DEFENSE HEALTH CARE
Information on DOD’s Processing of TRICARE Claims from Behavioral Health Providers
Report to Congressional Committees
United States Government Accountability Office
For more information, contact Sharon Silas at silass@gao.gov.
Highlights of GAO-25-107484, a report to congressional committees
Information on DOD’s Processing of TRICARE Claims from Behavioral Health Providers
Why GAO Did This Study
To support military deployments and provide health care, including behavioral health care, DOD operates a health system known as TRICARE. This system offers behavioral health and other services to over nine million eligible beneficiaries in military hospitals and clinics, or through authorized civilian providers in the private sector.
The Conference Report 118-301 accompanying the National Defense Authorization Act for Fiscal Year 2024 includes a provision for GAO to report on TRICARE’s payments to civilian network behavioral health providers. This report examines (1) the timeliness of TRICARE claims processing and (2) DOD’s oversight of payment accuracy to all civilian providers, including behavioral health providers.
GAO reviewed relevant documents, such as DOD and contractor reports for timeliness and accuracy, and DOD’s oversight plans for the TRICARE contracts. GAO also analyzed time frames for processing claims from behavioral health providers from 2018 through 2023 and audit findings on payment accuracy. Finally, GAO interviewed DOD officials with oversight responsibilities of TRICARE’s contractors, contractor staff, and four selected behavioral health provider groups who participate in TRICARE. GAO compared DOD’s oversight activities to a DOD goal and a recommended practice.
What GAO Found
The Department of Defense’s (DOD) two managed care support contractors generally processed TRICARE claims for care provided between 2018 and 2023 within required timeliness standards. The claims process involves determining payment amounts to civilian health care providers, including behavioral health providers. DOD’s timeliness standards require contractors to process 98 percent of TRICARE claims within 30 days, and 100 percent of claims within 90 days.
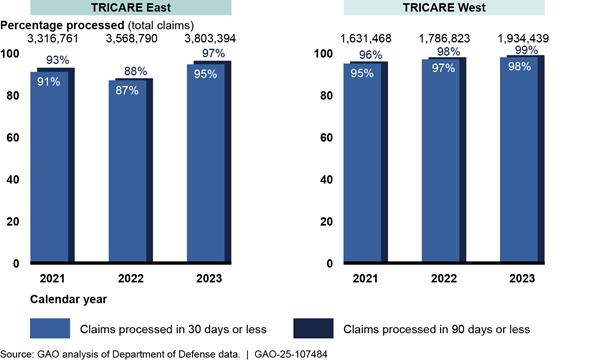
Although DOD does not apply these standards to specific provider types, GAO separately analyzed the nearly 28 million claims from behavioral health providers over the 6-year period. GAO found that almost 90 percent were processed in 30 days. In addition, the percentage of claims processed within 30 and 90 days generally increased each year (see figure for the 3 most recent years).
To oversee TRICARE payment accuracy, DOD monitored internal and external audit reports of randomly sampled claims from all types of providers, including behavioral health providers. DOD assessed contractor performance on all audited claims against the payment accuracy standards—which require payment error rates to not exceed between 2 and 1.75 percent, depending on the year of the contract—and took action when necessary. Across the audit reports from 2018 through 2023, claims from behavioral health providers made up between 1 and 8 percent of audited claims.
DOD’s oversight actions were consistent with its oversight goal for early identification and resolution of performance issues, and with a recommended practice from the Office of Management and Budget and prior GAO work that federal agencies use multiple sources of evidence to support decision-making.
|
Abbreviations |
|
|
|
|
|
DHA |
Defense Health Agency |
|
DOD |
Department of Defense |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
May 13, 2025
The Honorable Roger Wicker
Chairman
The Honorable Jack Reed
Ranking Member
Committee on Armed Services
United States Senate
The Honorable Mike Rogers
Chairman
The Honorable Adam Smith
Ranking Member
Committee on Armed Services
House of Representatives
Military service, especially combat, can carry a psychological cost for members of the military and their families. Further, untreated behavioral health conditions, which include mental health and substance use disorders, can affect readiness for military deployment and have a variety of other negative consequences.[1] As such, behavioral health care is an essential part of the full range of medical care and services that the Department of Defense (DOD) offers to over nine million eligible beneficiaries, including active duty service members, retirees, and their eligible family members.[2] DOD’s Defense Health Agency (DHA) offers medical care, including behavioral health services, through its health system known as TRICARE. Beneficiaries can obtain these services through DOD’s direct care system of military hospitals and clinics, or through authorized civilian providers in the private sector.
DOD military hospitals and clinics in the direct care system prioritize care for active duty service members above other TRICARE beneficiaries, such as eligible family members and retirees. As a result, DOD relies on civilian providers to provide care to these other beneficiaries—who comprised about 85 percent of beneficiaries at the end of fiscal year 2023.
These civilian providers must submit claims for payment. Processing delays or payment errors could affect their willingness to see TRICARE beneficiaries and in turn affect beneficiaries’ ability to access care. DOD uses managed care support contractors (contractors) to develop networks of civilian health care providers, and to process and pay claims for care provided by TRICARE-authorized providers.[3]
The Conference Report 118-301 accompanying the National Defense Authorization Act for Fiscal Year 2024 contains a provision for us to report on TRICARE’s payments to civilian network behavioral health providers.[4] In this report, we
1. Examine the extent to which DHA contractors processed TRICARE claims in a timely manner, including claims from behavioral health providers, and
2. Examine the extent to which DHA oversaw TRICARE payment accuracy across all providers, including behavioral health providers.
To address both objectives, we reviewed relevant portions of two generations of DOD’s two managed care support contracts: the T-2017 contracts, with health care delivery in effect from 2018 through 2024, and the T-5 contracts, which started health care delivery in January 2025.[5] Our review of these contracts included identifying contract requirements related to the timeliness and accuracy of payments, and determining whether there had been any changes to these requirements. These contracts include, by reference, the TRICARE Operations Manual, which provides instructions to DHA’s contractors for implementing contract requirements. In addition, we interviewed DHA officials responsible for overseeing the TRICARE managed care support contracts. We also interviewed representatives from the two contractors, Humana Government Business, Inc., and Health Net Federal Services, LLC, under the T-2017 contracts, which were the focus of our review.[6] Further, we interviewed four groups who represent behavioral health providers in their respective states to ask about providers’ experiences regarding the timeliness and accuracy of payments from the TRICARE program. To do so, we identified one group representing behavioral health providers from each of the top three states with the highest volume of claims from such providers, in each TRICARE region, from 2018 through 2023.[7] A group from one state declined to participate, and a group in another state did not respond, resulting in interviews with provider groups in Florida and Virginia in the TRICARE East region, and Colorado and Washington in the TRICARE West region.[8]
To examine the extent to which DHA contractors processed TRICARE claims in a timely manner, including claims from civilian behavioral health providers, we conducted three types of analyses covering TRICARE-authorized providers—that is, both network and non-network providers.
· The first analysis examined the timeliness of processing TRICARE claims from all providers for care provided from January 1, 2018, through December 31, 2023—the most recent complete years available at the time of our review.
· The second analysis examined the timeliness of processing claims from behavioral health providers for care provided from January 1, 2018, through December 31, 2023.
· The third analysis compared claims from behavioral health providers to a comparable group of provider types for care provided during calendar year 2023.
We used January 1, 2018, as the beginning date for our analyses to align with the start of health care delivery under the T-2017 contracts. We defined behavioral health providers as those who diagnose and treat mental health conditions and substance use disorders, excluding facilities.[9] For additional information about the methodology for these analyses and our data reliability assessments, see appendix I.
