VETERANS HEALTH CARE
Opportunities to Improve Access to Care Through the Veterans Community Care Program
Statement of Sharon M. Silas, Director, Health Care
Before the Subcommittee on Health, Committee on Veterans’ Affairs, House of Representatives
For Release on Delivery Expected at 2:15 p.m. ET
United States Government Accountability Office
View GAO-25-108101. For more information, contact Sharon M. Silas at (202) 512-7114 or SilasS@gao.gov.
Highlights of GAO-25-108101, a testimony before the Subcommittee on Health, Committee on Veterans’ Affairs, House of Representatives
Opportunities to Improve Access to Care Through the Veterans Community Care Program
Why GAO Did This Study
VHA operates one of the largest health care delivery systems in the U.S. It provides health care to more than 6 million veterans. The majority of veterans receive care in VHA-operated medical facilities. However, the number of veterans receiving care from community health care providers has increased from about 1.1 million in 2014 to about 2.8 million in 2023, according to VA.
This statement focuses on VA’s efforts to ensure that veterans have access to high-quality health care, particularly through community providers. It also discusses opportunities GAO has identified to improve VA operations. This statement is based on seven GAO reports that were issued between 2018 and 2025. See GAO-18-281, GAO-20-643, GAO-23-105290, GAO-23-105617, GAO-24-106410, GAO-24-106390, and GAO-25-106678. This statement also includes updated information on the status of GAO’s recommendations made in those reports.
What GAO Recommends
GAO has made 27 recommendations to VHA to address challenges related to aspects of the Veterans Community Care Program in the reports covered in this statement. VA has implemented 9 of these recommendations. VA has taken steps to address the remaining 17 but has not fully implemented them as of February 2025. GAO closed one recommendation as not implemented because it was no longer valid given changes in VA. Fully implementing all the recommendations would help ensure VHA can provide veterans timely access to care.
What GAO Found
In the last decade, Congress has taken steps to expand the ability of eligible veterans to receive care from community health care providers. In particular, the VA MISSION Act of 2018 established the current Veterans Community Care Program. The increased use of community care through this program is a major change for the Department of Veterans Affairs (VA).
GAO has identified challenges and made 27 recommendations related to the Veterans Community Care Program regarding (1) scheduling and wait times and (2) VA oversight of the contractors used to implement the program, including provider network adequacy. VA has implemented 9 of these recommendations and taken steps to implement others.
Scheduling and wait times. VA considers a key component of access to be the time it takes veterans to receive care at Veterans Health Administration (VHA) facilities or in the community.
· In a June 2018 report, GAO recommended that VA establish a community care scheduling process with time frames within which veterans’ (1) referrals must be processed, (2) appointments must be scheduled, and (3) appointments must occur. Although VA concurred with this recommendation and implemented the first two components, it has not established standard time frames within which appointments must occur. Thus, this recommendation has not been fully implemented.
· In January 2025, GAO found that VHA’s Referral Coordination Initiative—intended to improve scheduling timeliness and veterans’ experiences—needs improved program direction and guidance. VHA officials acknowledged that implementation of the initiative had been inconsistent. GAO recommended that VHA ensure program direction—specifically strategic goals, standards for consistent implementation, roles and responsibilities, and oversight and accountability—is documented in national policy and guidance. VA concurred in principle with this recommendation.
Contract oversight and network adequacy. VHA’s Office of Integrated External Networks leads, develops, and oversees community care contracts and networks for veterans.
· In a November 2022 report, GAO found that VA needed to strengthen its oversight and improve data on its community care network providers and made two recommendations accordingly. VA has implemented both of these recommendations.
· In an August 2024 report, GAO found weaknesses in VA’s oversight of the community care contracts. For example, the office responsible for contract oversight had not developed a clear and complete set of documents to guide oversight, among other concerns. GAO made three recommendations to address these findings. VA concurred with these recommendations and described planned actions to address them, which GAO will evaluate during the recommendation follow-up process.
February 12, 2025
Chairwoman Miller-Meeks, Ranking Member Brownley, and Members of the Subcommittee:
I appreciate the opportunity to be here today to discuss the Department of Veterans Affairs’ (VA) efforts to ensure veterans have timely access to health care, particularly care provided through private health care providers in the community. VA has a long history of using community providers under various programs—including the current Veterans Community Care Program—as a way to address veterans’ challenges accessing care at VA’s Veterans Health Administration (VHA) medical facilities.[1] In the last decade, Congress has taken steps to improve veterans’ access to care, including expanding the ability for eligible veterans to receive care from community providers when they face challenges accessing care at VHA medical facilities.[2] In particular, the VA MISSION Act of 2018 made community care a more central part of how VA accomplishes its mission.[3] However, the increased role of community care is a major change for VA as an organization.
Although the majority of veterans utilizing health care services delivered by VA still receive care in VHA-operated medical facilities, the number of veterans receiving care through the Veterans Community Care Program has increased. According to VA, the number of veterans who received services through community care increased from about 1.1 million in 2014 to about 2.8 million in 2023. VA documentation shows that community care represented about 40 percent of all VA health care in fiscal year 2023. According to VHA, the department spent about $26.7 billion on this care in this same year, out of the total $128.6 billion appropriated for all of VA health care.
