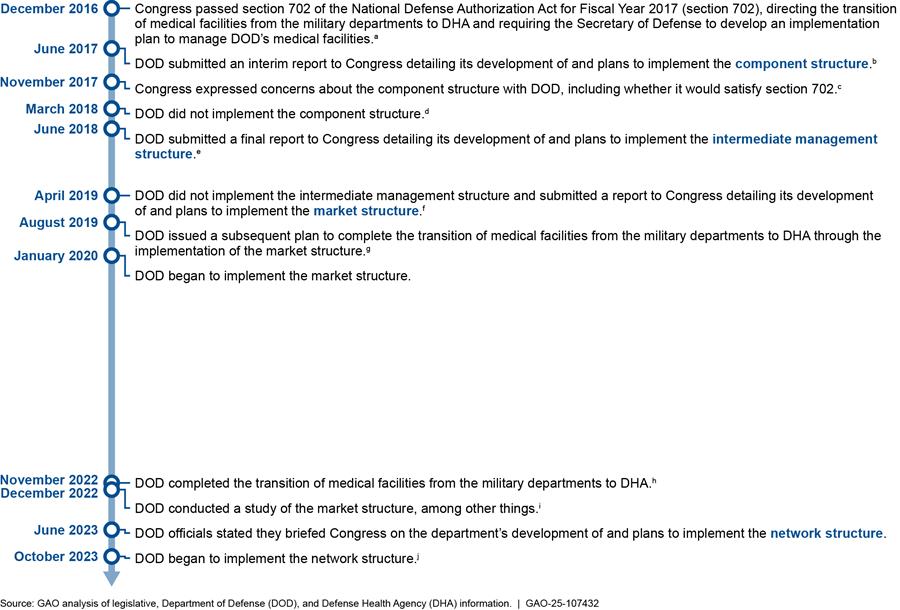
aPub. L. No. 114-328, 702 (2016), codified as amended at 10 U.S.C. 1073c.
bDepartment of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Second Interim Report (June 30, 2017).
cH.R. Rep. No. 115-404, at 849-50 (2017) (Conf. Rep.).
dDOD decided, after deeper analysis and discussions with Congress, that the component structure did not adequately satisfy the requirements of subsection (a) of section 1073c. Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Preliminary Draft Plan to Implement 1073c of Title 10, United States Code, Interim Report (Mar. 31, 2018).
eDepartment of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Final Plan to Implement Section 1073c of Title 10, United States Code, Final Report (June 30, 2018).
fDepartment of Defense, Report to Armed Services Committees, Section 712 of the John S. McCain National Defense Authorization Act for Fiscal Year 2019 (Public Law 115-232), “Organizational Framework of the Military Healthcare System to Support the Medical Requirements of the Combatant Commands” (Apr. 17, 2019). We requested information on the factors that led to DHA’s decision to not implement the intermediate management structure. In December 2024, DHA officials stated the factors were unknown, and they did not have any documentation related to the decision.
gDefense Health Agency, Plan 3: Implementation Plan for the Complete Transition of Military Medical Treatment Facilities to the Defense Health Agency, Version 6.0 (Aug. 12, 2019).
hDefense Health Agency Memorandum, Completion of Military Medical Treatment Facility Realignment of Personnel, Property, and Systems at Set 3 Locations (Nov. 30, 2022).
iDefense Health Agency, Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022).
jSection 714 of the National Defense Authorization Act for Fiscal Year 2024, enacted in December 2023, includes a provision prohibiting DOD from advancing beyond phase one of DHA’s plan to establish the network structure until GAO assesses and reports on DHA’s transition efforts. Pub. L. No. 118-31, 714 (2023). According to DHA officials, DHA has not taken the necessary steps to reach full operating capability for its network structure as a result of section 714. Specifically, a DHA official told us that these steps include restructuring headquarters and transferring personnel and financial systems.
These structures’ similarities and differences were mainly in the organization of their management offices, which manage the medical facilities. In all four structures, the medical facilities report directly to the management offices and the management offices report directly to DHA headquarters. In comparing DHA’s plans to manage its medical facilities, we found similarities and differences—as shown in table 1 below—in (1) military department affiliation, (2) the number of management offices identified as necessary under each structure, and (3) the number and rank of management office leaders.[39] For example, most management offices under the network structure, and medical facilities that comprise the network structure, are primarily organized by their affiliation with the military departments, similar to the component structure. In contrast, the management offices for the intermediate management and market structures were primarily organized based on geographic proximity of the medical facilities, among other things.
Table 1: DHA Organizational Structures to Manage Military Medical Treatment Facilities Since 2017, by Military Department Affiliation, Number of Management Offices, and Number and Rank of Leaders
|
Organizational structure |
Primarily organized by military department affiliation |
Number of management offices |
Number and rank of management office leaders |
|
Component structurea |
Yes |
3 |
3 General or Flag Officersb |
|
Intermediate management structurec |
No, primarily organized based on geographic proximity of medical facilities, among other things |
6 |
Unknownd |
|
Market structuree |
No, primarily organized based on geographic proximity of medical facilities, among other things |
22 |
7 General or Flag Officers 15 Captains or Colonelsf |
|
Network structureg |
Yes |
9h |
9 General or Flag Officers |
Source: GAO analysis of Department of Defense and Defense Health Agency (DHA) information. | GAO‑25‑107432
aDepartment of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Second Interim Report (June 30, 2017).
bGeneral or Flag Officers have the authority to move personnel to fill gaps across medical facilities under their management office, according to DHA officials.
cDepartment of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Final Plan to Implement Section 1073c of Title 10, United States Code, Final Report (June 30, 2018).
dWe also requested information regarding the proposed number and rank of appointed leaders for the intermediate management structure. In December 2024, DHA officials stated that such information was unknown and not documented.
eDefense Health Agency, Plan 3: Implementation Plan for the Complete Transition of Military Medical Treatment Facilities to the Defense Health Agency, Version 6.0 (Aug. 12, 2019).
fColonels and Captains do not have the authority to move personnel to fill gaps across medical facilities under their management office, unlike General or Flag Officers, according to DHA officials.
gSee Pub. L. No. 118-31, 714(a) (2023).
hThe network structure includes nine management offices that report to DHA headquarters and manage the medical facilities. This structure also includes a Defense Health Support Activity office within DHA headquarters that supports the network structure’s management of the medical facilities. However, because the Defense Health Support Activity office is not a management office, it is not included in the total number of nine management offices of the network structure.
In January 2020, DHA began implementing the market structure but faced difficulties staffing it.[40] Specifically, in 2023, we reported that DHA had not studied and validated the number of personnel required to conduct the work of the market structure’s 22 management offices, and that DHA had overestimated the personnel it needed to support the offices’ workload.[41]
DOD conducted three studies of the market structure between August 2022 and April 2023, according to DHA officials.[42] In these studies, DOD identified the following lessons learned about the market structure.
· Challenges coordinating with military medical organizations. Coordination with the military departments was variable within the market structure, and the interface between DHA and the military departments needed to be improved.[43]
· Too many management offices. The market structure had too many management offices that were directly reporting to DHA headquarters.[44]
· Inconsistent leadership of the management offices. Management office directors that were not General or Flag Officers did not have the capability to serve as intermediaries between DHA headquarters and the medical facilities.[45] As a result, many concerns had to be elevated to DHA headquarters, resulting in inefficiencies, according to DHA officials.
· Resource intensive. The design of the market structure was “suboptimal” because, for example, it was resource intensive, requiring more personnel than DHA had.[46]
To address these challenges, DHA replaced the market structure with the network structure on October 1, 2023, according to DHA officials.[47] The network structure (1) aligned the management offices more closely with the military departments and considered geographic location, (2) reduced the number of management offices directly reporting to DHA headquarters, and (3) assigned management office leaders at the General or Flag Officer level. According to DHA officials, these changes would enable DHA and the military departments to share budgetary and personnel resources, respectively, across the medical facilities. Figure 3 describes the military department affiliation of each management office and the parent medical facilities these offices manage.
Figure 3: DHA’s Network Structure, by Management Office, Parent Military Medical Treatment Facilities (Parent Medical Facilities) Managed, and DHA and Military Department Affiliation as of June 2024
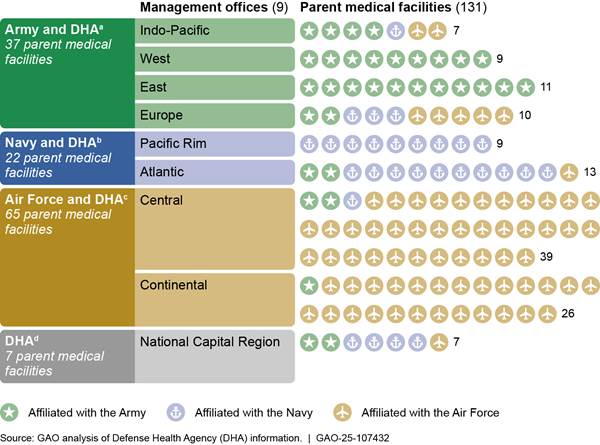
aThese management offices are led by a director who also holds a leadership position within an Army medical organization.
bThese management offices are led by a director who also holds a leadership position within a Navy medical organization.
cThese management offices are led by a director who also holds a leadership position within an Air Force medical organization.
dThis management office is led by a director who does not hold a leadership position within a military medical organization.