To examine how DHA oversaw TRICARE payment accuracy for all TRICARE-authorized providers under the T-2017 contracts, including behavioral health providers, we reviewed quarterly reports of audits, conducted by the contractors and by an external auditor, on TRICARE claims processed from January 1, 2018, through December 31, 2023. We also reviewed documentation related to actions that DHA took to address a contractor performance deficiency in claims’ payment accuracy. Lastly, we interviewed DHA officials responsible for overseeing the contract for the external auditor. We did not identify any missing data, outliers, or obvious errors in the external audit reports’ findings, and the reports were corroborated by the corrective action documentation. As a result, we determined the data to be sufficiently reliable for reporting on DHA’s oversight of payment accuracy. We compared DHA’s oversight activities for claims payment accuracy to a DHA goal for early detection and resolution of performance issues included in the agency’s plan for overseeing contractor performance. Our criteria for this objective also included a recommended practice from the Office of Management and Budget and our prior work that federal agencies use multiple sources of evidence in managing and assessing the results of federal efforts.[10]
We conducted this performance audit from March 2024 to May 2025 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
TRICARE Regional Structure and Contracts
TRICARE is organized into two regions in the U.S.—East and West. DHA manages civilian health care in each of these regions through contractors. Under the previous, fourth generation of TRICARE contracts (known as “T-2017”), health care delivery began January 1, 2018, and continued through December 31, 2024. The contractors were Humana Government Business, Inc. (TRICARE East region contractor) and Health Net Federal Services, LLC (TRICARE West region contractor). DHA’s current generation of TRICARE contracts (the fifth generation, known as “T-5”) began health care delivery on January 1, 2025. Although the number of TRICARE regions remains at two under T-5, the regional boundaries and the TRICARE West region contractor changed between the T-2017 and T-5 contracts (see fig. 1).[11]
Figure 1: Changes to the Boundaries of TRICARE Regions Under the Fourth and Fifth Generations of TRICARE’s Managed Care Support Contracts (T-2017 and T-5)
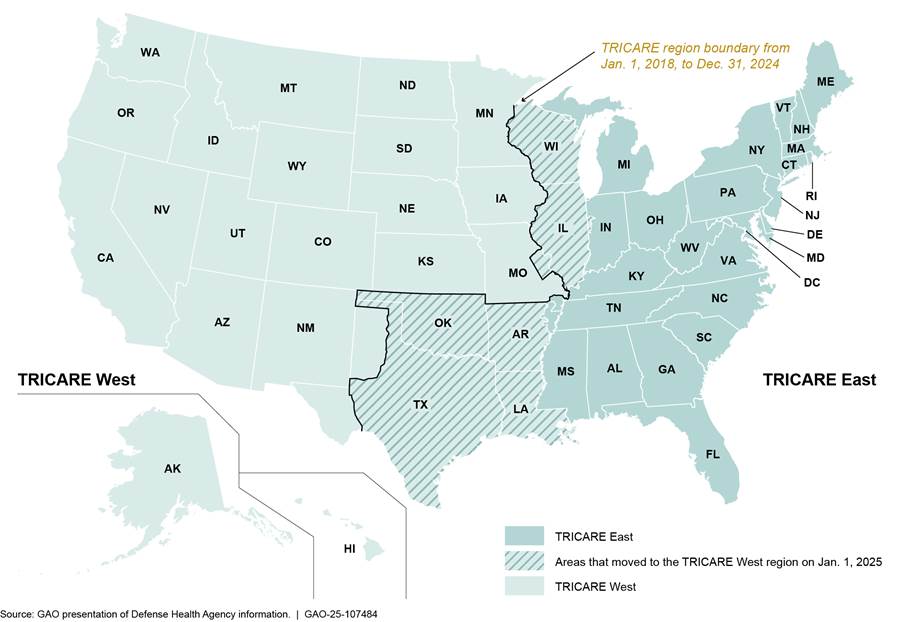
Note: According to Defense Health Agency data from November 2024, there were approximately 8.9 million eligible beneficiaries in the two regions. Under the T-2017 contracts’ regional boundaries, the TRICARE East region had approximately 6.1 million beneficiaries and the TRICARE West region had approximately 2.8 million beneficiaries. Under the T-5 contracts’ regional boundaries, the TRICARE East region would have approximately 4.7 million beneficiaries and the TRICARE West region would have approximately 4.2 million beneficiaries.
DHA’s contractors develop networks of civilian health care providers in these regions, and the contractors are also responsible for processing and paying TRICARE claims for care provided by these providers. The contractors must follow contractual requirements that include processing and paying claims received from civilian providers for covered services in accordance with law, regulation, and TRICARE policy. Contractors are also required to meet performance standards related to the timeliness and accuracy of these payments. During the contractors’ processing of TRICARE claims, the claims go through several key steps, including determining the accurate payment amount or whether the payment will be denied (see fig. 2). For more information on how DHA determines TRICARE payment rates, see appendix II.
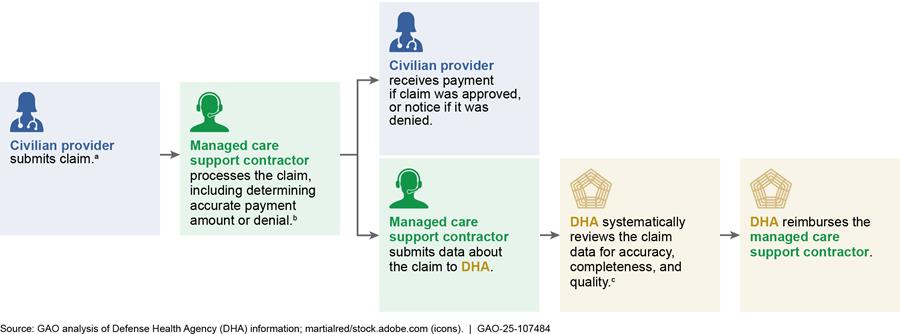
Note: The figure depicts the process by which claims are processed for healthcare services covered under the managed care support contracts provided outside the direct care system. Certain TRICARE-eligible beneficiaries’ health care costs are excluded from the underwritten costs of the contract (e.g., active duty service members), and follow a different approval and payment process for payment of claims for care provided in the community.
aProviders generally have up to 1 year from date of service to submit a claim for payment.
bPayment amounts are affected by factors such as type of facility, provider specialty, provider network status, and geographic location. If more information is needed to process the claim, the contractor can return the claim to the provider for additional information.
cIf needed, DHA can return the claim data to the contractor for edits.
TRICARE Contract Standards for Timeliness and Accuracy of Claims Processing
The managed care support contracts include performance standards for the timeliness and accuracy of claims processing. Specifically, for the timeliness of claims processing under the T-2017 contracts, the standards stipulated that 98 percent of all claims must be processed within 30 days, and 100 percent of claims within 90 days (with rounding included in both standards).[12] These timeliness standards are the same in the T-5 contracts.
· The starting point for measuring timeliness is the date the contractor files a received claim in its system. This filing date may differ from when the claim is first received because the contractor may need to send claims back to providers for additional information or corrections.
· The end point for measuring timeliness is the date that the contractor processes the claim to completion. This is the date when all services and supplies on the claim have been adjudicated, payment has been determined or denied, and the contractor has submitted data about the claim to DHA.[13]
Performance standards for the accuracy of claims processing under the T-2017 contracts stipulated that the payment error rate must not exceed 2 percent in the first 2 years of health care delivery (i.e., 2018 and 2019) and 1.75 percent thereafter. This standard is the same in the T-5 contracts.[14] To calculate the payment error rate under the T-2017 contracts, the absolute value of all payment errors—which can be positive (overpayment) or negative (underpayment)—is divided by the total billed amounts across all claims in the sample.
DHA’s Oversight of TRICARE Standards for Timeliness and Accuracy of Claims Processing
DHA is responsible for oversight of the contractors’ performance, including assessing performance against the contractual standards for timeliness and accuracy of claims processing. To help conduct this oversight, DHA monitors claims processing performance. Specifically, DHA’s subject matter experts are responsible for providing continuous technical oversight, documenting evaluation of contractor performance, and providing regular input on contractor performance to the contracting officer’s representative, including about any identified deficiencies. The contracting officer’s representative is responsible for documenting any deficiencies and communicating performance problems to the contracting officer, who ultimately ensures compliance with contract terms and determines final assessment of the contractor’s performance.
