ELECTRONIC HEALTH RECORD MODERNIZATION
VA Is Making Incremental Improvements, but Much More Remains to Be Done
Statement of Carol C. Harris, Director, Information Technology and Cybersecurity
Before the Subcommittee on Technology Modernization, Committee on Veterans’ Affairs, House of Representatives
For Release on Delivery Expected at 3:00 p.m. ET
United States Government Accountability Office
View GAO-25-108091. For more information, contact Carol Harris at (202) 512-4456 or HarrisCC@gao.gov.
Highlights of GAO-25-108091, a testimony before the Subcommittee on Technology Modernization, Committee on Veterans' Affairs, House of Representatives
Electronic Health Record Modernization
VA Is Making Incremental Improvements, but Much More Remains to Be Done
Why GAO Did This Study
After three unsuccessful attempts since 2001, VA initiated its fourth effort—the EHRM program—to replace its legacy system. In April 2023, after deploying the new system to five of its medical centers, VA paused deployments due to user concerns. On December 20, 2024, VA announced that it was resuming planned deployments in mid-2026 to four Michigan facilities.
GAO was asked to testify on VA’s EHRM program. GAO summarized the results of its previously issued reports on EHRM and followed up on implementation of its prior recommendations. GAO also summarized the preliminary results of a draft report currently at the agency for comment that addresses, among other things, VA cost estimating and integrated scheduling.
What GAO Recommends
GAO has previously made 15 recommendations on the EHR modernization in issued reports; 14 of the 15 have not yet been implemented. In its draft report, GAO is making three additional recommendations on cost estimating, schedule, and system metrics. Implementing GAO’s recommendations is critical to reducing EHR risks and delivering a quality system within cost and schedule expectations.
What GAO Found
From June 2020 to May 2023, GAO issued four reports on the Department of Veterans Affairs’ (VA) efforts to implement its electronic health record modernization (EHRM) and made a total of 15 recommendations aimed at improving implementation. Among other things, these recommendations addressed poor user satisfaction, the need for better change management, the pace of system trouble ticket resolution, and the importance of addressing independent operational assessment deficiencies.
Most recently, in its draft report currently at VA for comment, GAO’s preliminary results show that VA is making incremental improvements. This includes implementing over 1,500 system configuration changes and initiating projects to address user challenges. However, much more remains to be done:
· As of February 2025, VA had not addressed approximately 1,800 complex configuration change requests.
· The program lacks an updated total life cycle cost estimate that reflects the many EHRM changes and delays. Existing EHRM life cycle cost estimates range from VA’s $16.1 billion to an independent estimate of $49.8 billion. Updating the independent life cycle cost estimate is imperative to understanding the full magnitude of VA’s investment.
· Similarly, it is critically important that VA update its integrated schedule to inform decision-making. Planned system deployment at four additional locations results in about 160 medical centers (94 percent of VA’s total number of medical centers) without the new system as of mid-2026.
· The EHRM program did not identify baselines and targets for one of its nine metrics to measure the impact of the new system at the live sites.
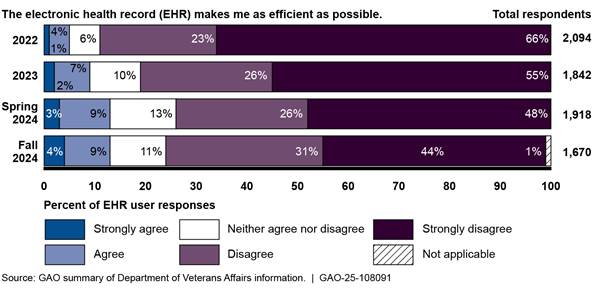
· VA’s 2024 user surveys continue to reflect general dissatisfaction with the new system. (See figure.)
Department of Veterans Affairs User Feedback on Electronic Health Record Enabling Efficiency
An updated cost estimate and integrated schedule are essential management tools to inform VA of the challenges it faces in moving forward.
Chairman Barrett, Ranking Member Budzinski, and Members of the Subcommittee:
Thank you for the opportunity to discuss our work on the challenges that the Department of Veterans Affairs (VA) faces as it works to replaces its legacy electronic health record (EHR) system.[1] As you know, VA depends on its EHR system to manage health care for its patients. Since 2017, the department’s Electronic Health Record Modernization (EHRM) program has undertaken an effort to replace its legacy EHR system with a modernized, commercial system.