For nearly 25 years, we have reported on the challenges VA has faced providing health care services in a timely manner. We have issued reports recommending that VHA improve appointment scheduling, ensure the reliability of wait time and other performance data, and improve oversight. Due, in part, to issues in VA’s ability to ensure consistent and timely access to health care, GAO added VA health care to GAO’s High-Risk List in 2015.[4]
My statement today summarizes the recommendations we have made to improve VA’s Veterans Community Care Program and the status of VA’s efforts to implement them. This statement is based on a body of work from June 2018, when the Veterans Community Care Program was being planned, through January 2025. Specifically, this statement includes information from seven reports with 27 recommendations to VA during this time period. VA has fully implemented 9 recommendations and taken some steps to address others, 17 of which remain open as of February 2025.[5]
More detailed information on the scope and methodology of our prior work can be found within the specific reports on which this statement is based. These reports are listed in the related products page at the end of this statement. This statement also includes preliminary observations from our ongoing work examining VHA’s efforts to coordinate with community care providers on medical documentation exchange for veterans receiving behavioral health services. For this work, we analyzed VA data on recent behavioral health referrals and VHA guidance on medical documentation exchange, and interviewed VHA officials and others.
We conducted the work on which this statement is based in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
VHA operates one of the largest health care delivery systems in the nation, serving over 6 million veterans. VHA’s system is organized into 18 regional networks known as Veterans Integrated Service Networks (VISN) that manage the day-to-day functions of VHA’s medical facilities, including outpatient facilities. VHA headquarters, its regional network of VISNs, and VHA medical facilities all play a role in managing referrals and scheduling veterans’ appointments for care in a timely manner at VHA medical facilities and in the community. For example, each VISN is responsible for overseeing policy implementation and the performance of the VHA facilities within its network.
VHA Appointment Scheduling
Access to timely medical appointments is critical to ensuring that veterans obtain needed medical care. In particular, access to timely primary care appointments is essential as a gateway to obtaining other health care services such as specialty care. There are three ways to initiate a request for health care once a veteran is enrolled in VHA:
(1) A veteran-initiated appointment request
(2) A provider request for a follow-up appointment with the veteran
(3) A provider referral of the veteran to a specialty care appointment
For a veteran to receive a specialty care appointment, a VHA provider must initiate a request by submitting a referral.[6] Clinical staff (e.g., providers and nurses) and administrative staff (e.g., schedulers) at the VHA facility review the referral and consider eligibility for community care. Then, depending on whether the veteran is eligible for community care and the veteran’s scheduling preferences, facility staff will schedule an appointment either with a provider at a VHA medical facility or with a provider in the community.[7]
In 2019, VHA updated its process for scheduling specialty care appointments, shortly after implementation of the VA MISSION Act. Under this process, called the Referral Coordination Initiative, referral coordination teams at VHA medical facilities review referrals for specialty care and discuss care options with veterans. The implementation of the initiative marked a significant change to the process previously followed by VHA medical facility staff for management of specialty care referrals.
According to VHA guidance, the initiative is intended to
· create dedicated referral coordination teams that are focused on sharing with veterans their health care options,
· empower veterans to make the health care choice that is right for them, and
· improve scheduling timeliness.
The revised referral process is handled by facility referral coordination teams that include designated clinical and administrative staff who assist with scheduling and are trained to discuss veterans’ options for care at the time of scheduling. The process is intended to ensure that referral documentation is complete and includes all pertinent clinical information before the coordination teams discuss care options with veterans and schedule appointments in VHA medical facilities or with community providers. Prior to implementation of the revised process, if a veteran met community care eligibility criteria, the referral for specialty care could be sent directly to community care staff for scheduling. However, the veteran might not be informed of their options to obtain care in a VHA medical facility. In implementing the initiative, VHA—specifically, its Office of Integrated Veteran Care—provided facilities with guidance describing the different ways to structure their referral coordination teams, but gave facilities flexibility to determine what worked best for their circumstances.[8] See figure 1 for an overview of the initiative’s scheduling process.
Figure 1: VHA Referral Coordination Initiative Specialty Care Appointment Scheduling Process
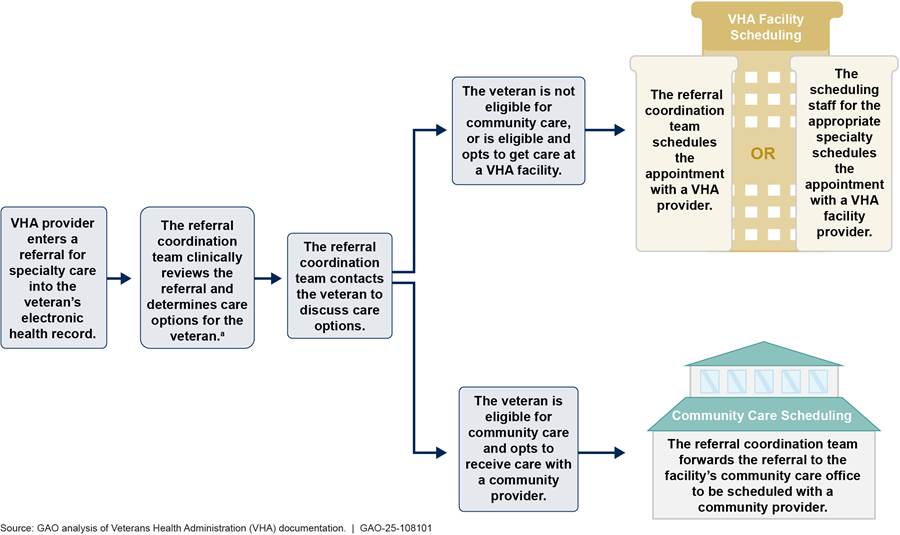
aThis step includes determining whether the
veteran is eligible for community care. If the referral coordination team
contacts the veteran to gather missing clinical information, they are to
discuss care options with the veteran at that time.