The contracting officer may take actions in response to a performance deficiency by issuing a formal corrective action request or, according to DHA officials, taking other corrective actions.
· Corrective action request. The contracting officer can make a formal request for the contractor to develop and submit for approval a corrective action plan to detail root causes of the deficiency and how it will be fixed. DHA would continue monitoring performance to determine when the deficiency was addressed and the performance standard had been sufficiently met. DHA would then notify the contractor that the corrective action plan was closed. In addition, corrective action requests and the contractor’s actions in response can affect DHA’s overall performance evaluation of the contractor.
· Other corrective actions. The contracting officer may decide to take other, more informal actions if they determine that the deficiency does not require a corrective action request, according to DHA officials. In doing so, the contracting officer may consider whether the performance deficiency affected any beneficiaries, caused financial or access to care issues, or whether the contractor can correct the performance immediately. DHA officials said these other, more informal actions include requesting the contractor to write a memo, informational paper, or other type of response documenting how it will address the inadequacies.
DHA Contractors Generally Processed TRICARE Claims in a Timely Manner, and Processed Claims from Behavioral Health Providers in a Similar Amount of Time
In reviewing monthly reports DHA uses to oversee the timeliness of claims processing, we found that DHA’s contractors generally processed TRICARE claims submitted for care provided between calendar years 2018 and 2023 within DHA’s claims processing standards. When we analyzed data from a subset of these claims that were from behavioral health providers, we found that these claims were processed in a similar amount of time, with almost 90 percent of claims processed within 30 days.
Timeliness of Claims Processing for All TRICARE Claims
|
TRICARE Claims Processing Standards for Timeliness The managed care support contractors for the Defense Health Agency’s T-2017 TRICARE contracts include two timeliness standards for processing claims: · 98 percent of retained and adjusted claims (e.g., claims with enough information for processing or claims that were previously corrected) must be processed within 30 days; and · 100 percent of retained and excluded claims, including adjustments, (e.g., claims with enough information for processing, claims that were previously corrected, or claims that required more information) must be processed within 90 days. Source: T-2017 TRICARE Operations Manual. | GAO‑25‑107484 |
According to data that the contractors are required to submit monthly to DHA, the contractors generally met DHA’s claims processing standards for timeliness, with some variation by contractor.[15] Specifically, in 65 of 72 months the TRICARE East region contractor met the standard for processing 98 percent or more of its approximately 243 million claims within 30 days.[16] The TRICARE West region contractor met the same standard for its approximately 101 million claims in 72 of 72 months (see fig. 3).[17] Further, both contractors met the standard of processing 100 percent of claims within 90 days across all 72 months we reviewed.
Figure 3: Timeliness of TRICARE Claims Processing for Care Provided During Calendar Years 2018-2023, by Managed Care Support Contractor
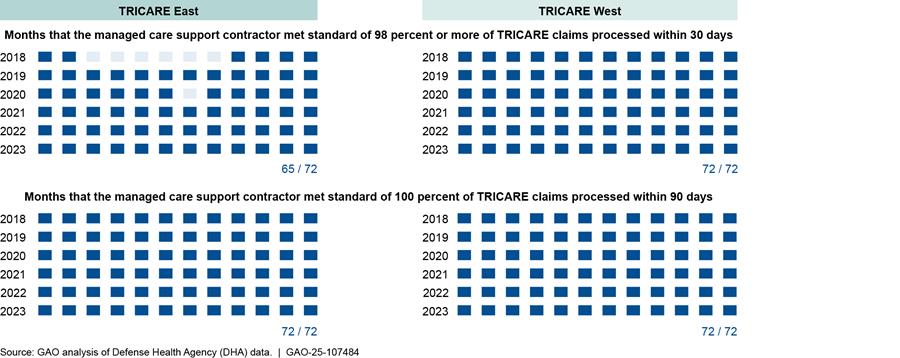
Notes: The data on claims processing are submitted monthly by the managed care support contractors to DHA. The number of days it took to process a claim represents the time elapsed from the filing date of the claim (the date the provider submitted the claim to the managed care support contractor) and the date the claim was processed to completion (meaning the claim has been adjudicated and payment/deductible/denial has been posted). DHA officials also confirmed that this is close to the date by which a provider has been sent payment or notice of denial has been issued.
DHA requires its managed care support contractors to process to completion 98 percent of claims within 30 days of receipt of a TRICARE claim, and 100 percent of claims within 90 days. These standards apply to all claims processed by the contractor each month—they are not specific to a certain type of provider. The TRICARE West region contractor received a waiver, or relief, from processing 98 percent or more of its claims within 30 days for 1 month in March 2019, due to delays in information from the federal government. Further, DHA’s instructions for calculating performance standards provide for rounding. Therefore, a contractor could meet this 98 percent standard by processing 97.5 percent of claims within 30 days, and it could meet the 100 percent standard by processing 99.5 percent of claims within 90 days. This occurred for some of the months we reviewed.
Of the 7 months in our review when the TRICARE East region contractor did not process 98 percent of claims within 30 days, 6 occurred in 2018—the first year of the T-2017 contracts. Because of this and other concerns, DHA submitted a formal corrective action request to the TRICARE East region contractor in April 2018.[18]
The TRICARE East region contractor responded with a corrective action plan, which identified underlying issues causing its claims processing deficiencies. In its plan, the TRICARE East region contractor also included several corrective actions it planned to take to address these deficiencies. Because the TRICARE East region contractor made changes and later met the 30-day claims processing standard for several consecutive months, DHA determined that the contractor had successfully implemented the corrective action plan in September 2019. Since then, there was 1 additional month in which the TRICARE East region contractor missed processing 98 percent of claims within 30 days. DHA officials told us that they did not need to issue a formal corrective action request because they determined that the single occurrence did not indicate a trend of poor performance.
Time to Process TRICARE Claims Submitted by Behavioral Health Providers
When we analyzed the subset of these claims that were from behavioral health providers, we found that almost 90 percent of the nearly 28 million claims were processed in 30 days.[19] Although DHA does not separately apply its timeliness standards for processing claims by specific subsets of providers, such as behavioral health providers, we used 30 days and 90 days as categories of time to assess the claims from these providers, similar to the contract timeframes for all claims.[20]
Across all 6 years from 2018 through 2023, we found that the time it took to process claims from behavioral health providers differed by contractor:
· For the TRICARE East region contractor, the median processing time across its approximately 18.8 million claims from behavioral health providers was 1 day; the contractor processed 84 percent of these claims within 30 days.[21]
· For the TRICARE West region contractor, the median processing time across its approximately 9 million claims from behavioral health providers was 2 days; the contractor processed 93 percent of these claims within 30 days.[22]
Additionally, the number of claims from behavioral health providers that were processed by the contractors within 30 and 90 days generally increased each year of our review (see fig. 4).