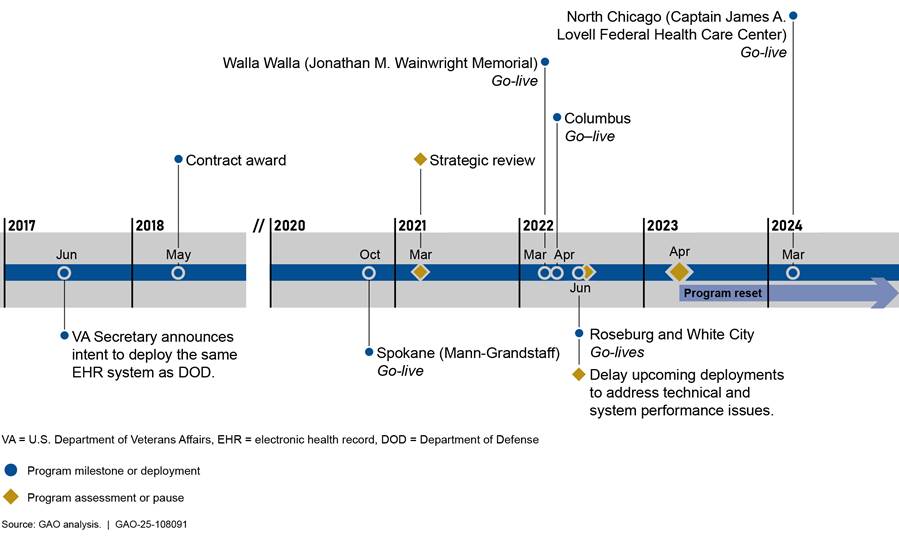
VA first deployed the new EHR system in October 2020 and followed up with further deployments to four additional sites in 2022. In April 2023, VA announced that it planned to halt future deployments to additional sites due to feedback from veterans and clinicians that the new system was not meeting expectations. An exception to this pause was the Captain James A. Lovell Federal Health Care Center in North Chicago that was deployed in March 2024.[2] On December 20, 2024, VA announced that it was resuming planning for future deployments starting with four facilities in Michigan.
We have previously designated VA health care as a high-risk area for the federal government, in part due to its IT challenges and implementation of EHRM.[3] In our 2023 high-risk update, we noted that VA had a number of major modernization initiatives, including the EHR, that faced challenges.
In this statement, I will summarize our prior reports and a draft report that is currently at the agency for comment that describe the challenges in VA’s implementation of the new EHR system and the status of improvements.
In developing this testimony, we summarized challenges identified in our prior reports and in a draft report that is currently at the agency for comment on VA’s efforts to implement its ERHM. We included results from our recent draft report and incorporated information on the department’s actions in response to recommendations we made in our previous reports. The reports cited throughout this statement include detailed information on the scope and methodologies.[4]
The work on which this statement is based was conducted in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
Within VA, the Veterans Health Administration (VHA) operates one of the nation’s largest health care systems. The administration relies on its legacy health information system—the Veterans Health Information Systems and Technology Architecture (VistA)—to deliver health care to veterans and to document this care. This technically complex system has been in operation for more than 30 years, is costly to maintain, and does not optimally support VA’s need to electronically exchange health records with other organizations, such as the Department of Defense (DOD) and community providers (who are non-VA providers that provide care to veterans and are reimbursed by VA).
The department has undertaken, and we have reported on, a number of initiatives to improve interoperability (i.e., the ability to exchange and use electronic health information) and modernize EHRs across the department.[5] These initiatives have included four efforts over two decades to modernize VistA. The first three efforts—HealtheVet, the integrated Electronic Health Record (iEHR), and VistA Evolution—reflect varying approaches that the department had taken since 2001 to achieve a modernized electronic health record system. However, these approaches were abandoned due to concerns about project planning, high costs, and undelivered capabilities.
VA’s current approach, EHRM, began in June 2017. At that time, the former VA Secretary announced that the department planned to acquire the Oracle Health EHR system—the same commercial system that DOD was implementing across the military health system—and configure it for VA.[6] According to the Secretary of VA, the department decided to acquire the same system as DOD because it would allow all of VA’s and DOD’s patient data to reside in one system. A single system is intended to enable seamless care between VA and DOD without the manual and electronic exchange and reconciliation of data between two separate systems.[7]
VA’s EHRM Integration Office manages the EHRM program and coordinates with stakeholders (e.g., VHA subject matter experts and site-specific staff) at the facility, regional, and national levels on the transition to a new EHR system. According to the department, EHRM is designed to improve veterans’ experiences by establishing a modernized, seamless, and secure EHR for VA. This modernization approach is also intended to improve VA health care providers’ ability to deliver care by standardizing clinical practice workflows, enabling interoperability between VA and DOD, and increasing interoperability with community care partners.
The EHRM program originally planned to implement the new EHR system across VA’s health care medical facilities in phases over the span of a decade. VA deployed the new EHR system at its first location, the Mann-Grandstaff VA Medical Center in Spokane, Washington, in October 2020. In 2021, VA performed a strategic review of the program and decided to pause new deployments and focus on fixing initial deployment issues.
In fiscal year 2022, VA moved forward with implementation of the system at four additional locations:[8]
· Jonathan M. Wainwright Memorial VA Medical Center in Walla Walla, Washington, in March 2022.
· VA Central Ohio Health Care System in Columbus, Ohio, in April 2022.
· Roseburg VA Health Care System in Roseburg, Oregon, in June 2022.
· VA Southern Oregon Rehabilitation Center and Clinics in White City, Oregon, in June 2022.
Following the Roseburg and White City deployments, VA decided to delay upcoming deployments to address feedback from users at the initial sites who identified patient safety and system reliability issues. In addition, it performed an assessment to diagnose and address problems with the governance and processes for deployments.