Community Care Eligibility
When VHA staff review a referral to schedule an appointment, there are six criteria that can qualify a veteran to receive care under the Veterans Community Care Program.[9] For example, veterans may qualify for community care when the needed services are not offered at a VHA facility or if VHA cannot provide care within its designated access standards. VHA’s designated access standards specify that a veteran may be eligible for community care if
· the average drive time to a VHA provider (from the veteran’s residence) is more than 30 minutes for primary care or more than 60 minutes for specialty care, or
· the first next available appointment with a VHA provider is not available within 20 days for primary care or 28 days for specialty care based on the date from the request for care unless a later date has been agreed upon.[10]
Community Care Contracts and Network Adequacy
VA implements the Veterans Community Care Program through five contracts with third-party administrators—with each contract covering services in one of the five community care regions. (See fig. 2.) The third-party administrators are contractors that are responsible for maintaining provider networks that are both adequate in size and have the capacity to ensure veterans’ timely access to care. The organizational structures, policies, and processes needed to effectively oversee care provided through contracts with third-party administrators are different from those required to manage care provided directly by VHA staff.
Figure 2: Map of VA’s Five Community Care Network Regions
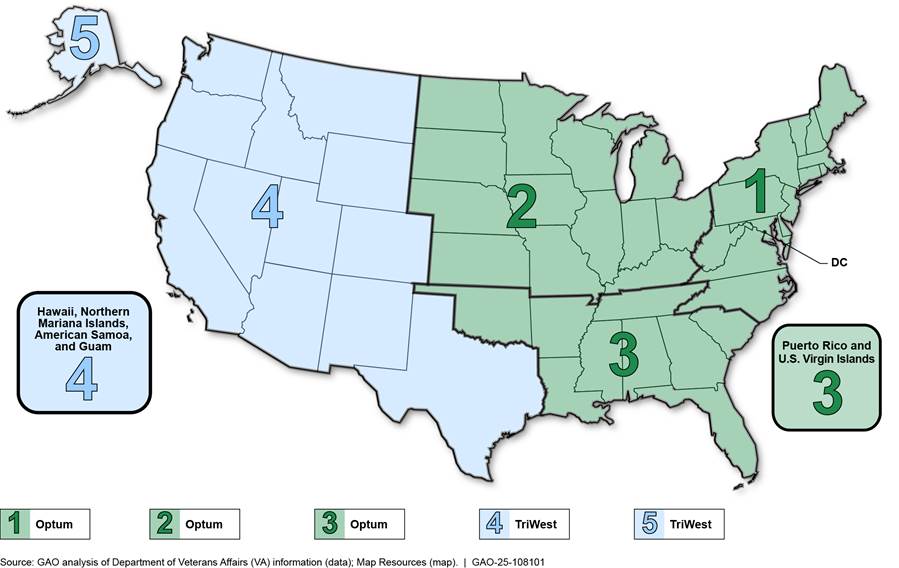
In December 2018, VA awarded community care contracts for regions 1, 2, and 3
to Optum Public Sector Solutions, Inc. In 2019 and 2020, VA awarded community
care contracts for regions 4 and 5 to TriWest Healthcare Alliance Corp. Each of
the contracts was awarded with an initial base period of performance and seven
12-month option periods, the last of which would conclude between 2026 and
2028, depending on the region. Although the work performed under the five
contracts is generally the same, there are some variations in contract terms
across the contracts, and each regional contract is administered separately.
The two contractors are responsible for establishing and maintaining networks of licensed health care community providers and practitioners across their respective regions, including hospitals, physician group practices, and individual physicians, and paying community provider claims. Services provided include primary care and specialty care, such as cardiology and gastroenterology. VHA’s Office of Integrated Veteran Care oversees the two contractors, including the adequacy of the five regional networks to provide veterans with sufficient access to care. In each community care contract, network adequacy is measured using two primary standards: (1) geographic accessibility based on drive time and (2) appointment availability. Both network adequacy standards vary by the category of care (e.g., primary or specialty care).
VHA Could Make Further Improvements to the Veterans Community Care Program by Fully Implementing GAO Recommendations
In reports issued from June 2018 through January 2025, we have made 27 recommendations related to the Veterans Community Care Program, which are intended to support VA in improving veterans’ access to care. In particular we have made recommendations to strengthen (1) community care appointment scheduling processes and monitoring of wait times and (2) oversight of the community care contracts and provider network adequacy.[11] As of February 2025, VA has implemented 9 of these recommendations and taken steps to implement others. (See appendix I for additional information on recommendations we have made regarding VA’s Veterans Community Care Program.)
Scheduling and wait times. VA considers a key component of access to be the time it takes veterans to receive care at VHA facilities and in the community. To this end, VA monitors certain wait times veterans experience, including the amount of time it takes for an appointment to be scheduled both with VHA providers and with community providers. Since 2018, we have made 21 recommendations for VA to improve its appointment scheduling processes and monitoring of wait times for community care. Among these, we recommended that VA establish timeliness standards (a time frame within which a veteran’s appointment should occur) and metrics to measure whether VA is meeting those standards.
VA has taken actions to address some of the 21 recommendations, and we have closed seven recommendations as fully implemented.[12] For example, in 2018, we recommended that VA establish a mechanism that would allow for systematic monitoring of the average number of days it takes to schedule community care appointments.[13] We closed this recommendation as fully implemented in October 2021, based on VA’s development and deployment of a data system that can monitor various time frames in the referral lifecycle.
In contrast, five of our early recommendations directed at the basic tenets of the Veterans Community Care Program remain open, including:
· In our June 2018 report on the prior community care program—Veterans Choice Program—we identified lessons learned that could be considered for the Veterans Community Care Program.[14] Specifically, we recommended that VA establish a community care scheduling process with time frames within which veterans’ (1) referrals must be processed, (2) appointments must be scheduled, and (3) appointments must occur. VA concurred with this recommendation. Although VA implemented the first two components of our recommendation, the department has not established a timeliness standard within which veterans’ appointments must occur. As a result, our recommendation related to community care appointments has not yet been fully implemented as of February 2025.