An example of the benefit of this alignment is the Pacific Rim management office. The director of that office is a Navy Flag Officer who also holds a leadership position within Navy Medical Forces Pacific, a Navy medical organization. Military medical personnel assigned to medical facilities that are under the Pacific Rim management office are generally affiliated with the Navy, according to DHA officials. Because the Pacific Rim director holds a dual-hatted position as a Navy leader within both the management office and the medical organization, this director has the authority to move Navy military medical personnel to fill personnel gaps within other medical facilities that are under the Pacific Rim management office, according to these same officials.
In some cases, medical facilities are assigned to management offices based on geographic location rather than the military department affiliation of the management office director. The network structure retained some of the long-standing, collaborative working relationships under the market structure between medical facilities within the same geographic location, according to DHA officials. These officials also stated that these facilities provided health care services to overlapping and shared populations. Therefore, the facilities remained grouped together under the same management office of the network structure, according to the same DHA officials. For example, Brooke Army Medical Center and the 59th Medical Wing are affiliated with different military departments and are both located in San Antonio, Texas. These medical facilities had a collaborative relationship under the market structure to achieve resource and scheduling efficiencies, according to a DHA official.
Another example of DHA assigning medical facilities to management offices based on geographic location is the assignment of Naval Health Clinic Hawaii to the Indo-Pacific management office. This medical facility is affiliated with the Navy, and the Indo-Pacific management office is led by a director who is an Army General Officer and also holds a position within Army Medical Readiness Command, Pacific, an Army medical organization. DHA assigned Naval Health Clinic Hawaii to the Indo-Pacific management office because the clinic provides personnel support to other medical facilities in the Indo-Pacific region that are not affiliated with the Navy, according to a DHA official.[48] Naval Health Clinic Hawaii provides this personnel support through coordination between its Indo-Pacific management office director and the management office directors of the medical facilities in the Pacific Rim and Central management offices of in the Indo-Pacific region, according to the same official.
DHA Has Determined Some but Not All of the Resources Needed to Manage Its Medical Facilities Under the Network Structure
DHA has determined some resources it needs to manage its medical facilities under the network structure, including the number of offices needed to manage its resources. However, the number of management offices it established may not be consistent with a statute. Moreover, DHA has not fully determined and validated the personnel it requires to manage and support its medical facilities or determined how it will consolidate business functions under the network structure.
The Number of Management Offices DHA Determined for the Network Structure May Not Be Consistent with a Statute
As part of establishing the network structure in October 2023, DHA determined that it needed nine management offices to serve as intermediaries between DHA headquarters and the medical facilities. Additionally, DHA established a Defense Health Support Activity office to support its nine management offices.[49] The network structure’s reliance on nine management offices is similar to that of the market structure, which used 22 management offices that served as intermediaries between DHA headquarters and the medical facilities. However, in reviewing the previous market structure in 2023, we reported that it may have been larger than, and inconsistent with, the structure specified in section 712 of the John S. McCain National Defense Authorization Act for Fiscal Year 2019.[50]
Specifically, section 712 mandates that there should be no more than two DHA regions within the continental United States, and no more than two DHA regions outside the continental United States.[51] Additionally, section 712 specifies that each DHA region within the United States should be led by a commander or director who is a member of the armed forces and not higher than a major general or rear admiral. This statute mandates that DHA establish an effective organizational structure that, among other things, integrates the military departments’ medical capabilities to enhance joint military medical operations.
Consistent with this statute, DHA’s previous market structure established two regions—that is, management offices—outside the continental United States that were led by a director who was a member of the armed forces and not higher than a major general or rear admiral. However, there were 20 additional management offices within the continental United States, instead of two regions as specified by section 712. These offices were led by a director who was a member of the armed forces and not higher than a major general or rear admiral. According to a DHA senior leader, DHA considered all the management offices located within the continental United States to be a single region, although it did not use the term “region” in its organizational structure. We reported in 2023 that the structure of the largest management offices within the continental United States paralleled that of the two regions outside the continental United States in terms of the number and types of medical facilities, the population of beneficiaries served, and the leadership and staffing framework.
In 2023, we recommended that DHA reevaluate its organizational approach for the market structure and use its conclusions to study and validate the personnel required to manage its medical facilities. DHA concurred and partially addressed this recommendation by studying the market structure. As we noted earlier, DHA relied on internal studies of the market structure to conclude that it needed fewer management offices directly reporting to DHA headquarters and that the offices should better align with the military departments, according to DHA officials.[52]
As a result, DHA established two management offices outside the continental United States and seven management offices within the continental United States under the current network structure. These management offices are led by a director who is a member of the armed forces and not higher than a major general or rear admiral, which we found is consistent with the statutory requirement for leadership within section 712.[53] However, the current network structure with its nine management offices may be inconsistent with the structure specified in section 712.
DHA officials stated the network structure is consistent with section 712 because the structure does not include regions but is instead aligned with the military departments. Moreover, DHA officials said there are no definitions of “markets” or “regions” (i.e., management offices) under section 712, resulting in ambiguity in determining its organizational structures over time. DHA officials also stated that the DHA Director has authority to determine the most efficient and effective organizational structure to manage its medical facilities within the resources available, in accordance with DOD Directive 5136.13. This directive states that the DHA Director organizes, directs, and manages the DHA and all assigned resources.
DHA officials told us they briefed Congress on their plans to implement the network structure in June 2023. However, they also stated that they did not discuss with Congress if and how the network structure was consistent with the statute or seek clarification on the definition of markets or regions. As a result, DHA officials stated they were not aware of any concerns that the network structure is not compliant with the law.
Standards for Internal Control in the Federal Government state that an oversight body should oversee the entity’s internal control system. In doing so, the oversight body can work with key stakeholders, such as Congress, to understand their expectations and help the entity fulfill these expectations if appropriate.[54] However, DHA has not provided information to Congress to clarify how the network structure meets the intent of section 712. Until DHA provides such information, Congress risks not having reasonable assurance that DHA is implementing an effective organizational structure that, among other things, integrates the military departments’ medical capabilities and enhances joint military medical operations.
DHA Identified Positions for the Network Structure but Has Not Fully Determined and Validated the Number of Personnel Required
DHA identified standardized positions for the management offices to implement its network structure.[55] However, DHA has not fully determined and validated the number of personnel required to manage and support its medical facilities, including by conducting workload analyses.
DHA identified standardized positions for the network structure. DHA identified standardized functions performed at the management office level, to include the patient experience, legal, and budget functions.[56] To carry out these functions, DHA identified standardized positions for the management offices, according to DHA officials. DHA also:
· Identified positions for the Defense Health Support Activity office based on input from headquarters personnel and lessons learned from the market structure, according to DHA officials. In identifying positions needed for this office, DHA analyzed the Defense Health Support Activity’s ability to respond to requests from the nine management offices.[57] DHA based this analysis on input from management office directors and Defense Health Support Activity office officials, according to DHA officials.
· Standardized the roles and responsibilities of personnel for the nine management offices of the network structure and identified factors that affect workload (i.e., the amount of work that organizations or individuals perform or are responsible for performing), according to DHA officials. These factors include missions, capabilities, and capacities needed to manage DHA’s medical facilities.
|
Prior GAO Recommendations to Address DHA’s Long-Standing Personnel-Related Challenges We have made multiple recommendations to address the Defense Health Agency’s (DHA) personnel-related challenges, including: · In August 2023, we found that DHA had not studied and validated its personnel requirements for the market structure. At that time, officials told us that they had not evaluated personnel requirements because it would require more time to understand the workloads of management office staff within the new structure (i.e., the market structure), among other things. As a result, we recommended that DHA reevaluate its organizational approach for the market structure and use the conclusions to study and validate the personnel required to manage the medical facilities. While DHA concurred and partially addressed this recommendation by studying the market structure, it has not provided evidence that it has studied workload and validated personnel requirements. · In October 2018, we found that the Department of Defense (DOD) had not validated DHA headquarters-level personnel requirements and recommended that the department do so. DOD concurred with our recommendation but has not yet implemented it. DOD issued a memorandum in December 2023 requiring the department to conduct a comprehensive review of all personnel requirements by June 30, 2024. As of January 2025, we continue to monitor DOD’s efforts to implement this recommendation. Source: GAO analysis of prior work. See GAO, Defense Health Care: DOD Should Reevaluate Market Structure for Military Medical Treatment Facility Management, GAO‑23‑105441 (Washington, D.C.: Aug. 21, 2023); and GAO, Defense Health Care: DOD Should Demonstrate How Its Plan to Transfer the Administration of Military Treatment Facilities Will Improve Efficiency, GAO‑19‑53 (Washington, D.C.: Oct. 30, 2018). I GAO‑25‑107432 |
DHA has not fully determined and validated the number of personnel required. Although it identified standardized positions for the management offices and the Defense Health Support Activity office, DHA has not analyzed workload to fully determine how many personnel are required to manage and support the medical facilities, according to these same officials. Additionally, DHA officials stated that DHA has not validated the missions, capabilities, and capacities factors that would inform how many personnel it needs for its medical facilities.[58]
DHA has had long-standing personnel-related challenges, to include determining and validating personnel requirements, and we have made multiple recommendations to address these challenges (see sidebar).