Figure 4: Time to Process TRICARE Claims Submitted by Civilian Behavioral Health Providers for Care Provided During Calendar Years 2018-2023, by Managed Care Support Contractor
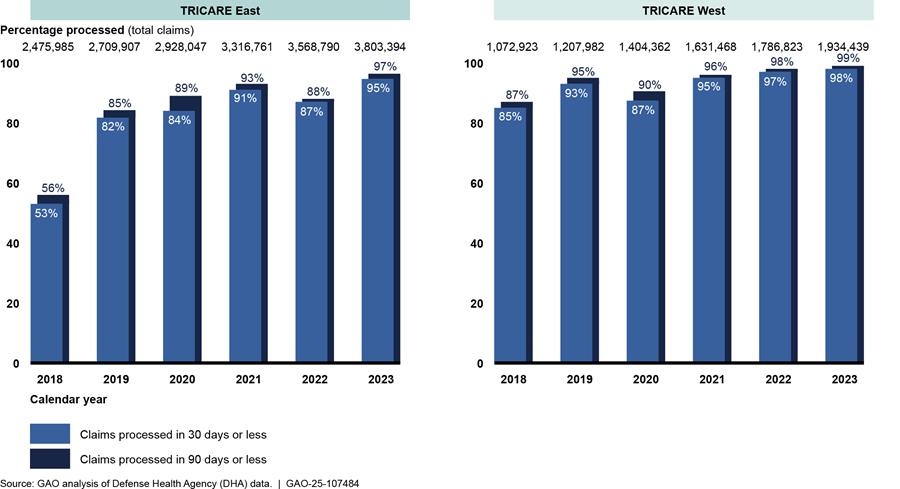
Note: For the purposes of this review, we defined behavioral health providers as those providers who diagnose and treat mental health conditions and substance use disorders. Further, our review is limited to payments to TRICARE-authorized providers for services rendered under the fourth generation of TRICARE managed care support contracts (“T-2017”) from calendar years 2018 through 2023 to individual behavioral health professionals, and not to facilities such as hospitals and inpatient residential facilities.
Under T-2017, DHA officials told us that they did not have concerns about the amount of time it took to process claims from behavioral health providers, nor had they received questions regarding how long it took for these providers to be paid. Further, the behavioral health provider groups we interviewed did not express specific concerns about the timeliness of TRICARE payments under T-2017.
For additional context, we then compared our analysis of claims from behavioral health providers to a comparable analysis of TRICARE claims provided by DHA for care provided during the most recent year available at the time of our review (calendar year 2023).[23] DHA’s analysis allows us to compare claims from behavioral health providers to claims from any professional who diagnoses and treats medical conditions. Based on the results of this comparison, we found that the amount of time it took to process TRICARE claims from behavioral health providers was generally the same relative to claims from comparable providers, for both contractors (see table 1).
Table 1: Time to Process TRICARE Claims Submitted by Civilian Behavioral Health Providers Compared to Claims Submitted by Comparable Providers, for Care Provided During Calendar Year 2023
|
|
|
GAO analysis of claims |
DHA analysis of claims from comparable providers |
|
TRICARE East region contractor |
Percent of claims processed within 30 days |
95% |
95% |
|
Percent of claims processed within 90 days |
97% |
97% |
|
|
Total number of claims |
3,803,394 |
27,886,356 |
|
|
TRICARE West region contractor |
Percent of claims processed within 30 days |
98% |
97% |
|
Percent of claims processed within 90 days |
99% |
98% |
|
|
Total number of claims |
1,934,433 |
10,850,348 |
Source: GAO and Defense Health Agency (DHA) analyses of TRICARE claims data. | GAO‑25‑107484
Note: Our analysis of behavioral health claims reviewed payments to TRICARE-authorized, individual behavioral health professionals (not facilities). We also limited our analysis to claims from behavioral health providers who diagnose and treat behavioral health conditions (and not from support staff). Accordingly, we asked DHA to analyze the timeliness of claims processing for a comparable subset of claims from individual professionals across all specialties who could diagnose and treat beneficiaries. DHA’s analysis includes claims from behavioral health providers. We also requested the subset of claims be limited to those claims for which TRICARE paid some amount to a provider, and the claims were processed by the two managed care support contractors.
We also examined claims processing by the type of behavioral health provider that submitted the claim, such as a psychiatrist versus a social worker. Overall, we found general consistency in the amount of time it took to process claims from specific types of behavioral health providers for care provided during the most recent, complete year of data (calendar year 2023). Further, depending on behavioral health provider type, the contractors processed between 93 and 97 percent of these claims within 30 days. For example, 96 percent of claims from social workers and 97 percent of claims from marriage and family therapists were processed in 30 days. See appendix III for more information on the results by behavioral health provider type.
DHA Oversaw TRICARE Payment Accuracy by Monitoring Audits Across All Providers, Which Included Behavioral Health Providers
DHA monitored internal and external audit reports to help oversee TRICARE payment accuracy. Using these reports met a DHA goal and a recommended practice identified by the Office of Management and Budget and prior GAO work. DHA’s monitoring of TRICARE payment accuracy focused on claims from all types of providers, including behavioral health providers, rather than separately monitoring by different types of providers.
DHA Monitored Quarterly Audit Reports to Oversee TRICARE Payment Accuracy Across All Providers, Meeting an Internal Goal and Recommended Practice
|
Standards for Payment Accuracy The managed care support contractors for the Defense Health Agency’s T-2017 TRICARE contracts must have a payment error rate that does not exceed 2 percent in the first 2 years of health care delivery (i.e., 2018 and 2019) or 1.75 percent thereafter. Source: T-2017 TRICARE Operations Manual. | GAO‑25‑107484 |
To oversee TRICARE payment accuracy under the T-2017 contracts, DHA monitored quarterly internal audit reports produced by the contractors and quarterly external audit reports produced by a third party.[24] According to DHA and contractor documentation, in each of these audits the contractors and external auditor sampled processed claims each quarter using slightly different methodologies. Then, the contractors and external auditor reviewed adjudication documentation from the sampled claims to determine whether any payment errors had been made previously.[25] They reported payment errors to DHA each quarter, which enabled DHA to determine payment error rates. See table 2 for key characteristics of these audit reports.
Table 2. Key Characteristics of Internal and External Audit Reports Monitored by the Defense Health Agency (DHA) to Oversee TRICARE Payment Accuracy
|
Key characteristics |
Internal audit reports |
External audit reports |
|
Audit source |
Each managed care support contractor |
Independent, external contractora |
|
Audit frequency |
Quarterly |
Quarterly |
|
Report time frames |
Due 45 days after the end of the quarter |
No due date requirement, but report time frames averaged slightly more than 8 months after the end of the audited quarter, between calendar years 2018 and 2023b |
|
Relative sample sizes |
Fewer claims sampled than in external audit reports |
More claims sampled than in internal audit reports |
|
Rebuttal period |
Not applicable, as the managed care support contractor conducts the audits |
The managed care support contractors have 30 days to review and rebut findings |
Source: GAO analysis of DHA and managed care support contractor documentation. | GAO‑25‑107484
aThe external auditor’s contract, known as TRICARE Claims Review Services, started in 2017 and it continued through the scope of our analysis of the fourth generation of TRICARE managed care support contracts.
bWe analyzed the time for completion based on audit closure dates received from DHA.
DHA officials said they used the internal audit reports for early identification of potential systemic claims processing issues. When a problem is identified, DHA officials said that the contractors are to fix any identified payment errors, and then discuss them with DHA to help understand whether these payment errors indicate larger systemic issues. For example, such issues could include that multiple staff were making data entry errors and internal guidance may need to be updated or clarified.
In comparison, DHA officials said they used the external audit reports to determine whether any corrective action requests needed to be sent to the contractors.[26] For example, in April 2019 DHA issued a corrective action request to the TRICARE East region contractor because the external audit reports found payment error rates in 2 consecutive quarters that were higher than contractual standards. In response, the TRICARE East region contractor submitted its corrective action plan, which attributed its deficiencies to leadership and staff turnover, and to not implementing system changes to the claims processing system in a timely manner before the start of health care delivery for the T-2017 contract.
DHA determined the contractor had successfully implemented its plan to correct the deficiencies in April 2021, after external audit reports from 6 consecutive quarters—the first quarter of 2019 through the second quarter of 2020—showed performance within the standards. As shown in figure 5, the external audit reports found no further deficiencies of payment accuracy from either contractor under the T-2017 contracts.