· In 2020, we made a recommendation related to the one we made in June 2018, that VA align its monitoring metrics with its time frames established for scheduling community care appointments to effectively monitor the extent to which veterans receive care within such specified time frames.[15] VA did not agree with our recommendation at the time of our report but has since taken some steps to address it. We continue to believe that correcting deficiencies in VA’s alignment of its monitoring metrics and establishing a performance metric to measure wait times for the receipt of community care will permit VA to more effectively monitor the timeliness of veterans receiving care regardless of whether the care is received at a VHA facility or in the community.
More recently, we have made eight additional recommendations to VA on its ongoing efforts to improve scheduling and reduce veteran wait times, all of which remain open, including:
· In a January 2023 report, we found that VHA appointment scheduling data indicated that most VHA medical facilities did not meet the timeliness standard for scheduling community care appointments.[16] We further reported that this standard was developed and implemented based on data from a limited number of VHA medical facilities, potentially limiting its utility. VHA did not have a clear rationale for setting the standard at 7 days, and officials were unable to provide documentation that explained the basis for the standard. We recommended that VHA conduct a comprehensive analysis of appointment scheduling data from all VHA medical facilities to determine whether the community care timeliness standards are achievable and revise them as necessary.
VA agreed with this recommendation and has taken some steps to address it. In May 2023, VA officials reported that VA had conducted an analysis of community care scheduling timeliness standards to determine whether these standards were achievable. Consistent with our finding, VA’s analysis showed that most VHA facilities were not achieving the current timeliness standard of scheduling appointments within 7 days of the relevant file entry dates. Subsequently, in June and November 2024, VA reported that VHA leadership is in the process of re-evaluating the 7-day community care referral scheduling metric and considering a proposed change. Once VHA leadership makes a final decision, we will evaluate whether our recommendation has been implemented.
· In June 2024, we recommended VA systematically capture the reasons for community care appointment scheduling challenges and use the information to address those challenges.[17] VA concurred in principle with this recommendation and said that it had put in place mechanisms to track such challenges. VA officials also stated that they plan to conduct an analysis of scheduling challenges based on data obtained through these mechanisms. We will evaluate whether these actions address the intent of our recommendation.
· In January 2025, we found that VHA’s Referral Coordination Initiative needs improved program direction and guidance.[18] VHA began implementing this program aimed at streamlining scheduling for specialty care appointments at its medical facilities across the country in 2019. In our survey of VHA medical facility officials responsible for implementing this initiative, facility officials reported implementation difficulties. Specifically, 80 percent (103 of 129 responses) of officials from facilities that implemented the Referral Coordination Initiative somewhat or strongly agreed that the process had been challenging to implement. Some VHA medical facility and VISN officials noted challenges they experienced due to the lack of clear policy for the initiative, and VHA officials acknowledged that implementation of the initiative had been inconsistent.
Given the transformative potential of this process change as it continues implementation across the VHA health care system, particularly the increased focus on communication with veterans about their care options, we recommended that VA make improvements to its program direction and guidance for this initiative. In particular, we recommended that VHA ensure key aspects of program direction—specifically strategic goals, standards for consistent implementation, roles and responsibilities, and oversight and accountability—are documented in national policy and guidance. Doing so would help VHA medical facilities provide veterans with a consistent appointment scheduling experience across VHA’s health care system. Moreover, we recommended VHA ensure it aligns performance metrics for this initiative with the defined strategic goals and communicate how to use these metrics.
VA concurred with four of our five recommendations and concurred in principle with the recommendation to include program direction in national policy. VHA published a new national referral management policy—which includes some information regarding the Referral Coordination Initiative—on November 22, 2024. We will review this new policy, and the extent to which it fulfills the intent of our recommendation, as part of our recommendation follow-up process.
Contract oversight and network adequacy. Within VHA’s Office of Integrated Veteran Care, the Office of Integrated External Networks leads, develops, and oversees contracts and their networks of providers for the Veterans Community Care Program to ensure high quality and timely health care services for veterans. As part of its oversight, the office (1) measures the contractors’ performance compared with contract terms, including provider network adequacy, (2) manages the reporting of quality issues, (3) oversees the credentialing of network providers, and (4) manages the resolution of disputes, complaints, and grievances. We have made six recommendations in this area, and VA has implemented two of them. Specifically, in a November 2022 report, we made two recommendations for VA to strengthen its oversight and improve data on its community care network providers.[19] VA took actions in response to our recommendations, which we closed as implemented in fall 2024.
We made other recommendations related to the community care contracts. VA concurred with these recommendations but not yet implemented them as of February 2025.
· In an August 2024 report, we found weaknesses in VA’s oversight of the Veterans Community Care Program contracts.[20] For example, we found that the office responsible for contract oversight has not developed a clear and complete set of documents to guide oversight, among other concerns. Likewise, while VHA officials have begun discussing how to address oversight challenges with the current contracts, we found that VA does not have a formal process for documenting lessons learned. We made three recommendations to address our findings. VA concurred with our recommendations and described planned actions to address them. We expect to receive updates from VA on these actions later this month, and will assess the extent to which the actions meet the intent of our recommendations.
· In June 2024, we reported on opportunities we identified for potential improvements to ensure network adequacy for the community care networks.[21] VA assesses community care contractors’ network adequacy performance against two primary standards: drive time and appointment availability. VA’s methodology to calculate specialty care network adequacy—specifically, excluding certain claims when they do not meet the standard and including them when they do—poses a risk to VA’s ability to fully assess the extent to which community care networks are adequate to meet veterans’ needs, including for mental health care. As VA begins to develop the next generation of community care contracts, it is important for VA to understand the risks associated with its existing methodology, and whether an alternative approach might be warranted. We recommended that VA assess the risks associated with its methodology for calculating specialty care network adequacy and revise its approach accordingly. VA concurred with this recommendation and described planned actions to address it by early 2025. We will continue to monitor VA’s progress in implementing this recommendation.