DHA officials stated they currently rely on DOD Directive 1100.4 and DHA’s Procedural Instruction 1100.01 to guide their process for validating personnel requirements. Specifically, DOD Directive 1100.4 provides that personnel requirements are driven by workload and shall be established at the minimum levels necessary to accomplish mission and performance objectives.[59] The directive also states that military (active and reserve) and civilian personnel resources shall be programmed in accordance with, for example, validated personnel requirements. In May 2019, DHA issued Procedural Instruction 1100.01 for its personnel program to supplement DOD Directive 1100.4. This instruction also states that personnel requirements are driven by workload, in line with DOD Directive 1100.4, but does not include a detailed process for determining and validating personnel requirements, including analyzing workload.
DOD Directive 5136.13 provides that DHA develops technical guidance, regulations, and instructions, among others, to support the Assistant Secretary in the administration of all medical and dental programs. Moreover, DOD Directive 1100.4 specifies that, as a matter of policy, existing DOD policies, procedures, and structures shall be periodically evaluated to ensure efficient and effective use of personnel resources. Furthermore, in August 2022, a zero-based review on military and DHA medical headquarters organizations recommended that DHA develop processes, policies, and procedures for validating its personnel
|
Military Department Personnel Guidance Describing Workload We reviewed Army, Navy, and Air Force guidance to identify how it describes workload. We found that: Army guidance describes workload as the level of effort required to perform tasks and functions necessary to accomplish a mission. The guidance also provides a definition for workload management, which includes describing the work to be accomplished and estimating the time and resources required to accomplish the workload. Navy guidance describes workload as the amount of work that an organization is responsible for performing during a specified period. The guidance defines specific types of workload. For example, projected workload is defined as an amount of work proposed or anticipated in the future to meet the requirements of a program and function. Air Force guidance describes workload as a military capability and states that the focal point of analysis during the validation process is the number of personnel and workload reflected in the personnel system. In addition, the guidance states that the relationship between the number of personnel and workload is critical because it provides the linkage needed to define or identify the hours of work necessary to produce a military output. Source: GAO analysis of Army Regulation 570-4, Manpower Management (May 1, 2024); Office of the Chief of Naval Operations Instruction 1000.16L, Navy Total Force Manpower Policies and Procedures (June 24, 2015) (change transmittal 3, July 2, 2021); and Air Force Manual 38-102, Manpower and Organization Standard Work Processes and Procedures (July 5, 2024). I GAO‑25‑107432 |
requirements consistent with DOD Directive 1100.4.[60] However, DHA has not developed these documents. Specifically, DHA has not issued guidance that details the processes needed to determine and validate the number of personnel required to manage and support its medical facilities, including by analyzing workload and addressing the frequency with which these analyses should be conducted.
Officials from the Office of the Under Secretary of Defense for Personnel and Readiness stated that they have not issued strategic-level guidance to determine and validate personnel requirements for Fourth Estate entities, such as DHA, but anticipate developing such guidance in 2025.[61] However, they stated it is DHA’s responsibility to establish a process and detailed guidance on how to determine and validate the number of personnel required to manage and support its medical facilities. Such guidance could mirror related military department guidance (see sidebar) by including descriptions of workload and processes, such as modeling, functionality assessments, and analyses of alternatives, to analyze workload.[62]
DHA plans to develop a standard operating procedure to validate personnel requirements for DHA headquarters, the management offices, and the medical facilities, according to DHA documentation we reviewed.[63] However, this plan for developing the standard operating procedure does not include steps for conducting workload analyses to determine personnel requirements. Additionally, the plan does not provide details on the frequency with which these workload analyses should be conducted or how to validate personnel requirements. DHA officials told us that they are updating DHA Procedural Instruction 1100.01 and anticipate continuing to update it as they continue to determine and validate personnel requirements for the medical facilities and the network structure.
Without issuing guidance that details the processes needed to determine and validate the number of personnel required to manage and support its medical facilities, including a process to analyze workload and address how frequently these analyses should be conducted, DHA will not have the information it needs to establish personnel requirements to effectively accomplish mission and performance objectives.
Further, DHA’s Strategic Plan, issued in July 2023, includes a strategic initiative to effectively manage the agency’s total workforce in a timely manner.[64] Our prior work on leading agency reform practices shows that incorporating change management practices improves the likelihood of successful reforms.[65] These practices include developing an implementation plan with timelines and key milestones and deliverables to track its progress.
DHA has initiated an effort to standardize and document personnel requirements in its medical facilities, according to DHA officials. DHA is currently prioritizing analyzing workload and validating personnel requirements for its medical facilities, where the overwhelming majority of the agency’s personnel work, according to these same officials. After completing this effort, DHA plans to analyze workload and validate personnel requirements for DHA headquarters, the Defense Health Support Activity office, and the management offices, according to DHA officials. They added that DHA anticipates initiating this analysis and validation process for the network structure by the fourth quarter of fiscal year 2025 and expects to complete the process by the fourth quarter of fiscal year 2026.
In the interim, DHA has updated personnel requirements, authorizations (i.e., funded positions), and staffing numbers to reflect workload factors based on the mission, capabilities, and capacities needed to manage its medical facilities, according to DHA officials. DHA officials told us that they are identifying key milestones and deliverables for their plan to determine and validate personnel requirements for the network structure and acknowledged the need to document their implementation plan. However, DHA has not developed a plan to implement its guidance, once issued, to establish personnel requirements. This plan should include key milestones and deliverables to track its progress in determining and validating the number of personnel it requires, including analyzing workload, to manage and support its medical facilities. By developing such a plan, DHA will be better positioned to implement the guidance as intended and have the information it needs to track its progress on such efforts.
DHA Has Not Determined How It Will Consolidate Business Functions to Manage Its Medical Facilities Under the Network Structure
DHA has not determined how it will consolidate business functions—such as clinical quality management, contracting activity, information technology, and education and training—to manage its medical facilities. In 2023, we reported that DHA believed that future efficiencies in market structure staffing were possible through the consolidation of shared functions across locations, which would reduce the number of personnel needed to perform those functions.[66] Specifically, DHA officials noted that personnel conducting certain shared business functions, such as legal support, resource management, and information technology, among others, could be consolidated. Officials from three of six selected market offices we interviewed described plans or efforts to identify such consolidation opportunities across the medical facilities to support the management offices. However, those opportunities had not been implemented because the management offices were reviewing options or waiting for input from DHA headquarters, according to DHA officials. In April 2024, the DHA Director told us that DHA expects to gain efficiencies under the network structure that will result in future cost savings by consolidating business functions rather than by personnel right-sizing.
DHA has identified and defined the business functions assigned to DHA headquarters and the management offices to manage its medical facilities. For example, health informatics is a business function that determines how to troubleshoot information technology challenges and improves processes related to its electronic records system, according to DHA officials.[67] This function exists at the management offices and at the medical facility levels, and DHA uses the information obtained through this function to ensure workload is allocated across the entire military health system, according to these same officials.
DOD guidance directs the DHA Director to develop appropriate processes to assume responsibility most effectively and efficiently for particular functions, including shared functions.[68] Additionally, this guidance directs the DHA Director to support the conduct of studies and research activities to assist the Assistant Secretary of Defense for Health Affairs and others, as necessary, in support of their responsibilities and to support the management and implementation of health policies for the Military Health System developed by the Assistant Secretary. As previously mentioned, our prior work on leading agency reform practices includes a practice to develop an implementation plan with timelines and key milestones and deliverables to track the progress of implementation.[69] However, DHA has not studied its business functions to determine which ones it will consolidate or developed an implementation plan with timelines and key milestones and deliverables to track its progress consolidating these functions to manage and support its medical facilities.