Around the same time, the department modified a task order performance work statement of the EHRM contract to include seven priority enhancements intended to address related feedback from pharmacists and providers.[9] In March 2023, VA released a report from a multidisciplinary, enterprise-wide team that assessed concerns and recommended solutions for the most impactful and critical patient safety issues to be fixed before future deployments (referred to as “Go-live”). As part of the review, VA identified 14 critical patient safety issues requiring development or enhancement work.
In April 2023, VA announced that feedback from veterans and clinicians continued to indicate that the new system was not meeting expectations at the five deployed sites. Consequently, the department halted future deployments, with the exception of the Captain James A. Lovell Federal Health Care Center in North Chicago, to focus on making improvements at the five initial sites. VA refers to its current improvement efforts as a program “reset.”[10] Figure 1 depicts a timeline of key program events.
Figure 1: Department of Veterans Affairs (VA) Electronic Health Record Modernization Program Timeline from 2017-2024
Since the program reset began in April 2023, the department has focused resources on fixing issues identified by users and optimizing the system at the deployed sites. Using an incremental approach, the EHRM Integration Office and VHA have identified goals for planning and executing incremental changes aimed at making improvements rapidly at the live sites. Specifically, VA established the following outcome-oriented reset goals:
· ensure that the new system is working as promised for its end users at the first five sites,
· prepare for and deploy the system at the Captain James A. Lovell Federal Health Care Center in North Chicago, and
· invest in foundational work for successful future deployment of the EHR across the enterprise (e.g., improving processes to manage issues for an enterprise system and workforce development).
While the reset efforts continued, VA deployed the new EHR system at the Captain James A. Lovell Federal Health Care Center in North Chicago, Illinois, in March 2024. On December 20, 2024, VA announced that it was beginning early-stage planning for restarting deployments to four sites in Michigan in mid-2026.
For the period of fiscal year 2018 through the third quarter of fiscal year 2024, VA reported that it obligated a total of about $12.71 billion on EHRM. This total is comprised of the following elements:
· EHR contract ($5.42 billion)
· IT infrastructure ($3.11 billion)
· program management ($1.33 billion)
· VHA ($2.58 billion)
·
Office of Information and Technology (OIT) ($273 million).
GAO Has Reported on VA’s Challenges in Implementing the New EHR
From June 2020 to May 2023, we issued four reports on VA’s efforts to implement its EHRM. In May 2023, we reported that the organizational change management activities for the EHRM program were partially consistent with seven leading practices and not consistent with one leading practice.[11] We also reported that users expressed dissatisfaction with the new system and VA did not adequately identify and address system issues. We made 10 high priority recommendations to address change management, user satisfaction, system trouble ticket, and independent operational assessment deficiencies. VA concurred with the recommendations. As of February 2025, VA has not yet implemented the recommendations. For example:
· VA has not yet developed and implemented a VA-specific change management strategy to formalize its approach to drive user adoption. According to the department, it worked with its contractor to update the contractor’s change management plan to be more VA-specific and stated that VHA and the EHRM program office were collaborating to develop a strategy that was targeted for completion in December 2025.
· VA has not yet adequately demonstrated that it addressed users’ barriers to change by ensuring planned completion of actions identified in a strategic review of the program. VA had plans in place to address the open action items through reset initiatives and key priority projects, but the underlying user barriers have not yet been fully addressed.
· VA has not reinstituted plans to conduct an independent operational assessment to evaluate the suitability and effectiveness of the new EHR system for users in the operational environment. As of November 2024, according to VA officials, funding for the project was not approved and VA could not move forward with the action. However, EHRM program officials said that VA was still able to conduct a variety of independent assessments such as independent end user testing.
Our February 2022 report on VA’s data management plans discussed migrating data to the new EHR system and supporting the continuity of reporting.[12] We noted that VA had made progress towards implementing planned data management activities, but clinicians faced challenges with the quality of migrated data. In addition, VA had not established performance measures and goals for data quality and had not used a stakeholder register to identify and engage all stakeholders. Accordingly, we made two recommendations to VA to (1) establish performance measures and (2) use a stakeholder register to meet reporting needs. VA concurred and took action to fully implement the second recommendation. However, because the program had paused system deployments and lacked a path to migrating data at the next sites, we do not yet have sufficient evidence to demonstrate that the first recommendation has been implemented.
In February 2021, we reported that VA had made progress toward implementing its new system but needed to postpone further deployment until it had addressed all critical and high severity test findings.[13] We made two recommendations that it do so, and VA concurred. As of December 2024, the department had made progress toward implementing the recommendations as it had no critical or high-severity test findings at go-live at the four subsequent locations. There were also no critical or high severity test findings at the joint DOD/VA Captain James A. Lovell Federal Health Care Center go-live. We will plan to consider the recommendations implemented when we have observed sustained resolution of significant test findings.