We also have ongoing work related to other aspects of community care—specifically, examining the various information technology systems involved in scheduling and related operations, and examining VHA’s efforts to coordinate care with community providers.
· Scheduling systems. We have ongoing work examining the systems VA uses to schedule appointments and monitor wait times and any challenges VHA facilities and veterans experience using these systems, among other questions. These systems include those related to determining community care eligibility and managing community care referrals. To do this work, we have reviewed VA documents, interviewed VA officials, and conducted site visits with VHA medical facilities. We anticipate issuing our report in late spring 2025.
· Care coordination. We also have ongoing work examining VHA’s efforts to coordinate with community care providers on medical documentation exchange for veterans receiving behavioral health services. As part of this work, we are reviewing data on behavioral health referrals to community care providers and assessing VHA’s oversight of medical documentation exchange.
Our preliminary observations show that from fiscal years 2021 through 2023, 224,741 veterans used referrals to receive behavioral health services from community providers. The majority of these veterans maintained a connection with a VHA medical facility, with about 90 percent keeping a VHA primary care provider and about 71 percent returning to VHA medical facilities to receive further behavioral health services. With nearly three-fourths of veterans returning to VHA medical facilities for behavioral health services after seeing a community provider for such services, ensuring that VHA medical facilities and community providers exchange medical documentation is critical to avoiding risks to the veterans’ continuity of care. We anticipate issuing our report by summer 2025.
In summary, VHA has faced a variety of challenges with the Veterans Community Care Program, including monitoring its facilities’ performance in scheduling appointments with community providers. Our work has identified a number of areas for improvement to the program. Since 2018, VHA has implemented some of our recommendations and taken steps to address others. Fully implementing our recommendations related to community care is important to ensuring that veterans have timely access to care. We stand ready to assist with providing continued oversight in this area.
Chairwoman Miller-Meeks, Ranking Member Brownley, and Members of the Subcommittee, this concludes my statement. I would be pleased to respond to any questions you may have.
GAO Contacts and Acknowledgments
If you or your staff have any questions about this testimony, please contact Sharon M. Silas at (202) 512-7114 or silass@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this statement. GAO staff who made key contributions to this testimony are Marcia A. Mann (Assistant Director), Julie T. Stewart (Analyst-in-Charge), Ying Hu, Megan Knox, Kelly Turner, and E. Jane Whipple. Other contributors include Jacquelyn Hamilton and Kate Tussey.
Appendix I: Open GAO Recommendations Related to the Department of Veterans Affairs (VA) Community Care Program
Table 1: Status of Open Recommendations Related to the Veterans Community Care Program for GAO Reports Included in This Statement, as of February 2025
|
GAO recommendation (GAO Report, Date) |
Implementation status |
|
The Under Secretary for Health should ensure that the Office of Integrated Veteran Care defines Referral Coordination Initiative program direction—strategic goals, roles and responsibilities, standards for consistent implementation, and oversight and accountability—in appropriate VHA national policy. (GAO‑25‑106678, January 2025) |
Open – Not Addressed. VA concurred in principle with our recommendation. In response to our draft report, VA acknowledged the importance of clear program direction and stated that the Referral Coordination Initiative was created to improve the referral coordination process, which is one piece of the overarching consult and referral management process. VA also said that the Referral Coordination Initiative should not be interpreted as a stand-alone process. We maintain that the Referral Coordination Initiative marks a significant change from how referrals have historically been managed within VA, and as such, our recommendation that program direction be fully defined in national policy would increase accountability mechanisms and help ensure veterans receive timely and effective care. The Veterans Health Administration (VHA) published a new national referral management policy on November 22, 2024. We will review this new policy as part of our recommendation follow-up process. |
|
The Under Secretary for Health, upon inclusion of the Referral Coordination Initiative in the appropriate VHA national policy, should ensure that the Office of Integrated Veteran Care aligns Referral Coordination Initiative guidance with VHA national policy and updates it as needed to reflect available evidence, such as findings from studies, best practices, and other elements that promote consistent implementation. (GAO‑25‑106678, January 2025) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA described actions the Office of Integrated Veteran Care would take to promote consistent implementation, such as a future update to Referral Coordination Initiative guidance. For example, VA stated that the Office of Integrated Veteran Care will update Referral Coordination Initiative guidance to include a Veterans Integrated Service Network-led model that is based on evidence-based studies and identified best practices. VA estimated that their actions would be completed by November 2025. |
|
The Under Secretary for Health, following initial alignment of Referral Coordination Initiative guidance and national policy, should ensure that the Office of Integrated Veteran Care establishes a process to ensure that any guidance remains current and accurate when the Office of Integrated Veteran Care makes changes to Referral Coordination Initiative policy or program requirements. (GAO‑25‑106678, January 2025) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA stated that the Office of Integrated Veteran Care will establish a process for recurring reviews and revisions of Referral Coordination Initiative guidance and other resources. VA estimated that their actions would be completed by November 2025. |
|
The Under Secretary for Health should ensure that the Office of Integrated Veteran Care reviews the Referral Coordination Initiative performance metrics, and updates them as needed, to ensure that the metrics align with and assess progress toward all aspects of Referral Coordination Initiative’s strategic goals. (GAO‑25‑106678, January 2025) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA stated that the Office of Integrated Veteran Care is in the process of reviewing, revising, and developing key performance indicators to assess its progress against Referral Coordination Initiative’s strategic goals. VA estimated that their actions would be completed by November 2025. |
|