In implementing the network structure, DHA consolidated some of its business functions, such as accounting, from its management offices to DHA headquarters, according to some DHA officials. However, other DHA officials we spoke with stated they were uncertain whether the total number of functions had decreased due to consolidation since the network structure had been implemented. Additionally, DHA officials told us that DHA’s goals for implementing the network structure were to standardize and consolidate business functions. By studying its business functions to determine which ones it will consolidate and developing an implementation plan to track its progress consolidating these functions, DHA will be better positioned to ensure these functions are structured to manage and support its medical facilities as efficiently and effectively as possible.
DHA Considered Input from Some but Not All Stakeholders in Implementing the Network Structure
DHA Considered Input from Some Stakeholders in Implementing the Network Structure
DHA established the Advancement Team to facilitate implementation of the network structure and to communicate with stakeholders, among others, according to DHA officials. In 2023 and 2024, the Advancement Team conducted three surveys of various stakeholders within DHA, including headquarters officials, management office directors of the market and network structures, and the chiefs of staff of the management offices under the network structure, according to DHA documentation and officials.[70] The goal of these surveys was to obtain input on the implementation of the network structure and to identify outstanding issues, according to DHA officials.
|
Stakeholder Perspectives on the Implementation of DHA’s Network Structure Collected through GAO Interviews We identified the following themes about the implementation of the network structure during our discussions with officials from each of the nine management offices and a nongeneralizable sample of six parent medical facilities. Benefits of the network structure unrealized and unknown. One parent medical facility director stated that it is too soon to realize any benefits and efficiencies because the management offices are in the process of hiring and training personnel. Another parent medical facility director stated they have not experienced any benefits resulting from the network structure and do not anticipate any as the structure continues to mature. Additionally, one management office director stated that quality health care is occurring within the network structure, but that there have not been as many efficiencies as the military departments and Congress had assumed there would be. Challenges in implementing the network structure. A management office director stated that additional analysis to inform the implementation of the network structure would have been helpful, but it sometimes seems as if DHA is “building the plane while flying it.” According to a parent medical facility director, the network structure has increased the number of people to report to and the management office directors are stretched too thin to address issues at the medical facilities in an effective and timely manner. Furthermore, medical facilities that are under a management office director that is affiliated with a different military department can experience challenges in budgeting and staffing, according to another parent medical facility director. Source: GAO interviews with Defense Health Agency (DHA) officials. I GAO‑25‑107432 |
DHA planned to conduct additional surveys at the 9-month point, and again at either the 12- or 15-month point after the start of the implementation of the network structure, according to DHA officials. However, the Advancement Team conducted no more surveys and is no longer active as of April 2024 because it achieved its purpose in implementing the network structure, according to DHA officials. We also spoke with officials from each of the nine management offices and a nongeneralizable sample of six parent medical facilities to obtain their perspectives on the implementation of the network structure (see sidebar).
In addition, the DHA Director met with officials from the military departments to discuss the network structure, solicit their feedback, and make changes in the plan based on that feedback, according to DHA officials. For example, DHA added an additional management office to the network structure following discussions with a surgeon general of one of the military departments, according to these same officials. Moreover, DHA holds regular meetings with officials from the military departments and has a liaison officer assigned to the joint staff and each of the combatant commands to maintain open lines of communication, according to DHA officials. Furthermore, in addition to the surveys DHA conducted, it also has available the following collaborative mechanisms, including groups and councils, to involve key stakeholders as shown in figure 4.
Figure 4: Examples of Surveys and Collaborative Mechanisms DHA Has Available to Involve Key Stakeholders
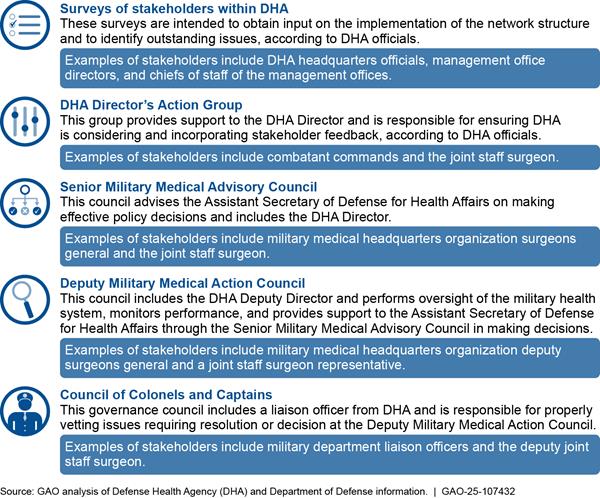
Additionally, DHA engages with Congress through reports, testimonies, and briefings. For example, between 2017 and 2018, DOD provided the Senate and House Armed Services Committees with four reports describing plans to accomplish the transfer of management for the medical facilities from the military departments.[71] In March 2022, the DHA Director testified before the House Armed Services Committee regarding DHA’s organizational reforms to manage its medical facilities.[72] In June 2023, DHA briefed Congress regarding DHA’s intent to make organizational changes to manage medical facilities and its time frame to implement these changes, according to DHA officials. In addition, the DHA Director meets with professional staff of congressional oversight committees and appropriations subcommittees on a monthly and quarterly basis, respectively, according to DHA officials.
Opportunities Exist to Enhance Stakeholder Involvement as DHA Continues to Implement the Network Structure
While DHA has taken steps to involve some stakeholders in the implementation of the network structure, it has not fully leveraged collaborative mechanisms to enhance stakeholder involvement to address concerns. Specifically, we spoke with senior leaders who have key roles in the military health system. These officials described the limited extent of DHA’s engagement with them, other key stakeholders, and Congress. For example:
· Military medical headquarters organization officials. Deputy Surgeons General from each of the three military medical headquarters organizations stated their respective offices, including the Surgeons General, had no formal role in the development of DHA’s network structure. One of the Deputy Surgeons General stated that it would have been beneficial for DHA to obtain buy-in from the military departments prior to implementing the network structure. This same Deputy Surgeon General stated that DHA had not used formal mechanisms to discuss how the organizational structure for managing its medical facilities affects military department missions (e.g., health care outcomes, health care experience, financing, and readiness). If DHA had used these formal mechanisms, it could have increased discussion, the raising of concerns, and buy-in from the military departments, according to the Deputy Surgeon General.
· Joint Staff and Combatant Command Surgeons. Although the joint force is affected by how DHA manages the medical facilities, the Joint Staff did not have a role in the development and implementation of the network structure, according to the Joint Staff Surgeon. Furthermore, both Deputy Command Surgeons we spoke with stated they did not have the opportunity to provide input regarding the development of the network structure. For example, one Combatant Command Deputy Command Surgeon stated that DHA has not solicited feedback in developing new organizational structures, which should consider the operational plans of the combatant commands when making decisions on staffing and resources to minimize adverse effects on their operations.
Additionally, this official stated that DHA needs to maintain two-way communication with the military departments and combatant commands. This communication is needed because operational plans and their resources, such as personnel requirements, are not incorporated enough into DHA’s plans, affecting commands’ abilities to conduct their missions. This official further stated that DHA needs to make sure its focus is not just on health care delivery but also on ensuring the military departments are ready for contingency operations. While DHA has assigned liaison officers to the Joint Staff and combatant commands, the Joint Staff Surgeon and officials from both combatant commands we spoke with stated that DHA has not solicited their input through these liaison officers.
· Congress. Following its briefing to Congress in June 2023, DHA began implementing its proposed changes to the organizational structure—from the market structure to the network structure on October 1, 2023—much faster than previously anticipated, according to DHA officials. These officials stated that as a result, Congress did not have a clear understanding of how implementation efforts were progressing, and DHA should have been more consistent in informing Congress about the accelerated pace of implementation.
DOD Directive 5136.13 directs the DHA Director to give primary consideration to the advice of the Surgeons General of the Army, Navy, and Air Force, as the chief medical advisors on matters pertaining to military health readiness requirements and the force health protection of their respective military service members.[73] Leading agency reform practices we identified in prior work state that agencies should directly and continuously involve their employees, Congress, and other key stakeholders—such as other federal partners with similar customers or that support similar goals—in the development of any major reforms to ensure their views are reflected.[74] Furthermore, these leading agency reform practices state that Congress and the executive branch need the tools and information to help evaluate agencies’ reform proposals and ensure they are effectively implemented.
