VA DISABILITY BENEFITS
Additional Oversight and Information Could Improve Quality of Contracted Exams for Veterans
Report to the Chairman, Committee on Veterans' Affairs, House of Representatives
United States Government Accountability Office
A report to the Chairman, Committee on Veterans’ Affairs, House of Representatives.
For more information, contact: Elizabeth H. Curda at CurdaE@gao.gov.
What GAO Found
The Department of Veterans Affairs (VA) relies on contracted examiners to provide most medical exams for veterans filing disability claims. VA’s Medical Disability Examination Office (MDEO) oversees contracted exams. MDEO uses exam error data to identify quality concerns but miscalculated certain payments intended to incentivize high-quality exams.
Error data. Each quarter, MDEO uses data on contracted exam errors to identify trends and improve exam quality. For instance, MDEO provides contractors with information on the exam types more likely to lead to errors, which contractors use to develop an action plan to prevent these exam errors.
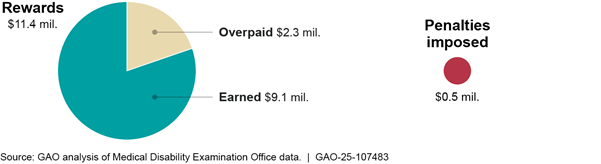
Financial incentives. MDEO also uses its exam error data to calculate financial incentives (rewards and penalties) based on contractor performance. However, it does not have written procedures for verifying the accuracy of these calculations. As a result, MDEO incorrectly paid over $2 million in incentives in the first quarter of fiscal year 2024 (see figure). Until MDEO develops and uses procedures to validate these calculations, it risks wasting funds on incorrect payments.
MDEO uses other key information, such as Special Focused Review findings and stakeholder feedback, to improve exam quality—but its efforts are incomplete.
Special Focused Reviews. MDEO uses Special Focused Reviews to address exam quality issues. However, MDEO has not met its schedule for reviewing exams for complex claims (i.e., traumatic brain injury, military sexual trauma, and Gulf War Illness), which are more likely to result in errors. Reviews for each complex claim type are either overdue--by 9 months as of July 2025--or not yet scheduled, contrary to MDEO procedures that reviews happen every other year. This schedule helps MDEO monitor changes in exam quality and assess the effect of prior recommendations. Completing the reviews as scheduled would improve MDEO’s ability to oversee the quality of these higher-risk exams.
Stakeholder feedback. MDEO collects feedback on exam quality directly from stakeholders, such as veterans and contractor officials, but not from examiners. MDEO relies on contractors to relay examiner feedback, but contractors said they rarely elevate this feedback to MDEO. Further, examiners said there are issues that they would prefer to raise directly to MDEO because of conflicting or unhelpful responses from the contractors. Collecting feedback directly from examiners could improve MDEO’s awareness of potential quality challenges and help improve decisions on disability claims.
Why GAO Did This Study
Disability exams are a critical source of evidence for determining veterans’ eligibility for compensation for service-connected disabilities. In fiscal year 2024, contractors conducted over 3 million disability exams at a cost of over $5 billion, according to MDEO officials.
GAO was asked to review MDEO’s oversight of contracted exams. This report examines the extent to which MDEO uses exam data and other key information to improve exam quality.
GAO reviewed MDEO documents, such as policies and reports, and the most recent MDEO data on financial incentive calculations (April 2023 through September 2024). GAO compared MDEO’s efforts to MDEO procedures, GAO practices for evidence-based decision making, and federal standards for internal control. Additionally, GAO held two discussion groups with claims processors selected for variation in location and duties and grouped by years of experience. GAO also interviewed MDEO officials and six examiners selected for variation in the contractors they worked for, medical specialty, and years of experience.
What GAO Recommends
GAO is making four recommendations, including that MDEO develop and use written procedures for validating financial incentive calculations, complete Special Focused Reviews for complex claims biennially, and identify and use a mechanism to collect and address direct feedback on exam quality from examiners.
VA concurred with three recommendations and concurred in principle with the recommendation on completing Special Focused Reviews. GAO continues to believe this recommendation is warranted, as discussed in the report.
Abbreviations
|
COR |
Contracting Officer’s Representative |
|
DBQ |
Disability Benefits Questionnaire |
|
MDEO |
Medical Disability Examination Office |
|
PACT Act |
Honoring our PACT Act of 2022 |
|
SFR |
Special Focused Review |
|
VA |
Department of Veterans Affairs |
|
VBA |
Veterans Benefits Administration |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
August 18, 2025
The Honorable Mike Bost
Chairman
Committee on Veterans’ Affairs
House of Representatives
Dear Mr. Chairman:
The Department of Veterans Affairs (VA) pays disability compensation to veterans who got injured or sick during their military service in recognition of their sacrifices. To determine veterans’ eligibility, VA’s Veterans Benefits Administration (VBA) often requires disability exams. VBA relies on contractors to provide the medical professionals, called examiners, to conduct most of these exams. In fiscal year 2024, contracted examiners conducted over 3 million disability exams at a cost of over $5 billion, according to VBA officials.
VBA’s Medical Disability Examination Office (MDEO) oversees these contractors, including the quality of the disability exams they provide. Part of MDEO’s stated mission is to ensure that veterans receive high-quality disability exams. Low-quality exams may need to be redone, resulting in delays to veterans’ benefits and higher costs.
You asked us to review MDEO’s oversight of the quality of contracted disability exams. This report examines the extent to which MDEO uses (1) data on contracted exams to identify and address exam errors and (2) other key information to improve contracted exam quality.[1]
To address both objectives, we analyzed VA and VBA documents related to disability exams conducted in the U.S. after a veteran’s discharge from the military. These documents included the performance work statements from the relevant contracts with the four contractors that perform disability exams. These performance work statements specify the contractors’ responsibilities and, according to officials, contractors are required to follow them.[2] In addition, we reviewed related GAO and VA Office of Inspector General audit reports released from 2018 through 2024.[3] We supplemented this information with interviews with VBA officials and relevant stakeholders.