Our June 2020 report found that VA’s decision-making procedures for configuring the EHR system were generally effective but did not always ensure key stakeholder involvement.[14] We recommended that the department ensure the involvement of all relevant medical facility stakeholders in the EHR system configuration decision process. VA concurred with our recommendation and stated that it intended to refine local workshop agendas and descriptions to facilitate subject matter expert identification and participation. However, the recommendation has not yet been implemented.
In total, our prior reports included 15 recommendations to assist the department in its efforts. While VA has taken steps to address our recommendations such as initiating key priority projects to address user concerns, as of February 2025, VA had fully implemented one of our 15 recommendations. As VA resumes planning activities for future deployments, we will continue to monitor VA’s progress.
VA Had Incrementally Delivered Improvements at the Initial Sites, but Much More Work Remained
Since the EHR deployments were paused and the program reset was announced in April 2023, we stated in our draft report that VA had taken an incremental approach to deliver system improvements. Specifically, our preliminary results indicate that VA made configuration changes to the new EHR system, delivered patient safety and pharmacy enhancements, improved system trouble ticket resolution, and improved system performance for the initial sites.
· Configuration changes. A significant part of VA’s improvement efforts focused on making configuration changes to the EHR baseline.[15] Specifically, the department reported that it implemented more than 1,500 configuration changes that impacted users at the enterprise level, through its standard configuration change process as of June 2024. These changes addressed user needs (i.e., a requested change) or supported enterprise standards (i.e., a change to support a standardized workflow) and were critical for improving performance and usability for staff at the five initial sites. However, as of September 2024, there were about 2,200 complex configuration change requests that had not yet been resolved. Over the course of the reset, VA developed a revised process for addressing configuration change requests with a tiered escalation process for timely and collaborative problem-solving across facilities. As of February 2025, VA had not addressed approximately 1,800 complex configuration change requests.[16]
· Patient safety and pharmacy enhancements. VA had closed many, but not all, of its highest-priority patient safety enhancement requests as identified in the department’s March 2023 assessment of what needed to be fixed before the future deployments resumed.[17] As of July 2024, according to EHRM program officials, VA had closed nine of 14 highest-priority patient safety related enhancement requests. These enhancements were intended to address items most impactful and critical for patient safety. For example, VA reported that it had addressed the patient safety concern that DOD’s system was overwriting VA identity and demographics information. Regarding pharmacy enhancements, VA delivered six of seven pharmacy enhancements identified by pharmacists and providers. However, as of June 2024, VA had not deployed the remaining pharmacy enhancement for synchronization between the system module used by pharmacists and the module used by other health care team members. VA estimated that the pharmacy capability would be delivered with the planned February 2025 system update.
· Ticket resolution. VA’s data on trouble ticket resolution showed that service level agreement requirements for the percentage of tickets that were resolved within timeliness thresholds were met since the implementation of financial consequences (i.e., financial credits from the contractor to the department in the form of an invoice offset) in September 2023. This was an improvement over earlier data that showed consistent challenges with resolving trouble tickets prior to July 2023.
· System outages and incidents. VA established performance requirements as part of its service level agreement with Oracle Health, which defined expectations that the EHR system operate free from incidents or outages for specific amounts of time. If performance requirements are not met monthly, financial consequences (i.e., financial credits from the contractor to the department in the form of an invoice offset) may apply. The outage-free time (system operates greater than 99.95 percent of the time without reported outages) was met for 14 of 16 months from June 2023 to September 2024. The outage-free time requirements were not met in March and April 2024 due to database bugs. From June 2023 to September 2024, incident-free time (system operates 95 percent of time without any reported incidents) was met for 12 of 16 months and not met for 4 of the 16 months.
However, the preliminary results of our draft report show that much more work remained for VA to implement additional configuration changes and enhancements. Specifically, VA had prioritized a number of complex projects that require additional stakeholder input and coordination. For example:
· According to the EHRM program, referral management within the new EHR system lacks functionality and intuitiveness for users. Further, data exchanges related to referrals experience issues that may cause delays in care and frustration among staff. The related priority project is intended to identify improvements by simplifying existing processes and standardizing referrals across the enterprise, by specialty, into streamlined workflows and tools.
· As another example, according to EHRM program officials, VA does not have a consistent strategy for standardizing and streamlining positions within the EHR, resulting in numerous unused, redundant, or overlapping positions. The priority project related to position standardization is intended to consolidate and reduce the number of standardized user positions (i.e., roles) in the system which could, among other things, relieve users from having to log in and log out to perform different position-specific functions.
Further, the program lacks an updated total life cycle cost estimate and integrated master schedule that reflects the many EHRM changes and delays. In January 2019, VA estimated that its life cycle cost for EHRM would total about $16.1 billion consisting of the following:
· The EHRM program contract, awarded in May 2018, was for a maximum of nearly $10 billion over 10 years.
· Expected costs for technology infrastructure readiness and program management support were estimated at $6.1 billion.