However, DHA has not fully leveraged collaborative mechanisms to continuously involve all key stakeholders and consider their input as it develops and implements the network structure to manage its medical facilities. Additionally, DHA has not continuously involved Congress in the development and implementation of the network structure to manage its medical facilities and ensure congressional views are reflected. According to DHA officials, DHA’s efforts to implement the network structure are internal efforts within the DHA Director’s authority, and DHA needed to implement the network structure quickly to address the challenges of the market structure. As a result, these officials stated that DHA communicated planned changes with the military departments instead of collaborating with them on the changes. We requested documentation of input DHA had collected from stakeholders who described the limited extent of the agency’s engagement and any plans to continuously involve them. In December 2024, DHA officials stated that such input was collected but had not been documented.
DHA has acknowledged the need to organize and improve processes to include stakeholder engagement. In February 2024, DHA proposed the establishment of an office to encourage a culture of continuous improvement in support of its organizational reform efforts. As of October 2024, DHA officials stated their proposal is evolving as they continue with these reform efforts. Additionally, in November 2024, DHA officials stated that they hold regular meetings with management office directors and staff to obtain input and monitor and manage the performance of the management offices.
Given the importance of ensuring a successful organizational structure for managing the medical facilities and the role they play in providing health care to beneficiaries, it is essential that DHA considers broader stakeholder input going forward to effectively maintain both military health readiness requirements and the force health protection of military service members. By further leveraging collaborative mechanisms to continuously involve all key stakeholders to consider their input on the implementation of the network structure, DHA can enhance these stakeholders’ involvement and better manage fragmented efforts.[75] Additionally, by continuously involving Congress in its organizational reform efforts, DHA will be better positioned to ensure the network structure is meeting the intent of legislative reforms and to create a more efficient oversight structure for the medical facilities that would lower costs and improve beneficiary care.
Conclusions
DHA completed a multiyear, significant reform of the military health system, which started in 2016 when the National Defense Authorization Act for Fiscal Year 2017 required it to assume management of the medical facilities. It has continued to take steps to revise its organizational structure to improve the efficiency and effectiveness of managing the more than 700 facilities it oversees. However, the agency has opportunities to address several long-standing challenges. These include clarifying how its network structure is appropriately organized in line with a statutory requirement, fully determining the personnel resources it requires to manage these facilities via a network structure, consolidating certain business functions, and leveraging all key stakeholders and Congress. Taking action to address these long-standing challenges will help ensure DHA’s network structure can effectively meet military health readiness requirements, force health protection needs of military service members, and the intent of legislative reforms to better serve the military.
Recommendations for Executive Action
We are making the following seven recommendations to DOD:
The Secretary of Defense should ensure that the DHA Director provides information to Congress to clarify how the network structure meets the intent of section 712 of the John S. McCain National Defense Authorization Act for Fiscal Year 2019. (Recommendation 1)
The Secretary of Defense should ensure that the DHA Director issues guidance detailing the processes needed to determine and validate the number of personnel required to manage and support its medical facilities. This guidance should also include processes for conducting workload analyses and address the frequency with which these analyses should be conducted. (Recommendation 2)
The Secretary of Defense should ensure that the DHA Director develops a plan with timelines and key milestones and deliverables to implement its guidance, once issued, to establish personnel requirements and that tracks its progress in determining and validating the number of personnel required, including analyzing workload, to manage and support its medical facilities. (Recommendation 3)
The Secretary of Defense should ensure that the DHA Director studies DHA’s business functions to determine which ones it will consolidate to manage and support its medical facilities. (Recommendation 4)
The Secretary of Defense should ensure that the DHA
Director develops an implementation plan with timelines and key milestones and
deliverables to track its progress consolidating business functions, once
studied, to manage and support its medical facilities.
(Recommendation 5)
The Secretary of Defense should ensure that the DHA
Director further leverages collaborative mechanisms to continuously involve all
key stakeholders and consider their input as DHA develops and implements the
network structure to manage its medical facilities.
(Recommendation 6)
The Secretary of Defense should ensure that the DHA Director continuously involves Congress in DHA’s development and implementation of the network structure to manage its medical facilities and ensure congressional views are reflected. (Recommendation 7)
Agency Comments and Our Evaluation
We provided a draft of this report to DOD for review and comment. In its written comments, reproduced in appendix I and summarized below, DOD concurred with the seven recommendations. DOD provided comments regarding the recommendations and described actions the department has taken or plans to take to address them. It also provided technical comments, which we incorporated as appropriate.
DOD concurred with recommendation 1. In its comments, DOD stated that DHA has frequently briefed Congress on its restructuring plans and that it considers DHA’s restructuring to be complete and implemented consistent and in compliance with the law. While DOD considers the restructuring to be complete and compliant with the statute, providing information to Congress to clarify how the network structure meets the intent of the statute would provide Congress reasonable assurance that DHA is implementing an effective structure that fully integrates the military departments’ medical capabilities and enhances joint military medical operations. We will continue to monitor the extent to which DHA’s actions have met the intent of the recommendation as part of our regular recommendation follow-up process.
DOD also concurred with recommendations 2 and 3, which state that DHA should issue guidance detailing the process needed to determine and validate the number of personnel required to manage and support its medical facilities and develop timelines for implementing this guidance. In its written comments, DOD stated that DHA’s restructuring is complete, and that any future work will continue to include guidance informed by requirements, workload, and appropriate timelines and milestones to ensure the continued, successful management and oversight of medical facilities. Fully implementing these recommendations will help ensure that DHA has the information it needs to establish personnel requirements to effectively accomplish mission and performance objectives. Further, we also discussed in this report the long-standing challenges associated with DHA’s efforts to validate the number of personnel required to manage and support its medical facilities that continue to persist. For example, DHA relies on guidance that does not include a detailed process for determining and validating personnel requirements, including analyzing workload. If the recommendations are implemented effectively, these actions should address the issues described in this report regarding DHA’s lack of necessary information to establish personnel requirements to accomplish its objectives and track its progress.
DOD concurred with recommendations 4 and 5 and stated that DHA has consolidated business functions and will continue to identify, review, and assess opportunities for additional efficiencies in consolidating business functions. We agree that DOD has started and completed the consolidation of some business functions. While this is a first step, DHA officials told us that DHA’s goals for implementing the network structure were to standardize and consolidate business functions. Studying its business functions to determine which ones it will consolidate and developing an implementation plan to track its progress in doing so will better position DHA to ensure these functions are structured to manage and support its medical facilities as efficiently and effectively as possible.
DOD concurred with recommendations 6 and 7 and stated that DHA has established routine engagements with external stakeholders, including through regular meetings. We recognize these aspects of DHA’s efforts to engage stakeholders and Congress. However, we disagree that current practices ensure that DHA is fully leveraging collaborative mechanisms to continuously involve all key stakeholders and Congress in its organizational reform efforts. For example, as we discuss earlier in this report, DHA did not consistently use formal mechanisms to discuss how the organizational structure for managing its medical facilities affects military department missions. In addition, DHA did not consistently inform Congress about the accelerated pace of implementing its network structure. Thus, further leveraging collaborative mechanisms to continuously involve all key stakeholders and consider their input, and continuously involving Congress, would better position DHA to ensure the network structure effectively meets military health readiness requirements, the force health protection needs of military service members, and the intent of legislative reforms to better serve the military.
We are sending copies of this report to the appropriate congressional committees; the Secretary of Defense; the official performing the duties of the Under Secretary of Defense for Personnel and Readiness; the Acting Assistant Secretary of Defense for Health Affairs; the Acting Director of DHA; the Secretaries of the Army, the Navy, and the Air Force; and other interested parties. In addition, the report is available at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions concerning this report, please contact me at AgarwalR@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix II.

Rashmi Agarwal
Acting Director, Defense Capabilities and Management
GAO Contact
Rashmi Agarwal, AgarwalR@gao.gov.
Staff Acknowledgments
In addition to the contact named above, key contributors to this report were Lori Atkinson (Assistant Director), Yecenia Camarillo (Analyst in Charge), Christopher Gezon, Alexandra Gonzalez, Steven Lozano, Jeffrey Mayhew, Jean McSween, Lillian Moyano Yob, Susan Murphy, Brian Noyes, Lillian Ofili, Pamela Snedden, Sarah Veale, and Jaya Walker.
Defense Health Care: DOD Should Reevaluate Market Structure for Military Medical Treatment Facility Management. GAO‑23‑105441. Washington, D.C.: August 21, 2023.
Defense Health Care: Improved Monitoring Could Help Ensure Completion of Mandated Reforms. GAO‑23‑105710. Washington, D.C.: June 22, 2023.
Defense Health Care: Additional Information and Monitoring Needed to Better Position DOD for Restructuring Medical Treatment Facilities. GAO‑20‑371. Washington, D.C.: May 29, 2020.
Defense Health Care: Additional Assessments Needed to Better Ensure an Efficient Total Workforce. GAO‑19‑102. Washington, D.C.: November 27, 2018.