Figure 5: Accuracy of Claims Processing from Calendar Years 2018-2023, by Managed Care Support Contractor
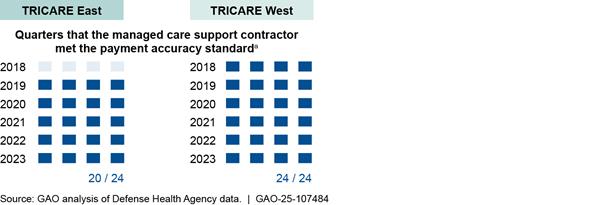
aThe payment accuracy standard stated that the payment error rate should not exceed 2 percent in 2018 or 2019, and 1.75 percent thereafter. Under this fourth generation of TRICARE contracts (known as “T-2017”), the rate was calculated by dividing the absolute value of payment errors in the audited sample of claims by the total billed amounts across claims of the sample.
DHA’s use of the internal audit reports is consistent with DHA’s goal for early detection and resolution of performance issues, as stated in DHA’s Quality Assurance Surveillance Plan for the T-2017 contracts.[27] The contractors were required to submit the internal audit reports to DHA within 45 days after the end of each quarter, which DHA officials confirmed the contractors regularly met. Without these reports, information about payment accuracy would take much longer; for example, past completion dates of the external audits from 2018 through 2023 indicated they took slightly more than 8 months on average after each quarter.[28]
Additionally, DHA’s use of both the internal and external audit reports to oversee TRICARE payment accuracy is consistent with a recommended practice identified by the Office of Management and Budget and in our past work, that federal agencies use multiple sources of evidence to support decision-making.[29] By relying on different audit reports—from each contractor and the external auditor—DHA is using multiple sources of evidence to monitor TRICARE payment accuracy. As stated in our past work, multiple evidence sources can help agencies assess, understand, and identify opportunities to improve the results of federal efforts.
DHA officials initially told us the requirement for contractors to produce internal audit reports was excluded from the current-generation T-5 contracts, which began health care delivery in January 2025. However, in response to our questions, DHA officials said in November 2024 that they discovered the exclusion was unintentional. As a result, DHA officials updated the T-5 requirements in February 2025 to include the internal audit reports. DHA officials said they do not anticipate any gap in the internal audit reports based on the initial exclusion, with the first reports due in May 2025.
DHA Monitoring of Payment Accuracy Covered All Types of Providers, Including Behavioral Health
Similar to its monitoring of claims for timeliness, DHA monitored TRICARE payment accuracy across claims from all provider types, rather than by type of individual provider who submitted the claim (such as for only claims from behavioral health providers). DHA officials said claims from behavioral health providers (which, based on our analysis, made up about 8 percent and 9 percent of all claims in the TRICARE East and West regions, respectively) would be included in the claim audits if selected via the random sampling methods. Our analysis found a range in the percentage of claims from behavioral health providers that were randomly sampled in the claim audits (see table 3).[30]
Table 3. Percentage of Audited TRICARE Claims That Came from Behavioral Health Providers, from 2018 to 2023, by Managed Care Support Contractor
|
Managed care support contractor |
Audit source |
Percent of audited claims that came from behavioral health providers |
|
TRICARE East |
Internal |
1% |
|
External |
3% |
|
|
TRICARE West |
Internal |
8% |
|
External |
5% |
Source: GAO analysis of Defense Health Agency (DHA) and managed care support contractor documentation. | GAO‑25‑107484
Note: The managed care support contractors’ internal audits randomly sampled processed claims and helped DHA to oversee managed care support contractor performance against the payment accuracy standard in the fourth generation of TRICARE contracts (T-2017). External audits were conducted by DHA’s external TRICARE Claims Review Services contractor. From 2018 through 2023, claims from behavioral health providers represented about 8 percent and 9 percent of all overall claims in the TRICARE East and West regions, respectively, based on our analysis. The payment accuracy standard applied to the processing of all claims, and there were no requirements to sample claims by provider type.
DHA officials explained that they do not separately apply the payment accuracy standard to any specific subset of the claims, such as for claims from behavioral health providers. They further told us that under T-2017, they had not heard complaints that payment accuracy for claims from behavioral health providers was different than for other claims from other provider types. Similarly, the behavioral health provider groups we interviewed did not relay concerns about the accuracy of TRICARE payments to behavioral health providers under T-2017.[31]
Agency Comments
We provided a draft of this report to DOD for review and
comment. DOD provided technical comments, which we incorporated as appropriate.
We are sending copies of this report to the appropriate congressional committees and the Secretary of Defense. In addition, the report is available at no charge on the GAO website at http://www.gao.gov.
If you or your staff have any questions about this report, please contact Sharon M. Silas at silass@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix IV.

Sharon M. Silas
Director, Health Care
Appendix I: Methodology for Examining the Timeliness of TRICARE Claims Processing from Civilian Providers
To examine the extent to which Defense Health Agency (DHA) contractors processed TRICARE claims in a timely manner, including claims from civilian behavioral health providers, we conducted three types of analyses covering TRICARE-authorized providers—that is, both network and non-network providers.[32] Specifically, we analyzed (1) the timeliness of processing TRICARE claims from all providers, (2) the timeliness of processing claims from behavioral health providers, and (3) a comparison of claims from behavioral health providers to a comparable group of provider types.
· Timeliness of processing TRICARE claims from all providers. We obtained and analyzed monthly claims processing summary reports from DHA that detailed the amount of time it took the contractors to process TRICARE claims for care that was provided from January 1, 2018, through December 31, 2023—all the complete years available under the T-2017 contracts at the time of our review. We compared the results of these reports against DHA’s claims timeliness processing standards that require 98 percent of claims to be processed within 30 days, and 100 percent of claims to be processed within 90 days.
· Timeliness of claims from behavioral health providers. We obtained claims data from DHA on claims submitted by behavioral health providers for care rendered from the same January 1, 2018, through December 31, 2023, time period. For our purposes, we defined behavioral health providers as those who diagnose and treat mental health conditions and substance use disorders. We then identified claims submitted by these providers using behavioral health taxonomy codes—such as psychiatrists and social workers—and we excluded claims from facilities.[33] We also selected for certain types of service and major diagnostic categories (such as mental health care and mental diseases and disorders, respectively) to confirm that the claims from the behavioral health providers were submitted for the purposes of providing behavioral health care. Lastly, we restricted this analysis to those providers who can make and treat medical diagnoses and excluded supporting staff.
We then analyzed the claims data from DHA on the almost 28 million resulting claims from behavioral health providers to determine how long the claims took to be processed—that is, the difference between the receipt of a TRICARE claim and the date that the claim was processed to completion.[34] Specifically, we determined the amount of time it took to process these claims (1) in aggregate, (2) by contractor, and (3) by type of behavioral health provider. Although DHA does not separately apply timeliness standards for processing claims by specific subset of providers (including behavioral health providers), we used 30 days and 90 days as categories of time to assess the behavioral health claims, similar to the contract timeframes for all claims. To assess the reliability of the claims data, we reviewed relevant documentation and interviewed DHA officials. We found these data to be sufficiently reliable for reporting on the timeliness of processing claims from behavioral health providers.
· Comparison of claims from behavioral health providers to a comparable group of all provider types. As a 1-year check, we asked DHA to analyze the amount of time it took the contractors to process TRICARE claims submitted for care rendered in calendar year 2023—the most recent, complete year available under the T-2017 contracts at the time of our review—from a comparable group of claims from all types of providers. Specifically, DHA analyzed the amount of time it took for claims to be processed from individual professionals (not facilities) who diagnose and treat conditions, from any provider type.[35] We then compared our results of the time it took to process claims from behavioral health providers for care in calendar year 2023 to the time it took to process claims for the comparable group from DHA’s analysis. To assess the reliability of the claims data, we reviewed relevant documentation and interviewed DHA officials. We found these data to be sufficiently reliable for reporting on the timeliness of processing claims from behavioral health providers to a comparable group of providers.