To assess how MDEO uses contracted exam data to identify and address exam errors, we reviewed MDEO documentation including policies, procedures, guidance, plans, and reports. We also analyzed agency data on performance measures for each of the four contractors. MDEO uses these data to calculate financial incentives (rewards and penalties) under each contract.[4] We obtained performance and financial incentive data from the third quarter of fiscal year 2023—when the current methods went into effect—through the fourth quarter of fiscal year 2024. These data were the most current at the time of our review.
We used MDEO’s performance data and parameters to calculate the amount of penalties or rewards that should have been imposed or awarded under each contract and compared our results to MDEO’s results.[5] We compared MDEO’s efforts to calculate financial incentives to MDEO’s goals for the process and to federal internal control standards related to the design of control activities and using quality information.[6] We determined that the performance data were sufficiently reliable for this purpose by analyzing MDEO documents and interviewing officials about their processes for obtaining and validating data. However, we found that MDEO’s calculations of the reward and penalty amounts were not reliable. We describe these limitations in detail later in this report.
To assess how MDEO uses other key sources of information to improve contracted exam quality, we examined MDEO procedures for reviews that are intended to assess topics related to contracted exam quality. We also reviewed the reports resulting from these quality reviews and interviewed agency officials for further context. We compared MDEO’s efforts to its procedures for completing these quality reviews.
In addition, we examined MDEO’s efforts to collect and address feedback from internal and external stakeholders to improve contracted exam quality. To do so, we obtained documents from and interviewed MDEO officials and contractors. We also interviewed disability claims processors and examiners.[7] Specifically, we:
· Reviewed documentation and interviewed MDEO officials about how they track and respond to stakeholder feedback.
· Interviewed representatives from all four contractors and obtained documents about their processes for conducting exams and obtaining examiner feedback.
· Conducted two group discussions with VBA claims processors. Specifically, we asked MDEO to identify claims processors with representation across a variety of VBA regional offices, responsibilities, and years of experience. Ultimately, we held one group discussion with nine claims processors who had 5 or more years of experience and another with 10 claims processors who had fewer than 3 years of experience. Two of the claims processors in each group served as exam liaisons, a role in which they are responsible for sharing information between claims processors in their regional offices and MDEO. Information obtained from these group discussions cannot be generalized to all claims processors.
· Interviewed six examiners who perform VBA contracted exams. Using a randomized list of all examiners, we selected eight examiners for variation in characteristics such as the contractors they worked for, geography, specialty, and years of experience. We interviewed six of the eight selected examiners: an audiologist, nurse practitioner, general practitioner, family medicine practitioner, dentist, and optometrist.[8] Findings from examiner interviews are not generalizable, but provide perspectives and illustrative examples related to VBA’s oversight of contracted exams.
We assessed MDEO’s efforts to collect and address stakeholder feedback against relevant key practices for evidence-based decision-making.[9]
We conducted this performance audit from March 2024 to August 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
VBA pays disability compensation to veterans with service-connected disabilities based on the severity of the disability. The VBA disability claims process starts when a veteran submits a claim to VBA. VBA claims processors help the veteran gather information to support their claim and, if necessary, may request a disability exam for the veteran. During an exam, the examiner fills out a Disability Benefits Questionnaire (DBQ) for each disability under evaluation to document the veteran’s condition. According to the agency, DBQs are designed to collect the medical evidence that claims processors need to adjudicate a claim and rate the severity of a specific disability.
According to VBA officials, in fiscal year 2024 contractors performed approximately 3.2 million exams—representing 93 percent of all disability exams—compared with 1.8 million exams in fiscal year 2022. The volume of exams performed by contractors has increased significantly following the enactment of the Honoring Our PACT Act of 2022 (PACT Act).[10]
VBA established MDEO in 2016 to oversee contractors and ensure exam quality. MDEO leads VBA’s oversight efforts by managing contractors, creating and updating DBQs, and analyzing available exam data to assess exam quality and contractor performance.[11] VBA has refined MDEO’s oversight of contractors and implemented new oversight mechanisms in response to recommendations from GAO and the VA Office of Inspector General (see table 1).
Table 1: Examples of Veterans Benefits Administration (VBA) Actions in Response to Prior GAO and Veterans Affairs Office of Inspector General Recommendations Related to Exam Quality
|
Report |
Recommendation |
VBA actions in response to recommendations |
|
Oct. 12, 2018a |
VBA should regularly monitor and assess aggregate performance data and trends over time. Status: closed—implemented |
In October 2020, VBA established a new data analytics team within its Medical Disability Examination Office (MDEO) to assess contractor performance data and allow VBA to monitor trends at both the contractor and program level. |
|
Mar. 23, 2021b |
VBA should develop a process to assess the quality of exam reports for complex claims completed by contractors. Status: closed—implemented |
In November 2021, MDEO completed its first review under the new process, which focused on a category of complex claims. MDEO completed reviews for the other two types of complex claims in August 2022 and September 2023. |
|
VAOIG-21-01237-127 June 8, 2022c |
VBA should assess and modify contracts to ensure that contractors can be held accountable for unsatisfactory performance by applying monetary disincentives. Status: closed |
VBA’s comments in the report said VBA executed new contracts in 2021 that included monetary disincentives (penalties). Additionally, VBA officials told GAO they imposed the first penalties under the new contracts in the third quarter of fiscal year 2022. |
|
|
VBA should require MDEO to analyze all available error data and provide systemic exam issues and error trends to contractors. Status: closed |
MDEO provided GAO with a Performance Work Statement attachment that states contractors will receive a report each quarter that contains systemic exam findings and error trends from two sources. |
Source: GAO analysis of the reports listed above and VBA information. | GAO‑25‑107483
aGAO, VA Disability Exams: Improved Performance Analysis and Training Oversight Needed for Contracted Exams, GAO‑19‑13 (Washington, D.C.: Oct. 12, 2018).
bGAO, VA Disability Exams: Better Planning Needed as Use of Contracted Examiners Continues to Grow, GAO‑21‑444T (Washington, D.C.: Mar. 23, 2021).
cVeterans Affairs Office of Inspector General, Contract Medical Exam Program Limitations Put Veterans at Risk for Inaccurate Claims Decisions, VAOIG-21-01237-127 (Washington, D.C.: June 8, 2022).