Defense Health Care: DOD Should Demonstrate How Its Plan to Transfer the Administration of Military Treatment Facilities Will Improve Efficiency. GAO‑19‑53. Washington, D.C.: October 30, 2018.
Defense Health Reform: Steps Taken to Plan the Transfer of the Administration of the Military Treatment Facilities to the Defense Health Agency, but Work Remains to Finalize the Plan. GAO‑17‑791R. Washington, D.C.: September 29, 2017.
Defense Health Care Reform: Actions Needed to Help Ensure Defense Health Agency Maintains Implementation Progress. GAO‑15‑759. Washington, D.C.: September 10, 2015.
Military Health System: Sustained Senior Leadership Needed to Fully Develop Plans for Achieving Cost Savings. GAO‑14‑396T. Washington, D.C.: February 26, 2014.
Defense Health Care Reform: Additional Implementation Details Would Increase Transparency of DOD’s Plans and Enhance Accountability. GAO‑14‑49. Washington, D.C.: November 6, 2013.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, X, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]Pub. L. No. 114-328, § 702 (2016), codified as amended at 10 U.S.C. § 1073c. The primary purpose of medical facilities is to support the readiness of the military services, according to DOD Instruction 6000.19. Medical facilities deliver health care to service members, service member families, retirees, and other eligible beneficiaries. Delivering this care also provides essential on-the-job training for military medical providers, enhancing their medical readiness. Department of Defense (DOD) Instruction 6000.19, Military Medical Treatment Facility Support of Medical Readiness Skills of Health Care Providers (Feb. 7, 2020).
[2]Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Interim Report – Preliminary Draft (Mar. 31, 2017); Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Second Interim Report (June 30, 2017); Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Preliminary Draft Plan to Implement 1073c of Title 10, United States Code, Interim Report (Mar. 31, 2018); and Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Final Plan to Implement Section 1073c of Title 10, United States Code, Final Report (June 30, 2018). For the purposes of our report, we refer to these four reports as “DOD’s four reports to Congress containing plans to accomplish the transfer of management for the medical facilities.”
[3]See GAO, Defense Health Care: DOD Should Reevaluate Market Structure for Military Medical Treatment Facility Management, GAO‑23‑105441 (Washington, D.C.: Aug. 21, 2023). The total number of 736 medical facilities reflects DOD’s most current figure, as reported in its annual TRICARE report in fiscal year 2023. Department of Defense (DOD), Evaluation of the TRICARE Program: Fiscal Year 2024 Report: Access, Cost, and Quality Data through Fiscal Year 2023 (Feb. 29, 2024).
[4]For the purposes of this report, a management office is an intermediary management organization that supports medical facilities through management and execution and directly reports to DHA headquarters.
[5]Pub. L. No. 118-31, § 714 (2023).
[6]The Office of the Joint Staff Surgeon coordinates health service support and force health protection capabilities for the joint force. Joint Chiefs of Staff, Joint Pub. 4-0, Joint Logistics (July 20, 2023). Each military department maintains one or more medical headquarters organizations, which are responsible for developing and maintaining the readiness of medical personnel. These include the U.S. Army Medical Command, the Navy Bureau of Medicine and Surgery, and the Air Force Medical Command. Army Medical Command (MEDCOM) Regulation 350-4, MEDCOM Training and Leader Development (June 16, 2010); Office of the Chief of Naval Operations (OPNAV) Instruction 5450.215F, Mission, Functions and Tasks of Bureau of Medicine and Surgery (Oct. 23, 2023); Air Force Medical Service, “Air Force Medical Command” (Falls Church, VA), accessed on December 5, 2024, https://www.airforcemedicine.af.mil/AFMEDCOM/; and Air Force Medical Service, “CSAF signs AFMEDCOM PAD, aligns with key readiness priorities” (Falls Church, VA: June 13, 2024), accessed on December 4, 2024. https://www.airforcemedicine.af.mil/News/Display/Article/3804331/csaf-signs-afmedcom-pad-aligns-with-key-readiness-priorities/. Air Force Medical Command was established on August 15, 2024, according to Air Force officials, and achieved its initial operational capability on March 12, 2025. Air Force, “Air Force Medical Command reaches initial operating capability” (Falls Church, VA: March 13, 2025), accessed on March 27, 2025. https://www.af.mil/News/Article-Display/Article/4119515/air-force-medical-command-reaches-initial-operating-capability/.
[7]For the purposes of this report, a medical facility that is identified as a parent medical facility is typically a large facility, such as a community hospital, with surrounding clinics referred to as child medical facilities, such as behavioral health clinics. The parent designation of a medical facility is based on the Parent Defense Medical Information System Identifier. The child designation of a medical facility is based on the Child Defense Medical Information System Identifier. Defense Health Agency Procedural Instruction 6010.03, Defense Medical Information System Identifier Management Procedures (Dec. 9, 2021). Of the 736 medical facilities reported in fiscal year 2023, 131 of them are designated as parent medical facilities, according to DHA officials. DHA’s management offices directly manage the parent medical facilities, and the parent medical facilities manage the child medical facilities.
[8]A combatant command is a unified or specified command with a broad continuing mission under a single commander established and so designated by the President, through the Secretary of Defense and with the advice and assistance of the Chairman of the Joint Chiefs of Staff. Joint Chiefs of Staff, Joint Pub. 1-0, Volume 2, The Joint Force (June 19, 2020). There are 11 combatant commands. The seven combatant commands that manage military operations in designated geographic areas of responsibility are U.S. Africa Command, U.S. Central Command, U.S. European Command, U.S. Northern Command, U.S. Indo-Pacific Command, U.S. Southern Command, and U.S. Space Command. The four combatant commands that have specific responsibilities or assist in coordinating operations and generally do so globally are U.S. Cyber Command, U.S. Special Operations Command, U.S. Strategic Command, and U.S. Transportation Command. See U.S. Central Command, “Unified Commands, CENTCOM & Components” (Tampa, FL), accessed December 4, 2024. https://www.centcom.mil/ABOUT-US/COMPONENT-COMMANDS/. We selected U.S. European Command and U.S. Indo-Pacific Command because these two combatant commands coincide with the two DHA management offices—Europe and Indo-Pacific—that are not located in the contiguous United States.
[9]Specifically, we reviewed DOD’s four reports to Congress containing plans to accomplish the transfer of management for the medical facilities; Defense Health Agency (DHA), Plan 3: Implementation Plan for the Complete Transition of Military Medical Treatment Facilities to the Defense Health Agency, Version 6.0 (Aug. 12, 2019); Under Secretary of Defense for Personnel and Readiness (USD(P&R)), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022); Defense Health Agency (DHA), Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022); Defense Health Agency (DHA) Memorandum, Defense Health Agency Director’s Initial 90 Day Assessment (Apr. 6, 2023); section 702 of the National Defense Authorization Act for Fiscal Year 2017, Pub. L. No. 114-328, § 702 (2016), codified as amended at 10 U.S.C. § 1073c; H.R. Rep. No. 115-404, at 849-50 (2017) (Conf. Rep.); section 714 of the National Defense Authorization Act for Fiscal Year 2024, Pub. L. No. 118-31, § 714 (2023); and GAO‑23‑105441.
[10]USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022); DHA, Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022); DHA Memorandum, Defense Health Agency Director’s Initial 90 Day Assessment (Apr. 6, 2023); Pub. L. No. 115-232, § 712 (2018), as amended by Pub. L. No. 116-92, § 712 (2019) and Pub. L. No. 118-31, § 714(c) (2023); GAO‑23‑105441; and GAO, Defense Health Care: DOD Should Demonstrate How Its Plan to Transfer the Administration of Military Treatment Facilities Will Improve Efficiency, GAO-19-53 (Washington, D.C.: Oct. 30, 2018). A list of other related GAO products is included at the end of this report.
[11]Pub. L. No. 115-232, § 712 (2018), as amended by Pub. L. No. 116-92, § 712 (2019) and Pub. L. No. 118-31, § 714(c) (2023). Throughout this report, we refer to this as “section 712.”
[12]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: September 2014).
[13]Department of Defense (DOD) Directive 5136.13, Defense Health Agency (Sept. 30, 2013) (incorporating change 2, effective Sept. 12, 2023).
[14]Department of Defense (DOD) Directive 1100.4, Guidance for Manpower Management (Feb. 12, 2005).
[15]Defense Health Agency (DHA), Defense Health Agency Strategic Plan Fiscal Year 2023-2028 (July 31, 2023); GAO, Government Reorganization: Key Questions to Assess Agency Reform Efforts, GAO‑18‑427 (Washington, D.C.: June 13, 2018); and DOD Directive 5136.13.
