VA NURSING HOME CARE
Opportunities Remain to Enhance Oversight of State Veterans Homes
Statement of Sharon M. Silas, Director, Health Care
Before the Subcommittee on Health, Committee on Veterans’ Affairs, House of Representatives
For Release on Delivery Expected at 2:15 p.m. ET
United States Government Accountability Office
For more information, contact Sharon M. Silas at silass@gao.gov.
Highlights of GAO-25-108441, a testimony
before the Subcommittee on Health,
Committee on Veterans’ Affairs, House of
Representatives
Opportunities Remain to Enhance Oversight of State Veterans Homes
Why GAO Did This Study
Veterans—like many other Americans—rely on nursing home care to help meet their health needs as they age. In fiscal year 2023, VA paid about $1.5 billion for veteran nursing home care provided in state veterans homes.
This statement describes (1) oversight of state veterans homes; and (2) the status of VA efforts to implement GAO recommendations to strengthen oversight of state veterans homes.
This statement is based on GAO’s November 2022 report (GAO-23-105167) on oversight of state veterans homes. To do that work, GAO conducted a nationwide survey to collect information on the 153 state veterans homes providing nursing home care. GAO also reviewed relevant laws and VA documents and interviewed federal and state officials, state veterans homes’ officials, and other organizations involved with veteran care, such as veterans service organizations. For this statement GAO reviewed expenditure and utilization data for fiscal year 2023 and provided updates on the status of GAO’s recommendations.
What GAO Recommends
In its November 2022 report, GAO made four recommendations. VA agreed with the recommendations and implemented three of them. However, VA has not implemented a recommendation to identify additional enforcement tools to help ensure state veterans home compliance with quality standards and seek legislative authority to implement them, as appropriate.
What GAO Found
The Department of Veterans Affairs (VA) is the only federal entity that oversees all state veterans homes. The Centers for Medicare & Medicaid Services (CMS) and state agencies also have an oversight role in some of these homes. While these homes are owned and operated by states, VA helps pay for care for eligible veterans and is required to ensure each home meets VA’s quality standards. To do this, VA conducts regular inspections. Homes that do not meet standards can be cited for deficiencies. CMS also conducts inspections in homes that receive Medicare or Medicaid payments and can also cite deficiencies. For example, as of January 2022, CMS inspected 116 of the 153 state veterans homes. In response to GAO’s 2022 national survey of state agencies that operate state veterans homes, 43 states also reported inspecting homes for compliance with state-specific regulations.
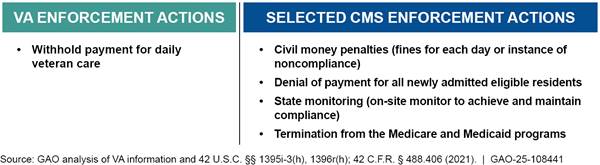
VA has implemented three of four GAO recommendations to strengthen oversight of state veterans homes. For example, VA developed a process to consistently follow up with homes that have not implemented their corrective action plans by agreed upon dates. However, VA has not addressed GAO’s recommendation to identify a range of enforcement actions to bring state veterans homes into compliance with quality standards. Unlike CMS, VA lacks a range of enforcement actions (see figure). At the time of GAO’s report, over 40 percent of homes were deficient in the same standard in both 2019 and 2021. VA had never used its only enforcement action, withholding payment, considering it too severe for most situations. VA officials said they were considering seeking legislative authority to take additional enforcement actions to ensure compliance with quality standards.
Available Enforcement Actions for Department of Veterans Affairs and Selected Actions for Centers for Medicare & Medicaid Services, as of November 2022
However, in 2025, VA officials said they are no longer pursuing the identification of additional enforcement actions and corresponding legislative authority. Instead, in 2024 VA developed a new enforcement plan that strengthens timelines and increases the amount of follow-up with homes that have deficiencies. However, the plan does not include a mechanism to compel compliance with VA’s quality standards.
GAO maintains that having a range of enforcement options would help VA meet its program goals, align VA’s practices with CMS’s, and help VA ensure veterans receive quality care in state veterans homes.
April 29, 2025
Chairwoman Miller-Meeks, Ranking Member Brownley, and Members of the Subcommittee:
I appreciate the opportunity to be here today to discuss the Department of Veterans Affairs’ (VA) oversight of state veterans homes.