VA faces long-standing challenges managing large volumes of disability compensation claims and making timely decisions. As a result, VA’s management of disability claims workloads has been on GAO’s High-Risk List since 2003.[12]
MDEO Uses Exam Data to Address Errors but Miscalculated Certain Financial Incentives
MDEO Uses Data from the Disability Claims Process and an Internal Checklist to Identify and Address Errors
Quality Action Plans
Each quarter, MDEO gathers data on exam errors and creates a report for each contractor identifying quality trends. The report identifies (1) the types of DBQs that claims processors reviewing the exams identified as being incomplete or unclear, and (2) the DBQs that VBA’s quality assurance processes later found to be insufficient.[13] For example, MDEO’s quarterly report for one contractor reviewed error data from the third quarter of fiscal year 2024 and identified the knee and lower leg DBQ as the type that was most often incomplete or unclear.
According to the performance work statement, contractors are required to submit a quality action plan within 45 days of receiving the quarterly report. The action plan should analyze the cause of the error trends and document the contractor’s efforts to address the report’s findings. For instance, in the example above, the contractor would identify corrective actions to improve the quality of DBQs related to the knee and lower leg exams. MDEO Senior Quality Analysts then review each contractor’s action plan and compile the findings into a summary report.
In September 2024, we found that MDEO’s procedures for its action plan review did not provide clear and complete steps to guide this process.[14] MDEO had developed written procedures for reviewing these action plans in response to our preliminary findings. However, we found that these procedures had gaps. As a result, we recommended that VBA improve the clarity and completeness of its procedures for reviewing contractors’ quality action plans. Specifically, we stated that these procedures should include steps for MDEO to routinely verify that contractors have completed the corrective actions in their quality action plans and determine the extent to which these actions help improve exam quality. VBA generally agreed with the recommendation and has partially addressed it.[15]
DBQ Quality Criteria Checklist
Each quarter, MDEO generates additional data on exam errors by evaluating a sample of completed DBQs from each contractor.[16] MDEO Quality Analysts identify errors in this sample using a 10-question Quality Criteria Checklist (which we refer to as the checklist) to measure whether examiners completed DBQs accurately and completely (see fig. 1).[17]
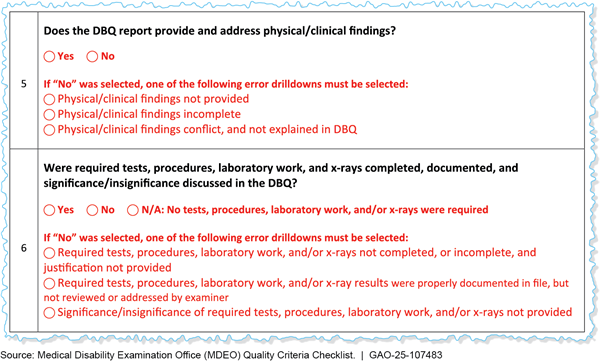
Note: During disability exams, examiners fill out Disability Benefits Questionnaires (DBQ) asking for specific information for each condition.
MDEO makes several efforts to verify the accuracy and completeness of the checklist errors identified by MDEO Quality Analysts, including:
· Providing detailed guidance on applying the checklist for each condition.
· Conducting a second review of each error to check compliance with MDEO guidance, identify trends and outliers, and resolve any items of concern.
· Offering an option for contractors to request error reconsideration. Three MDEO officials determine whether errors were cited correctly according to the contracts.
· Having performance expectations that Quality Analysts should correctly fill out 96 percent of the checklist questions (i.e., identify errors and non-errors) after their first year of employment. To measure this, a Senior Quality Analyst chooses a random sample of each Quality Analyst’s checklist reviews and completes a second checklist for comparison.
MDEO officials told us they analyze the checklist error data each month to identify trends and improve oversight of exam quality.[18] For example, in fiscal year 2024, MDEO identified two checklist questions with the most errors, regardless of the type of condition being evaluated (shown in fig. 1, above). In response, MDEO created two job aids to help examiners prevent these errors. MDEO officials told us that after distributing the job aids, they received positive feedback from contractors and observed a decrease in those specific errors.
MDEO also analyzes the effects of checklist errors on claims, such as delays associated with correcting errors. According to MDEO officials, many claims continue through processing and are decided before MDEO completes its checklist review. After MDEO identifies errors, claims processors determine if the errors affected their decisions on the claims. For example, in the third quarter of fiscal year 2024, MDEO identified around 1,200 errors. Eighty-eight percent of those errors did not affect the claim decision, according to MDEO’s analysis, but 6 percent needed a new exam.[19] According to MDEO documentation, MDEO provides this information to contractors to bring awareness of the impact of errors on the claims process.
Another MDEO analysis found that the DBQ for back conditions had the most errors in the second quarter of fiscal year 2024. Subsequently, MDEO created two microlearning modules about that DBQ. MDEO documents state that MDEO plans to continue to identify error trends and develop microlearning videos to address them.
MDEO Incorrectly Paid More than $2 Million in Financial Incentives in Fiscal Year 2024
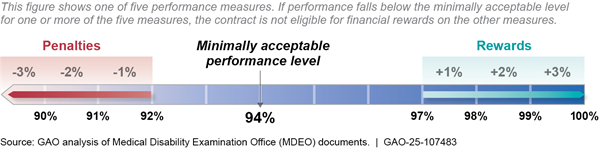
Each quarter, MDEO assigns financial incentives (rewards and penalties) to contractors based on five performance measures:
· Quality: Accuracy rate on the Quality Criteria Checklist (percentage of items reviewed that did not result in an error).
· Customer satisfaction: Percent of surveyed veterans who were satisfied overall with their examination.[20]
· Production: Number of exams completed.
· Average Days to Complete: Average days from accepting exam request until exam completion.
· Average Days Pending: For exams not yet completed, average days since contractor accepted exam request.[21]
Contractors may receive financial incentives when performance falls below or above certain thresholds, according to the performance work statement. For example, for the quality performance measure in fiscal year 2024, MDEO imposed a penalty for accuracy rates below 92 percent and assigned a reward for accuracy rates above 97 percent (see fig. 2). Penalties and rewards increased incrementally beyond these thresholds.