[16]Defense Health Agency, Market Director IOC Manning Feedback (June 29, 2023); Defense Health Agency, DHN Functional Validation Feedback (Mar. 13, 2024); Office of the Assistant Secretary of Defense for Health Affairs, Military Health System Governance: Senior Military Medical Advisory Council Charter (Jan. 12, 2021); Office of the Assistant Secretary of Defense for Health Affairs, Military Health System Governance: Deputy Military Medical Action Council Charter (Jan. 12, 2021); Office of the Assistant Secretary of Defense for Health Affairs, Military Health System Governance: Council of Colonels and Captains Charter (Dec. 7, 2020); Office of the Assistant Secretary of Defense for Health Affairs, Military Health System Governance Office, Military Health System Governance Business Rules (Mar. 24, 2023); Office of the Under Secretary of Defense for Personnel and Readiness, DHA Network-MTF Alignment (August 2023); Lieutenant General Ronald Place, Director, Defense Health Agency, Patient Safety and Quality of Care, testimony before the House Armed Services Committee, Military Personnel Subcommittee, 117th Cong., 2nd sess., March 30, 2022; DOD’s four reports to Congress containing plans to accomplish the transfer of management for the medical facilities; and DHA, Plan 3: Implementation Plan for the Complete Transition of Military Medical Treatment Facilities to the Defense Health Agency, Version 6.0 (Aug. 12, 2019).
[17]DOD Directive 5136.13.
[19]Department of Defense Directive 5124.02, Under Secretary of Defense for Personnel and Readiness (USD(P&R)) (June 23, 2008) (incorporating change 1, Dec. 11, 2024).
[20]Department of Defense (DOD) Directive 5136.01, Assistant Secretary of Defense for Health Affairs (ASD(HA)) (Sept. 30, 2013) (incorporating change 1, effective Aug. 10, 2017).
[21]The DOD unified medical program budget consists of the Defense Health Program appropriation request, military personnel costs, military construction costs, and the estimated payments to the DOD Medicare-Eligible Retiree Health Care Fund. The Defense Health Program budget makes up the largest portion of the unified medical program budget, accounting for $40.3 billion of the $61.4 billion fiscal year 2025 budget request. Office of the Under Secretary of Defense (Comptroller)/Chief Financial Officer, Defense Budget Overview, United States Department of Defense Fiscal Year 2025 Budget Request (March 2024, Revised Apr. 4, 2024).
[22]In the Army, Air Force, and Marine Corps, the General Officer ranks serve above the rank of Colonel and include the following: Brigadier General (one star); Major General (two stars); Lieutenant General (three stars); and General (four stars). In the Navy, the equivalent ranks, called Flag Officers, serve above the rank of Captain and include the following: Rear Admiral Lower Half (one star); Rear Admiral Upper Half (two stars); Vice Admiral (three stars); and Admiral (four stars). See DOD, “U.S. Military Rank Insignia” (Washington, D.C.), accessed November 6, 2024, https://www.defense.gov/Resources/Insignia/.
[23]DOD Directive 5136.13. The Director of DHA is also responsible for the TRICARE Health Program.
[24]10 U.S.C. § 1073c(a)(1). Initially, the transfer of responsibilities to DHA was to occur by October 1, 2018. However, in August 2018, Congress amended 10 U.S.C. § 1073c to require this transition to occur by September 30, 2021. Pub. L. No. 115-232, § 711 (2018).
[25]10 U.S.C. § 1073c(d). The Joint Staff Surgeon serves as the senior medical advisor to the Chairman of the Joint Chiefs of Staff and coordinates all issues related to joint force military health services. See Joint Chiefs of Staff, “Brig. Gen. (Dr.) John R. Andrus, Joint Staff Surgeon” (Washington, D.C.), accessed December 4, 2024, https://www.jcs.mil/Leadership/Article-View/Article/1981148/brig-gen-dr-john-r-andrus/#:~:text=(Dr.)-,John%20R.,Joint%20Staff%2C%20and%20Combatant%20Commanders. DHA is designated a combat support agency in accordance with section 193 of title 10, United States Code and Department of Defense Directive 3000.06, Combat Support Agencies (CSAs) (June 27, 2013) (incorporating change 1, effective July 8, 2016). This designation applies to the portion of the DHA mission involving support for operating forces engaged in planning for, or conducting, military operations, including support during conflict or in the conduct of other military activities related to countering threats to U.S. national security. Therefore, this portion of the DHA mission is focused on providing support to DOD organizations at the combatant command level and below. DOD Directive 5136.01.
[26]Secretary of Defense Memorandum, Guidance on Military Medical Health System Reform (Nov. 9, 2020); 10 U.S.C. § 1073c(d)(2); see also § 1073c(a)(2)(D) & (E).
[27]DOD Directive 5136.01; and DOD Directive 5136.13.
[28]DOD Directive 5136.13; and 10 U.S.C. §§ 7013(c)(4), 8013(c)(4), 9013(c)(4). A combatant commander is defined as a commander of one of the unified or specified combatant commands established by the President. Joint Chiefs of Staff, Joint Pub. 3-0, Joint Campaigns and Operations (June 18, 2022).
[29]MEDCOM Regulation 350-4; OPNAV Instruction 5450.215F; Air Force Medical Service, “Air Force Medical Command” (Falls Church, VA), accessed on December 5, 2024, https://www.airforcemedicine.af.mil/AFMEDCOM/; and Air Force Medical Service, “CSAF signs AFMEDCOM PAD, aligns with key readiness priorities” (Falls Church, VA: June 13, 2024), accessed on December 4, 2024, https://www.airforcemedicine.af.mil/News/Display/Article/3804331/csaf-signs-afmedcom-pad-aligns-with-key-readiness-priorities/. These military medical headquarters organizations are comprised of medical organizations, such as U.S. Army Medical Readiness Command, Pacific; Naval Medical Forces Pacific; and Air Force Medical Readiness Command Alpha. For the purposes of this report, we refer to these organizations as military medical organizations.
[30]DHA is established as a defense agency in accordance with sections 191 and 192 of title 10, United States Code. Defense agencies, such as DHA, along with the Office of the Secretary of Defense, the Office of the Chairman of the Joint Chiefs of Staff and the Joint Staff, the DOD field activities, and all other organizational entities in DOD that are not in the military departments or the combatant commands are sometimes referred to collectively as the “DOD Fourth Estate.” Department of Defense Instruction 1402.03, Volume 3, Senior Executive Service (SES), Senior Level (SL), and Scientific and Professional (ST) Personnel Categories in the DOD Fourth Estate: Staffing, Reassignments, Transfers, Details, and Reinstatements (Apr. 30, 2014) (incorporating change 2, May 17, 2022).
[31]In November 2013, shortly after DHA was established, we reported that a shared services concept is a combination of common services performed across the medical community, according to DOD officials. DOD identified 10 shared services it planned to implement. For additional details, see GAO, Defense Health Care Reform: Additional Implementation Details Would Increase Transparency of DOD’s Plans and Enhance Accountability, GAO‑14‑49 (Washington, D.C.: Nov. 6, 2013).
[32]10 U.S.C. § 1073c(a)(1). Initially, the transfer of responsibilities to DHA was to occur by October 1, 2018. However, in August 2018, Congress amended 10 U.S.C. § 1073c to require this transition to occur by September 30, 2021. Pub. L. No. 115-232, § 711 (2018). Specifically, the Director of DHA is responsible for budgetary matters, information technology, health care administration and management, administrative policy and procedure, and military medical construction, among other things. The DHA Director also assists the directors of management offices, who have the authority to direct the adoption of common clinical and business functions for their respective management office. DOD Directive 5136.13. For the purposes of this report, we will refer to these processes and functions as clinical or business functions.
[33]Pub. L. No. 115-232, § 711 (2018).
[34]DOD, Evaluation of the TRICARE Program: Fiscal Year 2024 Report: Access, Cost, and Quality Data through Fiscal Year 2023 (Feb. 29, 2024).
[35]Of the 736 medical facilities reported in fiscal year 2023, 131 of them are designated as parent medical facilities, according to DHA officials.
[36]DOD Instruction 6000.19.
[37]Wartime medical skills are those specific abilities required by medical personnel that are essential to the success of the medical mission during deployed operations. DOD Instruction 6000.19.
[38]According to a DOD report, medical facilities serve as training and readiness platforms in two respects. First, 22 medical facilities host graduate medical and dental education programs for physicians and dentists, along with other training and education programs for medical providers. Second, day-to-day patient care at medical facilities helps maintain the clinical skills and readiness of medical providers. Under Secretary of Defense for Personnel and Readiness, Section 749 of the National Defense Authorization Act for Fiscal Year 2017 (Public Law 114-328): Report on Oversight of Graduate Medical Education Programs of Military Departments (July 13, 2018).