In October 2022, the Institute for Defense Analyses issued a final report on an independent cost estimate for the EHRM program. The Institute estimated a total life cycle cost of $49.8 billion—$32.7 billion for a 13-year implementation phase and $17.1 billion for 15 years of sustainment costs.[18]
Regarding the program’s schedule, the Deputy VA Secretary testified in September 2022 before the Senate Appropriations Committee that the full EHR deployment schedule through 2028 was currently under development and would be ready in the fall of 2022. However, this schedule was not released, due, in part, to the deployment pause announced in April 2023. VA’s December 20, 2024, announcement pertained to the four locations in Michigan. VA does not have a deployment schedule for the other approximately 160 VA medical centers and associated clinics.
Following cost estimating and schedule best practices helps minimize the risk of cost overruns and schedule delays for government acquisitions.
· A high-quality, reliable cost estimate is a key tool for budgeting, planning, and managing federal programs. According to federal guidance, generating reliable program cost estimates is a critical function necessary to support the capital programming process.[19] Without this capability, agencies are at risk of experiencing program cost overruns, missed deadlines, and performance shortfalls.
GAO’s Cost Estimating and Assessment Guide describes best practices for developing reliable cost estimates that management can use to make informed decisions.[20] Among other things, it is important to revise cost estimates to reflect program changes and maintain reliable estimates throughout the life of the program. It is also important to have an independent view of the program to help an organization better understand the risks its program faces and better manage them as they are realized.
· The success of a project also depends, in part, on having an integrated and reliable master schedule that defines when and how long work will occur, and how each activity is related to the others. Integrated master schedules are a consolidation of lower-level project (i.e., subproject) schedules. Among other things, an integrated and reliable schedule can show when major events are expected as well as the completion dates for all activities leading up to them, which can help determine if the program’s parameters are realistic and achievable.
We have previously reported in our Schedule Assessment Guide that a reliable schedule can provide a road map for the systematic execution of a program and the means by which to gauge progress, identify and address potential problems, and promote accountability.[21] Following changes in a program, the schedule is used to forecast the effects of delayed, deleted, and added effort, as well as possible avenues for time and cost recovery.
On December 20, 2024, VA announced the decision to restart planning for deploying the new EHR system at four locations in Michigan beginning in mid-2026. In addition, work would continue to make improvements at the initial sites. However, the program did not commit to when it would update the EHRM life cycle cost estimate and integrated master schedule to reflect the changes and lessons learned from the initial deployments and the 20-month deployment pause.
Without updated cost estimates, management and oversight bodies must continue to rely on either the January 2019 VA total life cycle cost estimate of $16.1 billion, or an October 2022 independent cost estimate of $49.8 billion. However, these prior estimates do not reflect the full magnitude and impact of delays, system changes, and updated processes.[22] For example:
· VA’s life cycle cost estimate of $16.1 billion is severely outdated and incomplete. Specifically, it does not encompass the full life cycle of the program through each phase in the program as it estimates only for a 10-year period. It also does not reflect changes that have occurred over the last 6 years.
· The independent cost estimate represents a more realistic assessment of expected costs, but it also does not reflect the pause and other significant changes over the last 2 years. It includes a 15-year sustainment period, reflecting continuing operations and maintenance costs, and uses a more conservative 13-year implementation time frame rather than 10 years.
VA’s announcement that system deployment will occur at four additional sites in mid-2026 means that 8 years after contract award, the new system will be deployed at a total of 10 locations. With 2 years remaining on the contract in mid-2026, VA will have approximately 160 remaining medical centers and associated clinics (94 percent of VA’s total number of medical centers) that will still be using the legacy system.
According to EHRM program officials, VA learned from the program reset. However, we noted that given the volume of changes, delays, and continuing issues, an updated cost estimate is essential to understanding the magnitude of VA’s investment.
Accordingly, in a draft that is currently at the agency for comment, we recommended that VA (1) obtain an updated and independent total life cycle cost estimate using best practices described in GAO’s Cost Estimating and Assessment Guide and (2) expeditiously and reliably update its integrated master schedule using best practices described in GAO’s Schedule Assessment Guide.
Feedback Indicated Improvement, but Dissatisfaction with EHR at Initial Sites Persisted
VA’s user satisfaction surveys indicated improvement since 2022, but about half of respondents continued to disagree or strongly disagree that the system enabled them to deliver high-quality care.[23] For example, in 2022, 5 percent (112 of 2,094) of users responding to the survey agreed or strongly agreed that the system made them as efficient as possible. In September 2024, 13 percent (221 of 1,670) agreed or strongly agreed that the system made them as efficient as possible. However, 75 percent (1,247 of 1,670) disagreed or strongly disagreed that the EHR made them as efficient as possible (see figure 2).