The Under Secretary for Health should ensure that the Office of Integrated Veteran Care communicates with Veterans Integrated Service Networks and VHA facilities regarding how to use its metrics to measure performance toward the Referral Coordination Initiative goals. (GAO‑25‑106678, January 2025) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA described actions the Office of Integrated Veteran Care will take, including publishing information on the key performance indicators it develops on the internal Referral Coordination Initiative SharePoint. Further, the Office of Integrated Veteran Care plans to use community of practice calls and site visits to communicate informational updates. VA noted that, through these efforts, the Office of Integrated Veteran Care will also be able to incorporate feedback from Veterans Integrated Service Networks and facilities into the development of its program documentation. VA estimated that their actions would be completed by November 2025. |
|
The Secretary of VA should ensure that the Assistant Under Secretary for Health for Integrated Veteran Care establishes a complete set of documentation for oversight of the Community Care contracts, including documentation of clear and complete procedures and the identification of roles and responsibilities. (GAO‑24‑106390, August 2024) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA stated that the Office of Integrated Veteran Care will review existing contract oversight documentation and update the documentation accordingly. As of February 2025, we have not received an update from VA on actions taken to address this recommendation. |
|
The Secretary of VA should ensure that the Assistant Under Secretary for Health for Integrated Veteran Care assesses whether the oversight and reporting responsibilities of the program manager position outlined in the Quality Assurance Surveillance Plans are being effectively fulfilled by current processes and, if not, updates the plans as appropriate. (GAO‑24‑106390, August 2024) |
Open – Not Addressed. VA concurred in principle with our recommendation. In response to our draft report, VA stated that the Office of Integrated Veteran Care will review the responsibilities outlined in the Quality Assurance Surveillance Plans and mitigate any identified gaps. As of February 2025, we have not received an update from VA on actions taken to address this recommendation. |
|
The Secretary of VA should ensure that the Assistant Under Secretary for Health for Integrated Veteran Care develops a formal lessons learned process, consistent with leading practices, for the Community Care contracts to inform VA’s plans for the next set of contracts and its continuing oversight efforts. (GAO‑24‑106390, August 2024) |
Open – Not Addressed. VA concurred with our recommendation. In response to our draft report, VA stated that the Office of Integrated Veteran Care will use and refine the existing lessons learned process, including identifying areas for improvement. As of February 2025, we have not received an update from VA on actions taken to address this recommendation. |
|
The Undersecretary for Health should assess the risks associated with VA’s methodology for calculating specialty care network adequacy and revise its approach accordingly. (GAO‑24‑106410, June 2024) |
Open – Not Addressed. VA concurred with our recommendation. In November 2024, VA officials reported that VHA was in the process of assessing the methodology for specialty care network adequacy calculations and the requirements in VHA’s current community care contracts to identify risks and opportunities for improvement. According to officials, VHA is conducting this assessment in conjunction with its activities to prepare for the next generation of community care contracts. For example, officials state that one of their activities to prepare for the next community care contract is the development of a detailed operational plan that will include key objectives and milestones that are intended to enhance oversight and ensure that contractors maintain an adequate network. When VHA completes its assessment and preparations for the next generation of community care contracts, we will review these actions and evaluate whether they are sufficient to address our recommendation. |
|
The Undersecretary for Health should ensure that VA facility staff systematically capture the reasons for community care appointment scheduling challenges and use this information to help address those challenges. (GAO‑24‑106410, June 2024) |
Open – Not Addressed. VA concurred in principle with our recommendation. In response to our draft report, VA stated that it had put in place mechanisms to track community care appointment scheduling challenges. However, VA also noted it had not mandated the capture and reporting of reasons for scheduling delays due, in part, to the need for stronger contractual requirements that would require the contractor to act on the reasons. In December 2024, VA stated that it continued to use these mechanisms, which include, for example, required monthly meetings between the contractors and VA facilities, and the development of a ticketing system for VA facility staff to document recurring community care access issues. VA officials reported that they are using these mechanisms because requiring facility staff to systematically capture the reasons for appointment scheduling challenges would increase the administrative workload of VA staff. VA officials also stated that they are planning to conduct an analysis of scheduling challenges based on data obtained through these mechanisms. We will evaluate whether VA’s actions are sufficient to address our recommendation. |
|
The Undersecretary of Health should conduct a comprehensive analysis of appointment scheduling data from all VA medical centers to determine whether the community care timeliness standards are achievable and revise them as necessary. (GAO‑23‑105617, January 2023) |
Open – Partially Addressed. VA concurred with our recommendation. In May 2023, VA stated that VHA had conducted an analysis of community care scheduling for referrals VA medical centers scheduled from October 2022 through January 2023 against the timeliness standards to determine whether these standards were achievable. Consistent with our finding, VA’s analysis showed that many VHA facilities were not achieving the current timeliness standard of scheduling an appointment within 7 days of the file entry date. In response, VHA established a goal for each VHA facility to reduce the average number of days it takes to schedule appointments by specific percentage targets over time, in an effort to meet the 7-day scheduling standard. In June 2024, VHA officials reported that they continued to monitor this goal but also stated that VHA leadership was in the process of re-evaluating the 7-day scheduling standard. In November 2024, VHA officials reported that they had presented options for modifying the standard to the VHA Governance Board and that the Board had approved a proposed change in September. According to officials, VHA leadership is in the process of considering this proposed change. When VA completes these activities, we will evaluate the extent to which they have addressed our recommendation. |
|
The Undersecretary of Health should require referring providers and referral coordination team clinical reviewers to complete the role-based Referral Coordination Initiative training that VHA developed and track completion of the training to ensure familiarity with its updated scheduling process for VHA facility and community care appointments. (GAO‑23‑105617, January 2023) |