[39]Data on personnel requirements, authorizations, and staffing for the management offices within each organizational structure do not exist or are incomplete, according to DHA officials. See also GAO‑23‑105441. As a result, these characteristics cannot be compared. We discuss the status of DHA’s efforts to determine and validate personnel requirements for the management of its medical facilities through its network structure later in this report.
[40]For the purposes of this report, we use the term “staffing” to mean assigning personnel to fill a vacant position.
[41]DHA estimated it needed over 1,400 personnel across its management offices; we reported that this estimate may have been higher than what was needed to support the offices’ workloads and exceeded expected budgetary and personnel resources. GAO‑23‑105441.
[42]USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022); DHA, Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022); and DHA Memorandum, Defense Health Agency Director’s Initial 90 Day Assessment (Apr. 6, 2023).
[43]USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022); and DHA Memorandum, Defense Health Agency Director’s Initial 90 Day Assessment (Apr. 6, 2023).
[44]DHA conducted a study of its headquarters organizational structure to, among other things, assess its effectiveness to execute assigned functions and provide feedback. The study recommended replacing the market structure and provided three options based on, among other things, capabilities and capacity; number of management offices and medical facilities; and existing support constructs within DHA. DHA, Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022).
[45]DHA, Final Report of the Defense Health Agency Headquarters Assessment Team (Dec. 23, 2022).
[46]The Office of the Under Secretary of Defense for Personnel and Readiness completed a study of personnel resources of the military medical headquarters organizations and DHA headquarters. Regarding the market structure being resource intensive, the study identified an estimated shortfall of 513 personnel across DHA headquarters and the market structure relative to the 9,169 required personnel the study estimated. To address this personnel shortfall, the study recommended that DHA resource it internally. USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022).
[47]Section 714 of the National Defense Authorization Act for Fiscal Year 2024, enacted in December 2023, includes a provision prohibiting DOD from advancing beyond phase one of DHA’s plan to establish the network structure until GAO assesses and reports on DHA’s transition efforts. Pub. L. No. 118-31, § 714 (2023). According to DHA officials, DHA has not taken the necessary steps to reach full operating capability for its network structure as a result of section 714. Specifically, a DHA official told us that these steps include restructuring headquarters and transferring personnel and financial systems.
[48]The Indo-Pacific, Pacific Rim, and Central management offices have medical facilities in the Indo-Pacific region, according to DHA documentation we reviewed. The directors of these three management offices share personnel resources, according to a DHA official.
[49]The Defense Health Support Activity office is intended to streamline communications, integrate functional support, track actions through completion, and provide a clear interface with DHA headquarters. DHA, Defense Health Network (DHN) Concept of Operations, Version 4.0 (July 26, 2024). When DHA began to implement the network structure, it initially planned to establish four Defense Health Support Activity offices as part of a phased approach. Specifically, DHA established one Defense Health Support Activity office on October 1, 2023, and planned to establish three additional offices to support its management offices as the network structure continued to mature. DHA later determined it did not need to establish the additional three Defense Health Support Activity offices because one office provided sufficient support for all the management offices, according to DHA officials.
[51]Pub. L. No. 115-232, § 712 (2018), as amended by Pub. L. No. 116-92, § 712 (2019); and Pub. L. No. 118-31, § 714(c) (2023).
[52]USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022) and DHA Memorandum, Defense Health Agency Director’s Initial 90 Day Assessment (Apr. 6, 2023).
[53]Pub. L. No. 115-232, § 712(b)(2) (2018), as amended by Pub. L. No. 116-92, § 712 (2019); and Pub. L. No. 118-31, § 714(c) (2023).
[55]For the purposes of this report, we refer to full-time equivalents as positions. According to DHA guidance, a full-time equivalent is a unit or measure that indicates the workload of an employed person in a way that makes workloads comparable across various contexts. For example, a full-time equivalent of 1.0 is equivalent to a full-time worker, while a full-time equivalent of 0.5 signals half of a full-time worker. Defense Health Agency (DHA) Procedural Instruction 1100.01, Guidance for Manpower Program (May 16, 2019).
[56]The patient experience function includes providing policy, training, and oversight of customer service and the patient experience. The legal function includes providing support for the management office and its subordinate medical facilities in areas such as ethics, labor and employment law, and litigation. The budget function includes managing, allocating, and executing the budget and management of resources for the management office. DHA, Defense Health Network (DHN) Concept of Operations, Version 4.0 (July 26, 2024).
[57]Defense Health Agency, Defense Health Support Activity (DHSA) 60 – Day Assessment: ADHCA Brief (Dec. 14, 2023) and Defense Health Support Activity (DHSA) 90 – Day Assessment: ADHCA Brief (Jan. 24, 2024).
[58]DHA guidance describes validation as a process to justify that the dedication of resources does not duplicate an existing requirement and has not been previously satisfied. DHA Procedural Instruction 1100.01.
[59]DOD Directive 1100.4.
[60]USD(P&R), Zero-Based Review of Medical Headquarters Manpower Requirements (August 2022).
[61]DOD’s Fourth Estate is comprised of defense agencies, such as DHA, along with the Office of the Secretary of Defense, the Office of the Chairman of the Joint Chiefs of Staff and the Joint Staff, the DOD field activities, and all other organizational entities in DOD that are not in the military departments, or the combatant commands. Department of Defense Instruction 1402.03, Volume 3, Senior Executive Service (SES), Senior Level (SL), and Scientific and Professional (ST) Personnel Categories in the DOD Fourth Estate: Executive Resources Management (Apr. 30, 2014) (incorporating change 2, May 17, 2022).
[62]Army guidance states that the measurement and determination of workload will consist of quantitative processes including, personnel studies, modeling, and comparative analyses. Army Regulation 570-4, Manpower Management (May 1, 2024). Similarly, Navy guidance states that personnel requirements should be based on valid, approved workload and determined using analytical methods including operational evaluations, functionality assessments, and better business practices. Office of the Chief of Naval Operations Instruction 1000.16L, Navy Total Force Manpower Policies and Procedures (June 24, 2015) (change transmittal 3, July 2, 2021). Furthermore, Air Force guidance describes different types of studies to determine personnel requirements, including the Logistics Component Model, Manpower Assessment, and Air Force Mission Model. Air Force Manual 38-102, Manpower and Organization Standard Work Processes and Procedures (July 5, 2024).
[63]Defense Health Agency, DHA Strategic Plan 0001.01: Manpower and Resourcing Strategic Plan (Jan. 1, 2024).
[64]DHA, Defense Health Agency Strategic Plan Fiscal Year 2023-2028 (July 31, 2023).
[67]Specifically, these officials stated that the health informatics function reviews whether the Military Health System GENESIS can appropriately document health care delivery and ensure these data are integrated across the medical facilities. Military Health System GENESIS is a modernized electronic health record system that integrates inpatient and outpatient medical and dental information. Department of Defense, Department of Defense MHS Genesis: DOD Healthcare Management System Modernization MHS GENESIS (July 2019).
[68]DOD Directive 5136.13.
[70]In June 2023, DHA surveyed management office directors of the market structure regarding the realignment of medical facilities under fewer management offices and the staffing levels needed at these offices. In January 2024, DHA surveyed headquarters officials and the management office directors to solicit feedback regarding implementation of the network structure, including where certain functions should be managed, according to DHA officials. In March 2024, DHA surveyed the chiefs of staff of the management offices under the network structure to determine whether functions were appropriately assigned to DHA headquarters, the Defense Health Support Activity office, and the management offices. Chiefs of staff of the management offices manage and administer office staff on behalf of the directors of management offices and oversee operations and performance, among other responsibilities. DHA, Defense Health Network (DHN) Concept of Operations, Version 4.0 (July 26, 2024).
[71]Department of Defense, Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Interim Report – Preliminary Draft (Mar. 31, 2017); Report to the Armed Services Committees of the Senate and House of Representatives, Plan to Implement Section 1073c of Title 10, United States Code, Second Interim Report (June 30, 2017); Report to the Armed Services Committees of the Senate and House of Representatives, Preliminary Draft Plan to Implement 1073c of Title 10, United States Code, Interim Report (Mar. 31, 2018); and Report to the Armed Services Committees of the Senate and House of Representatives, Final Plan to Implement Section 1073c of Title 10, United States Code, Final Report (June 30, 2018).
[72]Lieutenant General Ronald Place, Director, Defense Health Agency, Patient Safety and Quality of Care, testimony before the House Armed Services Committee, Military Personnel Subcommittee, 117th Cong., 2nd sess., March 30, 2022.
[73]DOD Directive 5136.13.
[75]GAO, Fragmentation, Overlap, and Duplication: An Evaluation and Management Guide, GAO‑15‑49SP (Washington, D.C.: April 2015).