Figure 2: Quality Performance Measure Thresholds for MDEO Contracted Disability Exams, Fiscal Year 2024
According to MDEO officials, contractors’ performance has improved over time. For example, MDEO data showed that in the first quarter of fiscal year 2024, accuracy rates for work under 10 of the 13 contracts were above the reward threshold for the quality performance measure and none were below the penalty threshold.
In fiscal years 2023 and 2024, MDEO used a manual process to calculate financial incentives. According to officials, an MDEO Contracting Officer’s Representative (COR) obtained performance data for the work under each contract from other MDEO offices. Officials added that the COR then manually:
1. entered the data into a spreadsheet;
2. compared the data for each of the five performance measures to the relevant thresholds to determine the penalty or reward earned for that measure (up to +/- 3 percent of quarterly invoices);
3. summed the five percentages to obtain a cumulative positive or negative percentage;[22] and
4. applied the cumulative percentage to the contract’s quarterly invoices to calculate the penalty or reward. For example, if a contract earned a 1 percent reward on each of the five performance measures, its total reward would be 5 percent. If the contract’s total invoices were $1,000,000, the financial incentive payment would be $50,000 for that quarter.
Along with this manual calculation process, MDEO’s process for verifying CORs’ calculations was also manual and informal. Specifically, officials told us that the Chief or Lead Management Analyst conducted a quality check but did not provide more details on what the check entailed. Moreover, MDEO had no written procedures to guide this check or ensure consistent reviews of data entry or calculations. Officials also said that MDEO did not use electronic checks, such as formulas applying the thresholds to the performance data. For the second quarter of fiscal year 2025, MDEO began calculating financial incentives using a different spreadsheet with locked cells and auto calculations, which officials say will help reduce the likelihood of manual miscalculations. The new spreadsheet will not address inaccurate data entry, but MDEO officials told us they are developing another tool for verifying CORs’ calculations.
MDEO’s process for verifying calculations did identify and correct some errors. We examined MDEO’s financial incentive calculations from the third quarter of fiscal year 2023 through the fourth quarter of fiscal year 2024.[23] We identified five instances where CORs entered the wrong percentage for performance measures, but these errors were corrected before the financial incentives were finalized. If not corrected, these errors would have resulted in over $6 million in incorrect payments.
However, our analysis found that MDEO did not detect two other errors, resulting in almost $2.3 million in overpayments (see fig. 3). Specifically, for the first quarter of fiscal year 2024, CORs entered the wrong financial incentive percentages for two contracts. MDEO officials confirmed that these errors resulted in overpayments and said they are taking steps to recoup the funds from the contractors. As of April 2025, MDEO had not yet received the funds.
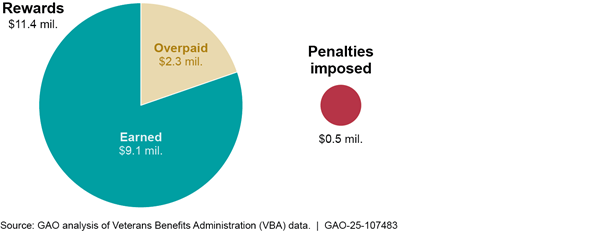
Officials said MDEO did not have procedures to guide the internal quality checks or to establish processes for verifying the accuracy of COR spreadsheets because they believed their review process was a sufficient quality control. They told us they are now creating new tools for calculating and verifying financial incentives but have not developed procedures for correct and consistent use of these tools. However, federal internal control standards call for management to use quality information and design control activities, such as policies and procedures, to achieve objectives.[24] In this case, establishing and following procedures for routine and thorough validation of financial incentive calculations (to include data entry and performance values) could help ensure the accuracy of these calculations and help MDEO prevent future incorrect payments.
Our analysis shows that there is a risk that MDEO could have made other incorrect payments from earlier calculations that we did not review. However, as of April 2025, MDEO officials had not verified all financial incentives calculations paid to contractors since incentives began in fiscal year 2022. Officials told us they were open to doing so but had not begun. The performance work statement says the purpose of financial incentive payments is to encourage contractors to continuously improve, but receiving unearned financial incentives undermines this purpose. By recalculating all the financial incentive calculations made to date, documenting any inaccurate payments found, and correcting any incorrect payments, MDEO can strengthen the effectiveness of its financial incentives and safeguard taxpayer dollars.
MDEO Uses Special Focused Reviews and Feedback from Stakeholders to Improve Exam Quality, but Efforts Are Incomplete
Special Focused Reviews Can Identify and Address Quality Concerns, but MDEO Has Not Met Its Review Schedule
As part of its oversight of exam quality, MDEO conducts Special Focused Reviews (SFRs) to identify and address exam quality trends. MDEO uses SFRs to recommend ways for both internal stakeholders and contractors to improve the exam process.[25] MDEO officials identified three primary types of SFRs related to exam quality: (1) provider SFRs, (2) quality SFRs, and (3) complex claim SFRs.
Provider SFRs.[26] When monthly quality reports or VA leadership identify examiners with potential quality issues, MDEO clinical staff review a selection of the examiner’s DBQs to identify the extent and severity of exam errors. The resulting corrective actions depend on the nature of the errors. In cases where MDEO staff determine that any identified errors are not significant, the examiner receives retraining on relevant material. However, if identified errors are severe, MDEO may suspend the examiner, who can be reinstated after completing retraining and performing up to 10 DBQs that are reviewed by clinical staff.
MDEO officials stated that 441 provider SFRs were completed in fiscal year 2024. Thirteen of these reviews resulted in examiners being suspended, with four of the 13 examiners being reinstated after completing retraining.
Quality SFRs. MDEO’s Quality team can review topics related to exam quality as needed, such as specific types of DBQs or potential issues with exam processes. Reasons for these reviews include requests from VBA leadership, planned reviews of emerging issues, or findings from prior quality reviews. The findings from the quality SFRs can include identified quality trends, a root cause analysis of identified deficiencies, and potential recommendations to address quality concerns.