TRICARE payment rates to civilian providers may differ depending on whether a provider is a network or non-network provider for TRICARE. Additionally, payment rates to civilian providers are generally limited to Medicare’s rates; however, the Defense Health Agency (DHA) has some options for increasing TRICARE payment rates if needed to improve access to care.[36]
Types of TRICARE Providers
Civilian providers must be TRICARE-authorized to be paid for care under the program. Depending on the type of provider, TRICARE authorization may require a provider to be licensed by their state, privileged in a hospital accredited by a national organization, and meet other standards of the medical community. There are two types of authorized civilian providers—network and non-network providers.
· Network providers are TRICARE-authorized providers who enter into agreements with the regional managed care support contractor (contractor) to provide care to TRICARE beneficiaries and agree to accept TRICARE payment rates as payment in full. Network providers may also agree to accept lower payments as a condition of network membership.[37] According to DHA officials, under the previous generation of TRICARE managed care support contracts that ended December 31, 2024 (called “T-2017 contracts”) the contractors could negotiate discounts of varied amounts with their network providers. However, DHA officials told us that under the current generation of TRICARE managed care support contracts that began on January 1, 2025 (called “T-5 contracts”) DHA is limiting the percentage it will credit back to the contractors for negotiated provider discounts to up to 5 percent, which may result in the contractors not pursuing discounted rates above 5 percent off the TRICARE rate. This was done to better ensure negotiated discounts have no impact on beneficiaries’ access to care.
· Non-network providers are TRICARE-authorized providers who have not entered into agreements with the contractor to provide care to TRICARE beneficiaries. As such, non-network providers may accept the TRICARE rate as payment in full or they may charge up to 15 percent above the maximum allowable charge (i.e., 115 percent of the TRICARE allowable amount).[38] The beneficiary is responsible for paying the extra amount billed in addition to the required cost-shares.
Overview of TRICARE Rate Setting
By law, TRICARE payment rates for civilian providers are generally limited to Medicare rates (see text box).
|
Medicare Payment Amounts Under traditional Medicare, the Centers for Medicare & Medicaid Services sets payment amounts for physicians’ and other providers’ services based on the underlying relative values that the agency assigns to more than 10,000 services included in the Medicare physician fee schedule. A committee from the American Medical Association provides recommendations for these underlying relative values to the agency for its consideration. For each of these services, there are three relative value units that correspond to the three components of physician payment for each of these services. The three components are the following: · Physician work—the financial value of physicians’ labor (i.e., the time, effort, and skill that are associated with providing the service); · Practice expense—the costs incurred by physicians in employing office staff, renting office space, and buying supplies and equipment; and · Malpractice expense—the premiums paid by physicians for professional liability insurance. In addition, the Centers for Medicare & Medicaid Services uses three geographic practice cost indices (indices) to adjust each of the three relative value units to account for variations in physicians’ costs of providing care in different geographic areas. The indices are numerical factors expressed as the ratio of an area’s cost to the national average. For example, in 2025, the physician work index for Houston, Texas, was 1.014, which means that the physician work index value is 1.4 percent above the national average. To calculate the Medicare payment amount for a service in a particular geographic area, each of the three relative value units for a service is adjusted by the appropriate indices and then converted into a dollar amount using a conversion factor that the agency calculates. For more information, see, for example, GAO, Medicare Physician Payment Rates: Better Data and Greater Transparency Could Improve Accuracy, GAO-15-434 (Washington, D.C.: May 21, 2015) and Medicare: Performance-Based and Geographic Adjustments to Physician Payments, GAO-24-107106 (Washington, D.C.: Oct. 19, 2023). |
Source: GAO. | GAO‑25‑107484
Prior to fiscal year 1991, TRICARE rates were paid under a fee-for-service type program. However, beginning in fiscal year 1991, to control escalating health care costs, Congress instructed the Department of Defense (DOD) to gradually lower its rates for individual civilian providers to mirror those paid by Medicare. Congress specified that reductions to TRICARE rates were not to exceed 15 percent each year.[39]
As of October 2024, of the more than 10,000 services included in the Medicare physician fee schedule, DHA reported there are 45 procedure or service codes for which the TRICARE payment rate remains higher than that of Medicare. Twenty-four of these codes are for maternity procedures or services (see table 4).[40]
Table 4: Maternity Procedure or Service Codes for Which the TRICARE Payment Rate Remains Higher than Medicare Payment Rates, as of October 2024
|
Procedure or service codea |
Procedure/service performed |
Ratio of TRICARE to Medicare payment |
|
58323 |
Sperm washing |
1.123 |
|
58600 |
Division of fallopian tube |
1.052 |
|
58615 |
Occlude fallopian tube(s) |
1.089 |
|
59012 |
Fetal cord puncture prenatal |
1.239 |
|
59020 |
Fetal contract stress test |
1.285 |
|
59025 |
Fetal non-stress test |
1.011 |
|
59030 |
Fetal scalp blood sample |
1.324 |
|
59050 |
Fetal monitor w/report |
1.467 |
|
59051 |
Fetal monitor/interpret only |
1.322 |
|
59320 |
Revision of cervix-vaginal |
1.205 |
|
59325 |
Revision of cervix-abdominal |
1.176 |
|
59350 |
Repair of uterus |
1.310 |
|
59409 |
Obstetrical care |
1.233 |
|
59412 |
Antepartum manipulation |
1.226 |
|
59414 |
Deliver placenta |
1.310 |
|
59514 |
Cesarean delivery only |
1.274 |
|
59525 |
Remove uterus after cesarean |
1.067 |
|
59612 |
Vbac delivery only |
1.153 |
|
59620 |
Attempted vbac delivery only |
1.293 |
|
59840 |
Abortion-induced,d&c |
1.064 |
|
59850 |
Abortion-induced,d&e |
1.019 |
|
59856 |
Abortion-induced by suppositories |
1.048 |
|
59857 |
Abortion-induced by supp w/hysterotomy |
1.096 |
|
59866 |
Abortion (mpr=multifetal preg reduction) |
1.235 |
Source: Defense Health Agency. | GAO‑25‑107484
aThe procedure/service codes are Current Procedural Terminology codes, which comprise a set of codes, descriptions, and guidelines intended to describe procedures and services performed by physicians and other health care providers.
The remaining 21 codes are for clinical labs or non-maternity procedures or services (see table 5).[41]
Table 5: Clinical Labs or Non-Maternity Procedure or Service Codes for Which the TRICARE Payment Rate Remains Higher than Medicare Payment Rates, as of October 2024
|
Procedure or service codea |
Procedure/service performed |
Ratio of TRICARE to Medicare payment |
|
80055 |
Obstetric panel |
1.810 |
|
81201 |
Apc gene full sequence |
1.027 |
|
81223 |
Cftr gene full sequence |
4.125 |
|
81228 |
Cytog alys chrml abnr cgh |
1.069 |
|
81229 |
Cytog alys chrml abnr snpcgh |
2.018 |
|
81243 |
Fmr1 gen aly detc abnl allel |
5.620 |
|
81255 |
Hexa gene |
5.608 |
|
81257 |
Hba1/hba2 gene |
1.902 |
|
81400 |
Mopath procedure level 1 |
2.506 |
|
81401 |
Mopath procedure level 2 |
1.307 |
|
81402 |
Mopath procedure level 3 |
1.092 |
|
81403 |
Mopath procedure level 4 |
2.596 |
|
81404 |
Mopath procedure level 5 |
1.199 |
|
81405 |
Mopath procedure level 6 |
1.989 |
|
81406 |
Mopath procedure level 7 |
2.833 |
|
81508 |
Ftl cgen abnor two proteins |
1.222 |
|
86850 |
Rbc antibody screen |
1.642 |
|
87426 |
Sarscov coronavirus ag ia |
2.454 |
|
87811 |
Sars-cov-2 covid19 w/optic |
4.365 |
|
90863 |
Pharmacologic mgmt w/psytx |
1.605 |
|
92558 |
Evoked auditory test qual |
3.440 |
Source: Defense Health Agency. | GAO‑25‑107484
aThe procedure/service codes are Current Procedural Terminology codes, which comprise a set of codes, descriptions, and guidelines intended to describe procedures and services performed by physicians and other health care providers.