Figure 2: Department of Veterans Affairs User Feedback on Electronic Health Record Enabling Efficiency
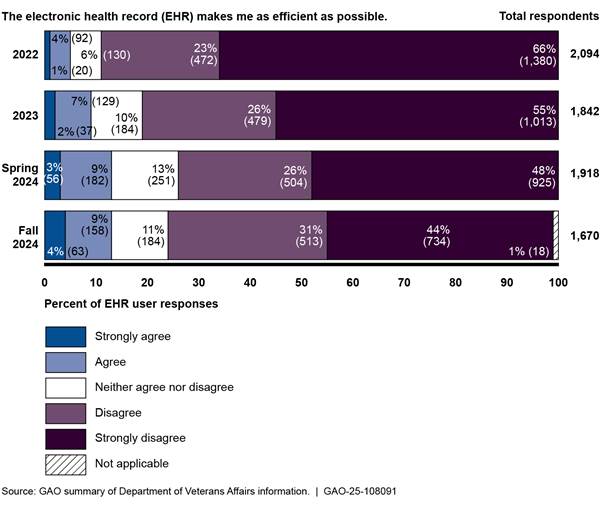
Note: The VA user surveys were conducted in September
2022, August-September 2023, March-April 2024, and September 2024.
Similar to VA’s survey results, most users we interviewed said that the system generally decreased productivity. Specifically, 54 of 71 reported that the EHR decreased or greatly decreased productivity, 14 of 71 reported that it neither increased nor decreased productivity, and one of 71 respondents said that it had increased productivity (see table 1).[24]
Table 1: Feedback from Selected Users on the Effect of the Department of Veterans Affairs’ New Electronic Health Record (EHR) System on Productivity
|
|
How has the new EHR system affected your productivity? |
|
Greatly increased productivity |
0 |
|
Increased productivity |
1 |
|
Neither increased nor decreased productivity |
14 |
|
Decreased productivity |
30 |
|
Greatly decreased productivity |
24 |
|
No basis to judge |
2 |
|
Total |
71 |
Source: GAO analysis of interviews with Department of Veterans Affairs officials. | GAO‑25‑108091
With respect to how the new EHR system had affected their productivity, the users we interviewed also provided examples of their concerns. These examples discussed anecdotal experiences with reductions in the amounts of patients that could be seen daily, needs for additional staff, and a backlog of referrals. On several occasions, users discussed their frustration with the increase in the number of steps required to complete actions in the system.
VA Had Begun Monitoring Performance Measures but Had Not Fully Defined Targets
According to federal guidance, performance measures allow the program the ability to measure and communicate the benefits intended and achieved by the program.[25] Leading practices for performance measures include:
· developing measurable outcome-based goals;
· identifying and documenting metrics to measure outcomes of the program against goals; a range of indicators is important because most program activities require managers to balance their priorities and programs may seek to measure areas such as organizational efficiency and customer (user) satisfaction;
· establishing baseline measures to serve as a comparison for current performance metrics and define success targets expected to be achieved by the program; and
· monitoring performance and report objective results to inform decisions, identify areas for process improvement, and take appropriate corrective action.
The preliminary results of our draft report show that VA identified performance measures for the new EHR reset in accordance with federal guidance. Specifically, VA developed four categories for outcome-based goals for reset success. They are to:
· improve end user and veteran experience,
· improve health system operations,
· sustain high performance and high reliability of the system, and
· mature program processes.
Further, VA identified and documented nine focus metrics aligned to the goal categories to measure and track progress over time. These metrics were selected from existing data. These metrics are:
· percentage of staff who agreed that the EHR provides them with the ability to provide quality care,
· time in EHR per patient seen for primary care/family medicine specialties,
· sites projected patient workload as a percentage of the veterans integrated services network patient weighted workload for performance based funding allotments,[26]
· percent total collections to expected results,
· productivity work relative value units for clinical full-time equivalents,
· incident-free time,
· number of crashes a user experiences,
· time to user-acknowledged incident ticket resolution in days, and
· time to user-acknowledged change request ticket resolution in days.
The EHRM program identified baselines and targets for eight of nine metrics to measure the impact of the new system at the live sites. However, VA had not established baselines and targets for one metric: the time to user-acknowledged ticket resolution for change requests. According to EHRM program officials, VA had not fully defined the baselines and targets for its metrics because it recently implemented a revised process for addressing configuration change requests at the end of August 2024.
In September 2024, VA began to measure and report on progress toward targets. Specifically, the EHRM program reported meeting its targets for four of the eight metrics for which it had established targets. For example, VA had met its target for the time spent in the EHR per patient seen for primary care or family medicine, patient weighted workload for performance based funding allotments, incident-free time, and user interruptions. However, VA had not yet met its targets for percentage of staff who agree that the EHR provides them with the ability to provide quality care, collected income, productivity, and time to user acknowledged ticket resolution metrics for tickets and change requests. Metrics are an important set of tools for the department to determine program and system improvements. Establishing all nine of the baselines and targets will provide VA management with complete information on program performance.
Accordingly, in our draft report, we are recommending that VA identify baselines and performance targets for all nine identified metrics intended to measure program and system performance.
In conclusion, the challenges facing VA’s EHRM have resulted in delays in delivering improvements to the system. While the department has indicated its readiness to plan for future deployments, it has not provided updated information on how long it will take to complete the modernization nor reliable estimates for how much it will cost. There is also much work to be done to demonstrate that our prior recommendations have been addressed and that improvements made to date are enough to reduce program risks and ensure that VA is delivering a quality system.