MDEO officials stated they completed eight quality SFRs across fiscal years 2023 and 2024. One review assessed PACT Act related exams and recommended establishing a monthly process to discuss and address PACT Act exam errors with each contractor. MDEO tracks and documents the completion status of recommendations resulting from each quality SFR.
Complex claim SFRs. MDEO reviews three types of complex claims: (1) traumatic brain injury, (2) mental health claims based on military sexual trauma, and (3) Gulf War Illness. These reviews assess the accuracy of exam requests and the quality of the DBQs completed by contracted examiners. MDEO uses the findings to identify potential improvements to the exam process by developing recommendations to contractors or MDEO staff. For example, a 2023 review for claims involving traumatic brain injury recommended revising part of the exam’s DBQ instructions and updating examiner training.
MDEO began conducting these reviews in response to prior GAO work where we found that examinations for traumatic brain injury, military sexual trauma, and Gulf War Illness are more challenging for examiners to perform.[27] We recommended that VBA develop a process to assess exam quality for these claim types. VBA agreed with the recommendation and, in response, established a process for conducting complex claim SFRs.
Current MDEO procedures state that reviews for each complex claim type are to be completed biennially to monitor changes in exam quality and assess the effects of corrective actions from prior reviews; however, MDEO has not followed this schedule. As of May 2025, MDEO has completed one review for each type of complex claim but has not completed any second reviews. Reviews for two of the complex claim types are currently behind schedule. Further, MDEO officials could not provide an expected start date for the third claim type, which has a review due by the end of fiscal year 2025 (see table 2).
|
Complex claim type |
First review completed |
Second review due |
Status of second review, according to MDEO officials |
|
Military sexual trauma |
November 2021 |
September 2024a |
Expected to be completed in July to September 2025 |
|
Gulf War Illness |
August 2022 |
September 2024 |
Not scheduled |
|
Traumatic brain injury |
September 2023 |
September 2025 |
Not scheduled |
Source: GAO analysis of Medical Disability Examination Office (MDEO) information. | GAO‑25‑107483
aThe procedures for complex claim Special Focused Reviews stipulate that military sexual trauma reviews should be performed biennially in the fourth quarter of even fiscal years. The second military sexual trauma review was scheduled for just under 3 years after the first review (rather than 2 years) because these procedures were implemented in September 2022, after the first military sexual trauma review had already been completed in November 2021.
MDEO officials told us competing priorities and limited resources have contributed to delays in completing the reviews on schedule. For example, the staff involved in complex claim SFRs also develop and modify examiners’ certification courses and assist in completing provider SFRs. Despite these competing priorities, in January 2025 officials told us that they designed the biennial schedule to determine if reviews are improving exam quality and would prefer to maintain this process rather than changing to a longer schedule.
Prioritizing the completion of complex claim SFRs as scheduled would help MDEO officials oversee and improve the quality of these higher-risk exams. For instance, the initial SFRs for each of the three complex claim types included recommendations for MDEO such as updating DBQs, examiner training, or exam request language. However, the second reviews for each claim type are either behind schedule or not yet scheduled. Conducting complex claim SFRs biennially would better position MDEO to determine whether these corrective actions are improving exam quality for these higher-risk exams and whether additional actions are needed.
MDEO Collects Direct Feedback on Exam Quality from Several Stakeholders but Not Examiners
Direct Feedback from Certain Stakeholders
To improve exam quality, MDEO collects direct feedback from internal and external stakeholders through mechanisms such as discussions, surveys, or a dedicated online portal. For example:
· Discussions: Representatives from the four contractors told us they provide feedback through regularly scheduled discussions with MDEO and, as needed, informal discussions. Similarly, VBA claims processors we spoke with said that certain claims processors—who serve as liaisons between claims processors in regional offices and MDEO—can also provide direct feedback through discussions with MDEO.
· Surveys: Typically, veterans can choose to complete a satisfaction survey following exams, and MDEO tracks the survey responses. As previously discussed, MDEO uses these post-exam survey responses when calculating contractors’ financial incentive payments.[28] Additionally, in 2024 MDEO surveyed contractors on MDEO feedback mechanisms; officials told us they also had conducted this survey in 2023.
· Online portal: According to officials, MDEO has an online portal that allows any stakeholder with a VA email address to submit feedback. This includes MDEO components and certain contractor officials who are given access but does not include examiners.[29] MDEO’s Inquiries team is tasked with tracking the feedback. According to officials from this team, they log the information and either address it or forward it to the MDEO component they believe is best positioned to respond.
MDEO officials described different ways they have used feedback to inform decisions related to exam oversight. For example, MDEO leads a DBQ Change Control Group that includes stakeholders from outside of MDEO, such as the Board of Veterans’ Appeals.[30] The DBQ Change Control Group collects and incorporates stakeholders’ feedback to identify, discuss, and approve changes to DBQs.[31] Officials described an instance in which the group incorporated feedback from the MDEO Quality team to split one DBQ question into two parts to improve clarity. Additionally, officials stated that the group meets biweekly and is responsible for approving any changes to DBQs, such as DBQ updates made in response to changes to VA regulations and court decisions.
Officials also said MDEO components met to identify new contract provisions before awarding new contracts in December 2024.[32] They said MDEO components presented ideas based on their expertise and on stakeholder feedback. Participants then discussed the benefits and risks of the different ideas and used this information to determine which ideas should become contract provisions. MDEO officials said they believed this process led to stronger contracts. For example, they said new contract provisions, such as requirements that contractors submit plans for inspecting exam facilities and report the results to MDEO, will improve oversight of exam quality.
Additionally, officials from MDEO’s Inquiries team said
they run reports for other MDEO components upon request. This includes compiling
data on complaints about specific examiners—submitted by veterans or other
stakeholders—to support provider SFRs.
Examiner Feedback
MDEO relies mainly on contractor officials to relay examiner feedback and does not collect feedback directly from examiners on the quality of exams. Representatives from the four contractors told us they use various methods to collect this feedback from examiners, such as dedicated phone lines, email addresses or online portals, and advocates assigned as points of contact with the examiners.
However, five of the six examiners we interviewed said they would prefer to provide direct feedback to MDEO rather than providing it indirectly, via contractors.[33] Examiners we interviewed primarily reported two concerns about delivering feedback via contractors that may prevent their feedback from being addressed: conflicting instructions and unhelpful responses.