DHA has some options for adjusting TRICARE payment rates, if needed. Specifically, DHA has the authority to adjust TRICARE rates using waivers in areas where it determines that the rates have had a negative impact on TRICARE beneficiaries’ access to civilian providers. DHA can issue three types of waivers for individual health care professionals and other non-institutional, non-professional providers, depending on the type of adjustment that is needed.
· Locality waivers may be used to increase rates for specific medical services in specific areas where access to civilian providers has been severely impaired.[42] The resulting rate increase would be applied to both network and non-network civilian providers for the medical services identified in the areas where access is impaired. As of February 2025, DHA has 22 active locality waivers.
· Network waivers are used to increase reimbursement rates up to 15 percent above the TRICARE reimbursement rate for all network providers in a specific location, to ensure an adequate number and mix of primary and specialty care network civilian providers.[43] As of February 2025, DHA did not have any active network waivers.
· TRICARE rates can be restored in specific localities to the levels that existed before a reduction was made to align TRICARE rates with Medicare rates for both network and non-network providers.[44] As of February 2025, DHA did not have any active waivers of rate reductions.
In addition to TRICARE, other federal health care programs also have payment rates that are linked to Medicare. For example, the Indian Health Service, within the Department of Health and Human Services, applies Medicare payment methodologies to services covered by its “Purchased/Referred Care” program. In doing so, the agency and tribal facilities can pay a “Medicare-Like Rate” for non-hospital services for tribal members. This rate is a cap on the amount the Indian Health Service is responsible for paying.[45] Additionally, the Veterans Community Care Program within the Department of Veterans Affairs uses Medicare rates for all rates paid for veteran community hospital care, medical services, or extended care services, to the extent practicable or otherwise specified.[46]
Appendix III: Processing Times for TRICARE Claims for Care Provided in 2023 from Civilian Behavioral Health Providers
Table 6: Processing Times for TRICARE Claims Submitted by Civilian Behavioral Health Providers for Care Provided in Calendar Year 2023, by Provider Type
|
Type of behavioral provider |
Percent of claims processed within 30 daysa |
Percent of claims processed within 90 daysa |
Total number of claims |
|
Counselor |
96% |
97% |
1,586,177 |
|
Social worker |
96% |
97% |
992,203 |
|
Psychiatry & neurology |
96% |
97% |
779,540 |
|
Psychologist |
96% |
97% |
681,121 |
|
Behavior analyst |
93% |
96% |
456,963 |
|
Marriage & family therapist |
97% |
98% |
427,125 |
|
Nurse practitioner |
95% |
97% |
250,889 |
|
Clinical nurse specialist |
96% |
97% |
94,582 |
|
Assistant behavior analyst |
93% |
96% |
58,629 |
|
Clinical neuropsychologist |
94% |
96% |
9,425 |
|
Other providers not specific to behavioral healthb |
97% |
98% |
404,902 |
Source: GAO analysis of Defense Health Agency (DHA) claims data. | GAO‑25‑107484
Note: Claims may include more than one TRICARE-authorized provider on them, depending on the services rendered during the encounter. These claims are represented in each row for a provider type that provided care on that claim. Therefore, the total number of claims by behavioral health provider type in this table exceed the total number of unique claims from behavioral health providers in calendar year 2023, which was 5,737,833.
aDHA’s contracts with its managed care support contractors include the following claims processing standards for timeliness: 98 percent of retained and adjusted claims must be processed within 30 days; and 100 percent of retained and excluded claims, including adjustments, must be processed within 90 days. There is no separate timeliness standard for claims processing for specific subsets of providers, including behavioral health providers. However, GAO used 30 days and 90 days as categories of timeliness to assess data on claims from behavioral health providers, similar to the contract timeframes for all claims.
bOther types of providers not specific to behavioral health include types of providers that may diagnose and treat behavioral health-related diagnoses and accordingly submit claims for these behavioral health services, but do not exclusively treat them. For example, such providers may include occupational therapists; art, dance, music, and poetry therapists; pain, sports, and sleep medicine physicians; neurologists; and internal medicine physicians.
GAO Contact
Sharon M. Silas, silass@gao.gov.
Staff Acknowledgments
In addition to the contact named above, Jeff Mayhew (Assistant Director), Ann Tynan (Assistant Director), Topher Hoffmann (Analyst-in-Charge), Kaitlin Asaly, Sang Lee, and Jeffrey Tamburello made key contributions to this report. Also contributing were Sampada Acharya, Jacquelyn Hamilton, David Jones, Teague Lyons, and Cathy Hamann Whitmore.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on X,
LinkedIn, Instagram, and YouTube.
Subscribe to our Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]We define behavioral health conditions as all mental health conditions and substance use disorders that are included in the Diagnostic and Statistical Manual of Mental Disorders. Mental health conditions include anxiety disorders; mood disorders, such as depression; post-traumatic stress disorder; and schizophrenia. Substance use disorders include alcohol use disorder and opioid use disorder.
[2]TRICARE is also available to National Guard and Reserve members, retirees, and their eligible family members. Eligible family members include spouses and dependent children.
[3]To manage the TRICARE program, including processing provider claims, DHA uses managed care support contractors (contractors) in each of its East and West TRICARE regions. DHA has several other TRICARE contracts in place to provide dental and pharmacy benefits through the private sector in the U.S., as well as for care rendered overseas.
There are two types of authorized civilian providers—network and non-network providers. All civilian providers must be TRICARE-authorized to be paid for care under the program. Depending on the type of provider, TRICARE authorization may require a provider to be licensed by their state, privileged in a hospital accredited by a national organization, and meet other standards of the medical community.
[4]H.R. Rep. No. 118-301, at 1121 (2023) (Conf. Rep.).
[5]The fourth and most-recently completed generation of TRICARE managed care support contracts, known as “T-2017,” started health care delivery on January 1, 2018, through December 31, 2024. The current, fifth generation of contracts, known as “T-5,” started health care delivery on January 1, 2025. The T-5 contracts are expected to continue through June 2034, if all option periods are exercised with transition-out activities.
[6]The T-2017 TRICARE East contract was awarded to Humana Government Business, Inc., and the TRICARE West contract was awarded to Health Net Federal Services, LLC.
[7]We selected Florida, Texas, and Virginia in the TRICARE East region, and California, Colorado, and Washington in the TRICARE West region.
[8]The behavioral health provider group in California indicated they were unavailable and declined to participate, and the group in Texas did not respond.
[9]According to DHA officials, claims from facilities represented less than 1 percent of all TRICARE claims in calendar year 2023. Our resulting sample only included claims from professionals, regardless of whether the care was rendered in an inpatient or outpatient setting.
[10]See GAO, Evidence-Based Policymaking: Practices to Help Manage and Assess the Results of Federal Efforts, GAO‑23‑105460 (Washington, D.C.: July 12, 2023), and Office of Management and Budget, Memorandum for Heads of Executive Departments and Agencies, M-19-23 (Washington, D.C.: July 10, 2019).
[11]Under the T-5 contracts, Humana Government Business, Inc., manages the TRICARE East region and TriWest Healthcare Alliance Corp. manages the TRICARE West region.
[12]The 30-day standard applies to retained and adjusted claims, and the 90-day standard applies to retained and excluded claims, including adjustments. Retained claims are those that contain sufficient information to allow for processing to completion or have missing information that may be populated using internal sources. Excluded claims are those that need additional information for processing not available from internal sources, require development for third-party liability, or require intervention by the government or another contractor. An adjustment refers to a correction to a claim that was previously processed. Adjustments can be made for reasons such as recoupments, additional payments, cancellations, and corrections to data.