Further, in our draft report that is currently at the agency for comment, we stated that VA was working to improve the system and address concerns from the five initial sites as it emerged from a 20-month deployment pause. However, VA has not updated its total life cycle cost estimate and integrated master schedule to reflect the reality of the program and the impact of delays, system changes, and updated processes. VA also has not finalized one baseline and target for its metrics, which can provide department leadership with important information of program performance. We plan to make three additional recommendations regarding these issues. Implementing our prior 15 recommendations as well as the three planned recommendations is critical to VA reducing program risks and delivering a quality system.
Chairman Barrett, Ranking Member Budzinski, and Members of the Subcommittee, this concludes my prepared statement. I would be happy to answer any questions that you may have at this time.
GAO Contact and Staff Acknowledgments
If you or your staff have any questions about this testimony, please contact Carol C. Harris at (202) 512-4456 or harriscc@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this statement.
GAO staff who made key contributions to this testimony include Jennifer Stavros-Turner (Assistant Director), Merry Woo (Analyst-in-Charge), John Bornmann, Chris Businsky, Quintin Dorsey, Rebecca Eyler, Anthony Gray, Anh-Thi Le, Jacqueline Mai, Sachin Mirajkar, Monica Perez-Nelson, Scott Pettis, Frances Tirado, Walter Vance, and Geoffrey Zhang.
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, X, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]An EHR is a collection of information about the health of an individual or the care provided, such as patient demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports.
[2]The Captain James A. Lovell Federal Health Care Center in North Chicago is the only fully integrated health care system operated by both VA and the Department of Defense (DOD).
[3]VA’s IT issues were highlighted in our 2015 high-risk report and subsequent high-risk reports. See GAO, High-Risk Series: An Update, GAO‑15‑290 (Washington, D.C.: Feb. 11, 2015); High-Risk Series: Progress on Many High-Risk Areas, While Substantial Efforts Needed on Others, GAO‑17‑317 (Washington, D.C.: Feb. 15, 2017); High-Risk Series: Substantial Efforts Needed to Achieve Greater Progress on High-Risk Areas, GAO‑19‑157SP (Washington, D.C.: Mar. 6, 2019); High-Risk Series: Dedicated Leadership Needed to Address Limited Progress in Most High-Risk Areas, GAO‑21‑119SP (Washington, D.C.: Mar. 2, 2021); and High-Risk Series: Efforts Made to Achieve Progress Need to Be Maintained and Expanded to Fully Address All Areas, GAO‑23‑106203 (Washington, D.C.: Apr. 20, 2023).
[4]GAO, Electronic Health Records: Ongoing Stakeholder Involvement Needed in the Department of Veterans Affairs’ Modernization Effort, GAO‑20‑473 (Washington, D.C.: June 5, 2020); Electronic Health Records: VA Has Made Progress in Preparing for New System, but Subsequent Test Findings Will Need to Be Addressed, GAO‑21‑224 (Washington, D.C.: Feb. 11, 2021); Electronic Health Records: VA Needs to Address Data Management Challenges for New System, GAO‑22‑103718 (Washington, D.C.: Feb. 1, 2022); and Electronic Health Records: VA Needs to Address Management Challenges with New System, GAO‑23‑106731 (Washington, D.C.: May 18, 2023).
[5]See, for example, GAO‑23‑106731; GAO‑22‑103718; GAO‑21‑224; GAO‑20‑473; Electronic Health Records: VA Needs to Identify and Report System Costs, GAO‑19‑125 (Washington, D.C.: July 25, 2019); VA Health IT Modernization: Historical Perspective on Prior Contracts and Update on Plans for New Initiative, GAO‑18‑208 (Washington, D.C.: Jan. 18, 2018); and Electronic Health Records: Outcome-Oriented Metrics and Goals Needed to Gauge DOD’s and VA’s Progress in Achieving Interoperability, GAO‑15‑530 (Washington, D.C.: Aug. 13, 2015).
[6]VA and DOD use the same Oracle Health Millennium system with agency-specific configuration differences. VA refers to its EHR system as the Federal EHR, while DOD refers to its system as Military Health System (MHS) GENESIS. VA contracted with Cerner Government Services, Inc. for the department’s new EHR system in May 2018. Subsequently, in June 2022, Cerner was acquired by Oracle Health Government Services, Inc. We use Oracle Health throughout this report.
[7]DOD’s initial implementation of MHS GENESIS began in 2017 at four military treatment centers in the state of Washington. The department completed the last of its deployments of the EHR system in March 2024.
[8]VHA is divided into areas called Veterans Integrated Services Networks (VISNs). There are currently 18 VISNs throughout VHA based on geographical location. VISNs provide oversight and guidance to the VA Medical Centers and VA Health Care Systems within their areas and are sometimes called a “network.” The five initial sites are within VHA’s VISN 20 and VISN 10. VISN 20 includes medical centers and community-based outpatient clinics in the states of Alaska, Washington, Oregon, most of Idaho, and one county each in Montana and California. VISN 10 serves veterans in the Ohio, Indiana, and Michigan areas.