Conflicting instructions. Examiners working for more than one contractor may receive different instructions from those contractors. For example, according to an examiner who works for two different contractors, one contractor said blood tests and radiology were required for a particular type of exam and another said they were not. According to the examiner, they raised this concern with the contractors, and both said their respective approaches were correct. The examiner said both the contractors cannot be right and these responses mean that some exams either are missing necessary information or are subjecting the veterans to unnecessary, potentially harmful tests. This examiner said if they could provide feedback directly to MDEO they would ask, “For my understanding, could you help me clarify what is the accepted standard for this particular claim? I’m seeing that contractors do different things. What should I be doing?”
Individual contractors are not positioned to address conflicting instructions an examiner may receive from different contractors. When we asked contractors how they would respond to such a scenario, each described their internal processes. Specifically, representatives from three contractors said they would rely on their quality experts to make the determination or elevate the issue internally by involving staff such as clinical experts. Of these, representatives from two said they would solicit MDEO’s guidance as needed. Representatives from the fourth contractor said it would be the examiner’s responsibility to determine which diagnostic testing was medically appropriate in accordance with the contractual guidelines. These processes do not help examiners determine what measures to take when contractors’ guidance conflicts.
Unhelpful responses: Four examiners told us the contractors they work for were unable to address the examiners’ feedback. One examiner we interviewed said, because past feedback was not addressed, they no longer elevate challenges to their contractor. This examiner told us, “My voice isn’t heard at all. I don’t know where [my feedback] goes. It’s out there in the clouds somewhere.”
Another examiner we interviewed, who has experience working for two contractors, said one of the contractors would list the examiner as the person ordering any additional tests that were needed after an exam. The examiner said they understood state law to require examiners to discuss all test results with patients, but the examiner neither knew the tests were ordered nor had any way to contact the veterans, which was an uncomfortable situation. The examiner told us they raised this concern with the contractor, but contractor officials said they would not make any changes to their processes. By contrast, the examiner said the other contractor they work with relies on its medical director to order all follow-on tests.
We asked representatives from the four contractors what they would do if an examiner raised ethical or legal concerns. Representatives from each contractor described elevating and addressing such concerns internally by working with senior staff such as attorneys, the medical director, or both.
The contractor representatives generally stated that their existing processes for assisting examiners and addressing feedback are sufficient and that they rarely need to relay examiner feedback to MDEO. Specifically, according to their representatives, two contractors do not raise feedback from examiners to MDEO often. Representatives from one of these contractors said it has been a few years since they last provided such feedback. Representatives from the third contractor said it has not yet needed to raise examiner feedback to MDEO. Finally, representatives from the fourth described their process for providing feedback to MDEO, but did not provide any examples of having done so.
All six examiners said unaddressed feedback can make it more difficult to provide quality exams, accurately complete exam paperwork, or both. Additionally, three examiners said they believe unaddressed feedback has contributed to delays in veterans’ disability determinations.
For example, one examiner who works for multiple contractors described challenges providing feedback to the contractors’ quality assurance staff. Specifically, the examiner told us they were required to work with the quality assurance staff, but they believed that the staff sometimes gave bad advice, such as suggesting a wording change to a DBQ that would confuse claims processors. Based on the examiner’s experience—both performing contracted exams and, previously, performing exams for VA—they have told contractors’ quality assurance staff that certain changes were incorrect and would cause delays. According to the examiner, despite this feedback, the staff still required the examiner to make the changes. The examiner added, “They make me do it the way they think is correct and, invariably, it will get kicked back, which is rework for me, rework for them, and a delay for the veteran…[It is] a wall of no communication.”
According to MDEO officials, they rely on contractors for examiner feedback because contractors are responsible for directing examiners’ work, per the contract. Specifically, the officials said contractors are required to employ key clinical personnel who are already collecting examiner feedback and relaying it to MDEO through mechanisms, such as monthly meetings. They also said that the contractors have frequent opportunities to share any concerns they have heard from examiners. According to MDEO officials, these interactions are sufficient for obtaining examiner feedback.
MDEO officials acknowledged they could provide a mechanism (such as an email address) for examiners to give direct feedback on exam quality. However, the officials said they had not considered doing so. Officials from MDEO’s Inquiries team said they could track incoming feedback from examiners, as they do with feedback from other stakeholders. They noted that if this caused the feedback volume to increase, however, the team might require more resources.
MDEO officials also said MDEO can obtain examiner feedback through interviews during site visits. However, according to officials, these visits are primarily focused on compliance with safety and cleanliness standards rather than on exam quality. Moreover, they are generally one-time events that reach a limited number of examiners.[34] Officials said any examiner feedback collected during site visits would either be included in a site visit report or be shared with the appropriate contractor; however, they were unable to provide examples of any changes MDEO made in response to such feedback in the past 2 fiscal years.
Collecting stakeholder feedback has been a key goal of MDEO’s strategic planning efforts.[35] Leading practices for evidence-based decision-making state that successful stakeholder engagement should occur early and often and is not a one-time event. The practices also state that stakeholder engagement should include identifying existing evidence and reviewing the results.[36] By identifying and using a mechanism for collecting and addressing voluntary feedback directly from examiners, who offer a key perspective about examinations, MDEO can improve its ability to identify and address potential challenges with exam quality and to prevent delayed disability determinations.
Conclusions
Disability exams are a critical source of information for determining veterans’ eligibility for benefits. Over the past several years, MDEO has implemented new mechanisms or refined existing ones to improve its oversight of exams performed by contractors, but additional oversight and information would help achieve better results.
Specifically, MDEO uses data on exam errors to inform financial incentive calculations and encourage high-quality contractor performance. However, MDEO manually reviews these calculations and does not have procedures for validating their accuracy, which resulted in over $2 million in incorrect payments in fiscal year 2024. By implementing procedures for validating financial incentive calculations, MDEO can prevent future overpayments. Further, recalculating all financial incentive calculations made to date and correcting any identified mistakes would help MDEO ensure the effectiveness of these incentives to facilitate high-quality exams.