Open – Not Addressed. VA concurred with our recommendation. In response to our recommendation, VA officials have reported that they were updating available trainings on the referral management process to ensure that they fully reflect the process and that the documentation that referral coordination team reviewers complete is standardized. In a November 2024 update to its referral management directive, VHA required that providers complete referral management training within 120 calendar days of the directive’s publication. New providers are required to complete the training within 120 calendar days of their start date. According to VA officials, this required training will include a Referral Coordination Initiative role-based module. VA officials said VHA will track providers’ completion of this mandatory training. VA estimated that their actions would be completed by April 2025. At that time, we will evaluate whether the steps VA has taken are sufficient to address our recommendation. |
|
The Undersecretary of Health should align its monitoring metrics with the time frames established in the Veterans Community Care Program scheduling processa (GAO‑20‑643, September 2020) |
Open – Partially Addressed. VA initially did not agree with our recommendation but since February 2022 has started to address it. In a directive and standard operating procedure, VHA defined some time frames for VHA facilities to follow when scheduling appointments under the Veterans Community Care Program. However, VHA has not yet defined a timeliness standard for when a veteran’s appointment should occur (i.e., receipt of care). The Consolidated Appropriations Act, 2023, enacted on December 29, 2022, requires VHA to establish a specific wait time measure (the number of days from the date of request for the appointment to the first next available appointment) for veterans eligible for care under the Veterans Community Care Program and requires program third-party administrators to furnish care within this standard. In September 2023, VA officials stated that they continue to evaluate the technical, logistical, and financial implications of operationalizing these legislative requirements. When VA takes further actions, we will evaluate the extent to which those actions address our recommendation. |
|
The Under Secretary of Health should direct VA medical center leadership to assess their community care staffing and resource needs, and develop a plan to address any identified risks to their ability to schedule appointments in a timely manner, including strategies to adjust staff levels and address recruitment and retention challenges as needed. (GAO‑20‑643, September 2020) |
Open – Partially Addressed. VA agreed with our recommendation and in January 2023, stated that it last updated its staffing tool in March 2022 to enable each VA medical facility to quantify resource needs and identify the recommended number of administrative and clinical staff based on current workload data, systems, and processes. VA also stated that VA medical facilities are to make quarterly updates to the staffing tool, which is then used by the facility community care offices to support position requests and for discussions with leadership regarding community care staffing levels. In addition, VHA submits staffing tool results to Congress every 180 days. Under the Referral Coordination Initiative, VHA transitioned responsibilities for community care appointments from multiple clinical employees to designated referral coordination teams at each VA medical facility. In January 2023, VHA stated that community care staffing needs are expected to evolve further over the next year as VA medical facilities continue to recruit staff and implement new business processes, like the use of referral coordination teams and enhanced technological tools to expedite referral management and appointment scheduling. Although VA has made some progress in implementing this recommendation, we have asked for more evidence to show how VA uses the tool to help VA medical facilities develop plans to address any identified scheduling risks or to address recruitment and retention challenges. |
|
The Undersecretary for Health should establish an achievable wait-time goal for the consolidated community care program that VA plans to implement that will permit VHA to monitor whether veterans are receiving community care within time frames that are comparable to the amount of time they would otherwise wait to receive care at VHA medical facilities.a (GAO‑18‑281, June 2018) |
Open – Partially Addressed. VA agreed with our recommendation. The Consolidated Appropriations Act, 2023, enacted on December 29, 2022, requires VHA to establish a specific wait time measure (the number of days from the date of request for the appointment to the first next available appointment) for veterans eligible for care under the Veterans Community Care Program and requires program third-party administrators to furnish care within this standard. In September 2023, VA officials stated that they continue to evaluate the technical, logistical, and financial implications of operationalizing these legislative requirements. When VA takes further actions, we will evaluate the extent to which those actions address our recommendation. |
|
The Undersecretary for Health should design an appointment scheduling process for the consolidated community care program that VA plans to implement that sets forth time frames within which (1) veterans’ referrals must be processed, (2) veterans’ appointments must be scheduled, and (3) veterans’ appointments must occur, which are consistent with the wait-time goal VHA has established for the program.a (GAO‑18‑281, June 2018) |
Open – Partially Addressed. VA agreed with our recommendation and has so far, defined time frames for when a community care referral must be processed and scheduled, but has not yet defined a timeliness standard for when a veteran’s appointment should occur (i.e., receipt of care). The Consolidated Appropriations Act, 2023, enacted on December 29, 2022, requires VHA to establish a specific wait time measure (the number of days from the date of request for the appointment to the first next available appointment) for veterans eligible for care under the Veterans Community Care Program and requires program third-party administrators to furnish care within this standard. In September 2023, VA officials stated that they continue to evaluate the technical, logistical, and financial implications of operationalizing these legislative requirements. When VA takes further actions, we will evaluate the extent to which those actions address our recommendation. |
|
The Under Secretary for Health should issue a comprehensive policy directive and operations manual for the consolidated community care program VA plans to implement and ensure that these documents are reviewed and updated in a timely manner after any significant changes to the program occur. (GAO‑18‑281, June 2018) |
Open – Not Addressed. VHA agreed in principle with this recommendation and in January 2025, stated that the Office of Integrated Veteran Care has continued its development of a community care directive. VA estimated that their actions to develop the directive would be completed by June 2025. |
Source: GAO‑25‑106678, GAO‑24‑106390, GAO‑24‑106410, GAO‑23‑105617, GAO‑20‑643, and GAO‑18‑281 and GAO analysis of Veterans Health Administration (VHA) information. | GAO‑25‑108101
aGAO identifies priority open recommendations each year. These are GAO recommendations that have not been implemented and warrant priority attention from heads of key departments or agencies because their implementation could help the federal government save large amounts of money or significantly improve government operations. In the 2024 update, this was a priority open recommendation for VA. See GAO, Priority Open Recommendations: Department of Veterans Affairs, GAO‑24‑107265 (Washington, D.C.: June 3, 2024).