[9]An IT enhancement is any change or modification of an IT solution or service to notably improve capabilities or performance beyond the original implementation through additional functionalities, major error and bug repairs, greater processing speed, or better cross-platform compatibility.
[10]The Captain James A. Lovell Federal Health Care Center in North Chicago, Illinois, integrates services previously provided by the former North Chicago VA Medical Center and its community-based outpatient clinics and the Naval Health Clinic Great Lakes and its associated clinics. The Federal Health Care Center provides health care to service members, veterans and other beneficiaries throughout northern Illinois and southeastern Wisconsin. Additionally, the Federal Health Care Center ensures that Navy recruits who pass through Naval Station Great Lakes each year are medically ready. The Federal Health Care Center is part of VISN 12, the VA Great Lakes Health Care System, which serves veterans who reside in Illinois, the Upper Peninsula of Michigan, Wisconsin, and northwestern Indiana.
[11]GAO, Electronic Health Records: VA Needs to Address Management Challenges with New System, GAO‑23‑106731 (Washington, D.C.: May 18, 2023).
[12]GAO, Electronic Health Records: VA Needs to Address Data Management Challenges for New System, GAO‑22‑103718 (Washington, D.C.: Feb. 1, 2022).
[13]GAO, Electronic Health Records: VA Has Made Progress in Preparing for New System, but Subsequent Test Findings Will Need to Be Addressed, GAO‑21‑224 (Washington, D.C.: Feb. 11, 2021).
[14]GAO, Electronic Health Records: Ongoing Stakeholder Involvement Needed in the Department of Veterans Affairs’ Modernization Effort, GAO‑20‑473 (Washington, D.C.: June 5, 2020).
[15]The EHR baseline consists of the commercial software solution operating within the federal environment. Design configuration decisions include determining the data that need to be incorporated into the EHR system. These configurations set up the EHR system to support the work processes that VA clinicians and staff follow in delivering care.
[16]According to EHRM program officials, there are about 600 new configuration change requests per month.
[17]Department of Veterans Affairs, Veterans Health Administration, EHRM Sprint Report (March 2023).
[18]According to EHRM program officials, the original VA cost estimate was based on an assumption that the first few deployments to the system for initial operating capability would be more expensive, and as the department progressed towards full-rate production, there would be economies of scale, thus reducing costs. VA officials said that once a revised deployment schedule was developed, the department had plans to develop an updated cost estimate.
[19]Office of Management and Budget, Preparation, Submission, and Execution of the Budget, Circular No. A-11 (Washington, D.C.: July 25, 2024); Managing Information as a Strategic Resource, Circular No. A-130 Revised (Washington, D.C.: Executive Office of the President, July 28, 2016); and Capital Programming Guide v. 3.1: Planning, Budgeting, and Acquisition of Capital Assets, Supplement to Circular A-11 (Washington, D.C.: July 25, 2024).
[20]GAO, Cost Estimating and Assessment Guide: Best Practices for Developing and Managing Program Costs, GAO‑20‑195G (Washington, D.C.: Mar. 12, 2020).
[21]GAO, GAO Schedule Assessment Guide: Best Practices for Project Schedules, GAO‑16‑89G (Washington, D.C.: Dec. 22, 2015).
[22]The VA Office of Inspector General previously reported on the differences in cost estimates from $16 billion to almost $50 billion. The VA Office of Inspector General reported that the EHRM Integration Office, which is responsible for preparing VA to deploy the EHR system, was working on updating the program cost estimate as of June 2024. See, VA Office of Inspector General, VA Needs to Strengthen Controls to Address Electronic Health Record System Major Performance Incidents, 22-03591-231 (Washington, D.C.: Sept. 23, 2024).
[23]In 2022, VA surveyed users of the new EHR system from Veterans Integrated Services Networks (VISN) 10 and 20 and about 20 percent (2,102 of 10,400) of recipients responded to the survey. In 2023, VA surveyed users from VISNs 10 and 20 and about 26 percent (1,845 of 7,072) of recipients responded to the survey. The March-April 2024 EHR User Experience Survey included provisioned Federal EHR users from five live sites and remote service providers and did not include users from the joint DOD/VA Captain James A. Lovell Federal Health Care Center. About 25 percent (2,081 of 8,289) responded to the survey. The September 2024 User Experience Survey included provisioned EHR users from five live sites, and remote service providers and did not include users from the joint DOD/VA Captain James A. Lovell Federal Health Care Center. About 19 percent (1,871 of 9,747) responded to the survey.
[24]Two users responded that they had no basis to judge.
[25]Office of Management and Budget, Preparation, Submission, and Execution of the Budget, Circular A-11, Part 6: The Federal Performance Framework For Improving Program And Service Delivery (Washington, D.C.: July 25, 2024); General Services Administration, Modernization and Migration Management (M3) Playbook, accessed Aug. 7, 2023, https://www.ussm.gov/m3.
[26]VA uses a measure called the patient-weighted work to measure workload and account for factors such as patient volume, case-mix, and specialized services.