Additionally, MDEO conducts SFRs on certain complex types of exams that are particularly challenging for examiners to perform. However, MDEO has not prioritized completing these reviews on the biennial schedule established in its procedures, limiting its ability to determine whether its prior reviews were effective or if new corrective actions are needed. Completing these SFRs as scheduled would help MDEO monitor and improve the quality of these high-risk exam types.
Finally, MDEO collects feedback directly from certain stakeholders and uses this feedback to inform exam oversight. But because MDEO does not collect feedback on exam quality directly from examiners, the agency is missing a key perspective for identifying quality issues. Collecting voluntary feedback on exam quality directly from examiners would better position MDEO to address exam quality concerns and help veterans receive the benefits they are entitled to without delay.
Recommendations for Executive Action
We are making the following four recommendations to VA:
The Secretary of VA should ensure that MDEO develops and uses written procedures to validate the accuracy of its financial incentive calculations, including data entry and scoring of performance measures. (Recommendation 1)
The Secretary of VA should ensure that MDEO recalculates all financial incentives since 2022 and documents and corrects any inaccurate penalties and payments. (Recommendation 2)
The Secretary of VA should ensure that MDEO conducts Special Focused Reviews of contracted exams for complex claims (traumatic brain injury, military sexual trauma, and Gulf War Illness) on a biennial basis, in accordance with its procedures. (Recommendation 3)
The Secretary of VA should ensure that MDEO identifies and uses a mechanism to collect and address direct feedback from examiners on the quality of exams. (Recommendation 4)
Agency Comments, Third Party Views, and Our Evaluation
We provided a draft of this report to VA for review and comment. VA provided written comments, which are reproduced in appendix I and summarized below. VA concurred with recommendations 1, 2, and 4 and described actions it would take to address them. VA concurred in principle with recommendation 3. VA estimated that its actions to address each of the four recommendations would be completed by September 30, 2025. VA did not provide any technical comments.
Regarding recommendation 3, VA concurred in principle that MDEO should conduct SFRs of exams for complex claims biennially, in accordance with its procedures. VA stated that the referenced procedures allow for some flexibility and include a disclaimer that they can be adapted to the specific needs of a given review. As an example of how its disclaimer might work in practice, VA stated that without the necessary resources, MDEO might not be able to complete these reviews on a biennial basis. VA stated that MDEO will assess its current resources, review the requirements for complex claim SFRs, and revise the procedures if appropriate.
As VA considers changing its procedures, VA should be mindful that it established the biennial schedule because prior GAO work identified that exams for these complex claim types are challenging for examiners to perform. Additionally, MDEO officials told us the biennial schedule is the preferred process for these reviews. While we acknowledge that the procedures allow for some flexibility, we found VA has fallen behind schedule across the board. Specifically, VA is already behind schedule on reviews for two complex claim types and could not provide a completion timeframe for the third claim type. As noted in the report, the purpose of these reviews is to monitor changes in exam quality and assess the effects of corrective actions from prior reviews. We continue to believe our recommendation is valid and that prioritizing the completion of these reviews as scheduled would better position MDEO officials to improve the quality of these higher-risk exams.
We also provided excerpts of the draft report to representatives of each of the four contractors for their review. One contractor provided technical comments, which we incorporated as appropriate, and two contractors did not have any comments. The other contractor suggested that the fourth recommendation focus specifically on examiner feedback related to unclear or conflicting exam guidance or instructions. We agree that such feedback could help resolve conflicting information among contractors. However, as the report details, examiners also raised other concerns, such as contractors not being responsive to examiners’ questions. We did not change the recommendation that MDEO should identify and use a mechanism for examiners to provide direct feedback on exam quality and continue to believe it is valid.
As agreed with your office, unless you publicly announce the contents of this report earlier, we plan no further distribution until 16 days from the report date. At that time, we will send copies to the appropriate congressional committees, the Secretary of Veterans Affairs, and other interested parties. In addition, the report will be available at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions about this report, please contact me at curdae@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix II.
Sincerely,

Elizabeth H. Curda
Director, Education, Workforce, and Income Security
Elizabeth H. Curda, curdae@gao.gov
In addition to the contact named above, James Whitcomb (Assistant Director), Brittni Milam (Analyst in Charge), Christian Burks, and MacKenzie Cooper made key contributions to this report. Also contributing to this report were James Bennett, Robert Bullock, Alex Galuten, Margaret Hettinger, Gina Hoover, Zachary Sivo, Joy Solmonson, Jessica L. Yutzy, and Christopher Zbrozek.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on X,
LinkedIn, Instagram, and YouTube.
Subscribe to our Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]This report presents the final results of our review. We testified about the initial findings of our review in September 2024. See VA Disability Exams: Improvements Needed to Strengthen Oversight of Contractors’ Corrective Actions, GAO‑24‑107730 (Washington, D.C.: Sept. 18, 2024).
[2]According to VBA officials, during our review four contractors held 13 contracts for post-discharge disability exams performed in the U.S. and the performance work statements for these 13 contracts were identical. Officials said they reached the maximum number of exams allowed on these 13 contracts and, in December 2024, awarded 13 new contracts. The officials provided a revised performance work statement for the new contracts and confirmed that this revised performance work statement was identical for each of the 13 new contracts. We reviewed both the former and revised performance work statements and found the clauses we reference in this report were substantially similar in both. Because the relevant information is consistent across performance work statements, in this report we refer to the performance work statement (singular). We excluded other contracts from our scope, which officials said included three contracts for pre-discharge exams of active service members and two contracts for exams outside the U.S.
[3]We chose these years because 2018 was the first year we released a report on VBA’s management of contracted disability exams. See GAO, VA Disability Exams: Improved Performance Analysis and Training Oversight Needed for Contracted Exams, GAO‑19‑13 (Washington, D.C.: Oct. 12, 2018).
[4]MDEO calculates quarterly financial rewards and penalties for each contract based on performance. We use the term “financial incentives” to include both rewards and penalties, which MDEO calls “positive incentives” and “negative incentives.”
[5]We used MDEO’s performance data and did not independently assess contractors’ performance under the contracts.
[6]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: Sept. 2014), principles 10 and 13.