Related GAO Products
Veterans Health Care: Referral Coordination Initiative for Specialty Care Needs Improved Program Direction and Guidance. GAO‑25‑106678. Washington, D.C.: Jan. 21, 2025.
Veterans Community Care Program: VA Needs to Strengthen Contract Oversight. GAO‑24‑106390. Washington, D.C.: Aug. 21, 2024.
Veterans Health Care: Opportunities Exist to Improve Assessment of Network Adequacy for Mental Health. GAO‑24‑106410. Washington, D.C.: June 3, 2024.
Veterans Health Care: VA Actions Needed to Ensure Timely Scheduling of Specialty Care Appointments. GAO‑23‑105617. Washington, D.C.: Jan. 4, 2023.
Veterans Community Care Program: VA Needs to Strengthen Its Oversight and Improve Data on Its Community Care Network Providers. GAO‑23‑105290. Washington, D.C.: Nov. 10, 2022.
Veterans Community Care Program: Improvements Needed to Help Ensure Timely Access to Care. GAO‑20‑643. Washington, D.C.: Sept. 28, 2020.
Veterans Choice Program: Improvements Needed to Address Access-Related Challenges as VA Plans Consolidation of its Community Care Programs. GAO‑18‑281. Washington, D.C.: June 4, 2018.
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, X, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]VHA operates 170 medical centers and more than 1,100 outpatient facilities, which we refer to collectively as “VHA medical facilities.”
[2]In August 2014, after several well-publicized events highlighted serious and longstanding issues with veterans’ access to care, Congress enacted the Veterans Access, Choice, and Accountability Act of 2014. Among other things, the law established a temporary program—called the Veterans Choice Program—and provided up to $10 billion in funding for veterans to obtain health care services from community providers when they faced long wait times, lengthy travel distances, or other challenges accessing care at VHA facilities. Pub. L. No. 113-146, tit. I, §§ 101, 802(d), 128 Stat. 1754, 1755-1765, 1802-1803 (2014).
In 2019, the Veterans Community Care Program replaced the Veterans Choice Program and consolidated other existing community care programs. The VA MISSION Act of 2018 (VA MISSION Act) broadened veterans’ eligibility to receive care outside of the VA health care system under this program. Pub. L. No. 115-182, tit. I, §101, 132 Stat. 1393, 1395 (2018).
[3]Pub. L. No. 115-182, tit. I, § 101(a), 132 Stat. at 1395 (codified at 38 U.S.C. § 1703(d)(1)(E)).
[4]Similarly, GAO added VA acquisition management to our High-Risk List in 2019. This list focuses attention on government operations that are most vulnerable to fraud, waste, abuse, or mismanagement, or in need of transformation. To determine which federal government programs and functions should be designated “high risk,” we consider factors such as whether the risk involves public health or safety. See GAO, High-Risk Series: An Update, GAO‑15‑290 (Washington, D.C.: Feb. 11, 2015).
[5]GAO recommendations not yet fully implemented include ones that VA has partially addressed and those that VA has not yet addressed. We also closed one recommendation as not implemented as the time for VA to have addressed the recommendation before implementing the Veterans Community Care Program had passed.
[6]VHA policy uses the terms “consult” and “referral” when describing requests placed by VHA providers. For the purposes of this testimony, we will use the term referral. For a limited number of outpatient specialty services, veterans can schedule an initial or follow-up appointment at VHA medical facilities without a referral from a provider. Veterans can use this option for audiology, optometry, and podiatry, among other services.
[7]In addition to VHA medical facility scheduling on behalf of veterans, as of March 2024, 33 of 139 facilities were receiving contractor support in scheduling community care appointments. In some limited cases, veterans may also directly schedule appointments with providers.
[8]We have ongoing work examining the creation and implementation of VHA’s Office of Integrated Veteran Care.
[9]See 10 U.S.C. § 1703 and implementing regulations at 38 C.F.R. §§ 17.4000 - 17.4040 (2024).
[10]In addition to the six criteria, veterans must either be enrolled in VA health care or be eligible for VA care without needing to enroll, and in most circumstances, veterans must receive approval from VHA prior to obtaining care from a community provider. See Pub. L. No. 115-182, tit. I, § 101, 132 Stat. at 1395-1404 (codified, as amended, at 38 U.S.C. § 1703(d), (e)) and implementing regulations at 38 C.F.R. §§ 17.4000 - 17.4040.
[11]Network adequacy is measured by standards designed to ensure that veterans have access to community providers who can offer timely care.
[12]See Recommendations 3, 4, 5, 6, 7, and 8 from Veterans Choice Program: Improvements Needed to Address Access-Related Challenges as VA Plans Consolidation of its Community Care Programs, GAO‑18‑281 (Washington, D.C.: June 4, 2018) and Recommendation 2 from Veterans Community Care Program: Improvements Needed to Help Ensure Timely Access to Care, GAO‑20‑643 (Washington, D.C.: Sept. 28, 2020). We also closed one recommendation as not implemented because it was no longer valid given changes in VA.
[17]GAO, Veterans Health Care: Opportunities Exist to Improve Assessment of Network Adequacy for Mental Health, GAO‑24‑106410 (Washington, D.C.: June 3, 2024).
[18]GAO, Veterans Health Care: Referral Coordination Initiative for Specialty Care Needs Improved Program Direction and Guidance, GAO‑25‑106678 (Washington, D.C.: Jan. 21, 2025).
[19]GAO, Veterans Community Care Program: VA Needs to Strengthen Its Oversight and Improve Data on Its Community Care Network Providers, GAO‑23‑105290 (Washington, D.C.: Nov. 10, 2022).
[20]GAO, Veterans Community Care Program: VA Needs to Strengthen Contract Oversight, GAO‑24‑106390 (Washington, D.C.: Aug. 21, 2024).