Further, DHA’s instructions for calculating performance standards provide for rounding. Therefore, a contractor could meet this 98 percent standard by processing 97.5 percent of claims within 30 days, and it could meet the 100 percent standard by processing 99.5 percent of claims within 90 days. This occurred for some of the months we reviewed.
[13]DHA officials also confirmed that this is close to the date by which provider payment or notice of denial has been issued.
[14]For the T-5 contracts, the payment error rate must not exceed 2 percent in the first 2 years of health care delivery (i.e., 2025 and 2026) and 1.75 percent thereafter.
[15]Time for claims processing is measured by the difference between the date the contractor files a received claim in its system (filing date) and the date that the claim is “processed to completion”—i.e., the date when all services and supplies on the claim have been adjudicated, payment has been determined, deductible has been applied, and payment/deductible/denial has been posted to history and the claim record. DHA officials also confirmed that this is close to the date by which payment has been sent to a provider or notice of denial has been issued.
[16]DHA’s instructions for calculating performance standards provide for rounding. Therefore, a contractor could meet this 98 percent standard by processing 97.5 percent of claims within 30 days, and it could meet the 100 percent standard by processing 99.5 percent of claims within 90 days. This occurred for some of the months we reviewed.
[17]The TRICARE West region contractor received a waiver, or relief, from processing 98 percent or more of its claims within 30 days for 1 month in March 2019, due to delays in information from the federal government.
[18]Other reasons included in the corrective action request were out of the scope of our review.
[19]The 27,840,776 claims represent at least 208,336 unique behavioral health providers across the 6 years. Not all claims we reviewed included a National Provider Identifier for us to use to identify providers. According to DHA officials, there have been delays in implementing this identifier in TRICARE records due to reasons such as transitions and funding. Therefore, we could not verify the identity of behavioral health providers on claims missing this element.
[20]DHA officials told us that they could monitor the timeliness of claims to specific types of providers if the officials had concerns. For example, in January 2018, DHA had concerns about the timeliness of the TRICARE East region contractor’s payments to applied behavior analysis claims. In response, the TRICARE East region contractor provided DHA with metrics related to performance for these claims and provider outreach.
[21]The TRICARE East region contractor processed 18,802,808 claims from behavioral health providers across the 6 years. That contractor reported that 47,279 (less than 1 percent) of these claims were initially returned to providers for additional information before resubmission and processing, sometimes more than once.
[22]The TRICARE West region contractor estimated that approximately 12,600 (less than 1 percent) of its total 9,037,968 claims from behavioral health providers were initially returned to providers for more information before resubmission and processing.
[23]We asked DHA to analyze the amount of time it took to process claims for care provided in calendar year 2023 from individual professionals (not facilities) who diagnose and treat conditions (i.e., have the same skill level as our universe of identified behavioral health providers). Individual professionals may include physicians and mid-level providers such as nurse practitioners. This may include claims from primary care, specialty, and behavioral health providers, but would exclude claims from supporting staff, such as health technicians. DHA’s analysis includes claims from behavioral health providers.
[24]Our review period consisted of claims processed from calendar years 2018 through 2023 under the T-2017 contracts. DHA officials confirmed there are no significant changes planned for oversight of payment accuracy under the T-5 contracts. The external auditor’s contract, known as TRICARE Claims Review Services, started in 2017, and it continued through the scope of our analysis of the T-2017 contracts.
[25]According to the external auditor’s contract documentation, payment errors can result from issues including misapplication of the deductible, payment of non-covered services or supplies, payment of services or supplies for which a benefit cannot be determined based on the information available at the time of processing, or a payment in the correct amount but sent to the wrong payee.
[26]The external auditor’s contract states that it provides DHA an independent impartial review of the contractors and other TRICARE private sector care contractors, such as the TRICARE Pharmacy and TRICARE Overseas programs. The quarterly audits discussed above, and other audits the external auditor conducts on these programs, are further used to assist DHA in identifying and reporting improper payments for DHA’s private sector care system, to help meet requirements of the Payment Integrity Information Act of 2019.
[27]The Quality Assurance Surveillance Plan was DHA’s plan for determining whether the contractors were meeting the performance requirements and contract standards under the T-2017 contracts.
[28]There are several reasons why the external audits take longer to prepare than the internal contractor audits. For example, the external auditor did not have direct access to the necessary claim documentation, and they had bigger sample sizes than the internal audits. Additionally, DHA required the external auditor to provide each contractor the chance to review and rebut any identified payment errors as part of the audit process.
[29]See Office of Management and Budget, Memorandum for Heads of Executive Departments and Agencies, M-19-23 (Washington, D.C.: July 10, 2019), and GAO‑23‑105460.
[30]We did not calculate payment error rates among the audited behavioral health claims because the resulting payment error rate would not be generalizable due to the random sampling nature of the audit reports.
[31]Because of the lack of complaints as well as the external auditor independently evaluating TRICARE payment accuracy, we did not independently review claims documentation from behavioral health providers to assess payment accuracy. Further, our analysis of the timeliness of TRICARE claims processing for behavioral health providers did not indicate potential processing issues that would be unique to behavioral health providers.
[32]Civilian providers must be TRICARE-authorized to be paid for care under the program. Depending on the type of provider, TRICARE authorization may require a provider to be licensed by their state, privileged in a hospital accredited by a national organization, and meet other standards of the medical community. Thus, there are two types of authorized civilian providers—network and non-network providers.
Under the T-2017 contracts, health care delivery began January 1, 2018, and continued through December 31, 2024.
[33]A taxonomy code is a unique 10-character code that designates a provider’s classification and specialization. According to DHA officials, claims from inpatient facilities represented less than 1 percent of all TRICARE claims in calendar year 2023. Our resulting sample only included claims from professionals, regardless of whether the care was rendered in an inpatient or outpatient setting.
[34]The date that the claim was processed to completion reflects the date when all services and supplies on the claim have been adjudicated, payment has been determined, deductible has been applied, and payment/deductible/denial has been posted. DHA officials also confirmed that this is close to the date by which a provider has been paid or notice of denial has been issued.
[35]Individual professionals may include physicians and mid-level providers such as nurse practitioners. Further, DHA’s assessment may have included claims from primary care, specialty, and behavioral health providers. We excluded claims on supporting staff, such as health technicians.
[36]Medicare is the federally financed health insurance program for persons aged 65 or over, certain individuals with disabilities, and individuals with end-stage renal disease.
[37]DHA offers a financial incentive to the contractors for getting providers to accept to a discounted payment rate below the usual TRICARE payment rate. The purpose of this incentive is to encourage the contractors to negotiate discounts with network providers and thereby reduce the cost to the government for reimbursing for this care. The incentive is calculated based on total underwritten health care costs.
[38]To reimburse civilian physicians, DOD has established a fee schedule known as the Civilian Health and Medical Program of the Uniformed Services maximum allowable charge rates. The managed care support contractor shall allow the lesser of the billed charges or the balance billing limit (115 percent of allowable charge). If the charges on a claim are exempt from the balance billing limit, the contractor shall allow the billed charges.
[39]See 10 U.S.C. §§ 1079(h), 1086(f).
[40]Beginning in 1998, DOD established a policy that its payment rates for some maternity services and procedures must be set at the higher of the current Medicare fee or the 1997 Medicare fee.
[41]These are payment rates for professional (non-facility) charges.
[42]See 32 C.F.R. § 199.14(j)(1)(iv)(D) (2024).
[43]See 32 C.F.R. § 199.14(j)(1)(iv)(E) (2024).
[44]See 32 C.F.R. § 199.14(j)(1)(iv)(C) (2024).
[45]42 C.F.R. § 136.30 (2023).
[46]38 U.S.C. § 1703(i).