[7]Claims processors are regional VBA staff who request disability exams and make determinations on veterans’ claims.
[8]We were unable to interview the other two examiners we selected: a psychologist and a neurologist.
[9]GAO, Evidence-based Policymaking: Practices to help Manage and Asses the Results of Federal Efforts, GAO‑23‑105460 (Washington, D.C.: July 2023).
[10]Pub. L. No. 117-168, 136 Stat. 1759. Among other things, the PACT Act changed certain disability compensation examination requirements and expanded presumptive conditions associated with exposure to burn pits and other toxins. This resulted in a potential increase in eligibility for certain health care and benefits.
[11]MDEO has an executive office and five components: (1) Data and Operations, (2) Quality, (3) Policy and Program Management, (4) Acquisitions and Budget, and (5) Training and Development. Within its executive office, MDEO also has an Inquiries team that serves as a point of contact for internal and external stakeholders.
[12]GAO’s High-Risk List focuses attention on government operations that are vulnerable to fraud, waste, abuse, or mismanagement, or are in need of transformation to address economy, efficiency, or effectiveness challenges. Our 2025 High-Risk Report provides VA a road map for better managing its disability workloads and updating its disability benefit eligibility criteria. See High-Risk Series: Heightened Attention Could Save Billions More and Improve Government Efficiency and Effectiveness, GAO‑25‑107743 (Washington, D.C.: Feb. 25, 2025).
[13]The report contains two lists. One includes the DBQs that claims processors most frequently sent back to the examiners for clarification or additional information, through a process known as rework. This list is specific to each contractor. The second list comes from VBA’s national-level Systematic Technical Accuracy Review program that reviews a random sample of claims for accuracy. It includes the DBQs found to have had an insufficient exam across all contractors, so each contractor receives the same list. For more information, see table 2 in GAO‑24‑107730.
[15]MDEO updated the procedures in December 2024 to stipulate that analysts reviewing each contractor’s action plans should confirm that corrective actions for that quarter were completed and evaluate the effectiveness of the plans. This update provides improved guidance, but the procedures do not provide detail on how to identify and evaluate the effect of the action plans on exam quality. We will continue to monitor VBA’s efforts to fully implement the recommendation.
[16]According to MDEO documents, the sample is randomly selected to ensure a 95 percent confidence level and a 2.5 percent margin of error.
[17]The checklist was created in 2016 and updated in 2021 after a 2-year study, according to the study report. A multidisciplinary team analyzed qualitative and quantitative data to recommend the updates, which MDEO piloted with Quality Analysts. MDEO hired a consultant to review the process and its findings, including surveying subject matter experts and analyzing the results of the pilot, before implementing the new checklist.
[18]As we reported in September 2024, MDEO’s oversight of contracted exam quality includes techniques to prevent, detect, and correct exam errors. GAO‑24‑107730.
[19]According to the analysis, the remaining 6 percent affected claim outcomes but did not need a new exam to rectify the error.
[20]MDEO officials said the contract for administering the customer satisfaction survey was canceled in February 2025, halting survey administration. They said they are working with another VA office to administer the survey in the future. Until the new survey begins, MDEO is excluding the customer satisfaction measure from its financial incentive calculations.
[21]During the period we studied (fiscal years 2023 and 2024), MDEO validated the accuracy of these data using various methods. However, MDEO officials told us their data validation contract for the Production, Average Days to Complete, and Average Days Pending measures was canceled as of February 2025. Officials said another VBA office will validate these data in the future, and they do not expect any interruptions in the calculation of financial incentives due to data validation.
[22]If any of the five performance measures was below the minimally acceptable performance threshold, the contract was not eligible for any rewards on the other performance measures. In these cases, the COR summed any negative percentages but not the positive percentages.
[23]MDEO began issuing financial incentives in the third quarter of fiscal year 2022. We reviewed the calculations for financial incentives beginning in the third quarter of fiscal year 2023, when MDEO implemented an updated method for calculating these incentives.
[24]GAO‑14‑704G, principles 10 and 13.
[25]According to the performance work statement, contractors are required to comply with any corrective actions resulting from SFRs. Corrective actions may include retraining for contracted examiners.
[26]MDEO uses both “examiner” and “provider” to refer to contracted examiners. For consistency, we use “examiner” in this report.
[27]See GAO, VA Disability Exams: Better Planning Needed as Use of Contracted Examiners Continues to Grow, GAO‑21‑444T (Washington, D.C.: Mar. 23, 2021).
[28]The contractors responsible for providing disability exams administered the post-exam surveys until April 2024 when, according to MDEO officials, a third-party vendor assumed this responsibility. As previously noted, MDEO officials told us this third-party contract was canceled in February 2025, halting survey administration. The officials also said they are working with another VA office to administer the survey in the future.
[29]Contractors can have a variety of relationships with examiners, according to MDEO officials and examiners we spoke with. For example, the contractor may employ an examiner, may enter into a contract with a company that employs an examiner, or may enter into a contract directly with an examiner. Examiners may conduct exams for more than one contractor.
[30]The Board of Veterans’ Appeals adjudicates appealed cases in which a veteran is dissatisfied with VBA’s initial decision on their claim.
[31]The DBQ Change Control Group includes representatives from MDEO’s Policy and Program Management Office, MDEO’s Quality team, Compensation Services, the Board of Veterans’ Appeals, VA’s Offices of Business Process Integration and Information and Technology Product Development, and the Veterans Health Administration’s Office of Disability and Medical Assessment. Each entity votes on proposed changes to DBQs.
[32]According to officials, they awarded this new contract because they had reached the maximum number of exams allowed under the prior contract.
[33]The sixth examiner told us the contractor they work with has been very helpful in answering questions.
[34]According to officials, in fiscal year 2024 MDEO conducted 405 site visits. Based on our analysis of agency data, this covered approximately 4.8 percent of examiners conducting domestic, post-military discharge exams.
[35]Strategic planning documents available during the course of our audit included an MDEO “Roadmap” identifying goals and objectives and VA’s Fiscal Years 2022-28 Strategic Plan. In April 2025, VBA officials told us the agency’s strategic plan is no longer published, because it is under review, but said it remains applicable nonetheless.