Like many older Americans, aging veterans may have extensive health care needs and require skilled nursing home care to meet their daily needs. For many of these veterans, VA provides or pays for nursing home care in three settings: VA-owned and -operated community living centers, publicly or privately owned community nursing homes, and state-owned and -operated state veterans homes.[1]
In fiscal year 2023, VA spent almost $8.4 billion for approximately 36,000 veterans who required skilled nursing and personal care in an institutional setting. More than 40 percent of these veterans—almost 15,000—received this nursing home care in state veterans homes at a cost of about $1.5 billion. To receive VA payments, the state veterans homes must meet VA quality standards related to quality of care, quality of life, infection control, and resident rights, among other areas. Homes that fail to meet the standards can be cited for deficiencies by VA. Some of these homes also receive payments from the Centers for Medicare & Medicaid Services (CMS). These homes must also meet CMS quality standards and can be cited for deficiencies by CMS.
Over the past several years, we reported on opportunities for VA to enhance its oversight of state veterans homes to ensure aging veterans receive high-quality care.[2] My statement today summarizes findings from our most recent report from November 2022. It describes
1) oversight of state veterans homes and
2) the status of VA’s efforts to implement our recommendations to strengthen oversight of these homes.
To perform the work for our November 2022 report, we reviewed federal documents, conducted a national survey of officials from the state agencies that operate 153 state veterans homes, and interviewed officials from VA and other organizations, including state veterans homes and veterans service organizations.[3] We reviewed VA and CMS documents about state veterans home inspection policies and processes, and documents on VA’s oversight process for state veterans homes (modeled after CMS’s system). We also reviewed applicable statutes and regulations pertaining to VA’s oversight authorities. Further details on our scope and methodology can be found in our November 2022 report. For this statement, we also reviewed VA’s fiscal year 2025 congressional budget submission to obtain fiscal year 2023 data on state veteran home utilization and expenditures. Additionally, we reviewed written statements VA provided about the status of its efforts to implement our recommendations.[4]
The work on which this statement is based was performed in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
VA supports state veterans homes by providing per diem payments for each day that an eligible veteran is receiving care and has an overnight stay, with certain exceptions.[5] VA also provides grants to construct, acquire, remodel, or modify state veterans homes, and payments to states for the hiring and retention of nurses.[6] State veterans homes are owned and operated by the state in which they are located. Federal statute prohibits VA from having authority over the management of or control of any state home.[7]
Depending on the veteran, VA pays the full or partial cost of state veterans home care.[8] States have different methods of funding the remaining balance, including private out-of-pocket payments from the veteran or state general funds. States might also obtain payment from CMS for services furnished to eligible individuals in state veterans homes certified to participate in Medicare or Medicaid.
VA, CMS, and States Can Each Have a Role in Overseeing State Veterans Homes
VA is the only federal entity that oversees all state veterans homes and must ensure they meet applicable quality of care and other standards in order to provide them with payments. Any home that participates in Medicare or Medicaid is also overseen by CMS to ensure they meet the federal quality standards required to receive those payments. Finally, states may subject homes to their own regulations—and, in 2022, we found a majority did.
VA Oversight
Federal law and VA policy prevent VA from making payments to state veterans homes until it determines that they meet applicable quality of care and other standards.[9] Within VA, the Office of Geriatrics and Extended Care (GEC) is responsible for overseeing the quality of care provided to veterans at state veterans homes. Each home is affiliated with a VA medical center. The VA medical center of jurisdiction—usually the medical center located closest to the home—is responsible for helping veterans make decisions about nursing home care, responding to inquiries from state veterans home management, referring management to the appropriate VA office, among other things. Each VA medical center resides within regional networks called Veterans Integrated Services Networks, and GEC works with liaisons within each regional network to address state veterans home quality issues, as needed.
As a function of its oversight, VA contracts with a third party to conduct inspections that determine the extent to which state veterans homes meet relevant nursing home quality of care standards.[10]
· State veterans homes must first be inspected for recognition, which makes them eligible to receive VA’s per diem. VA reviews policies, procedures, staffing patterns, and all other requirements appropriate to the facility’s level of care and issues a pass or fail decision for the facility.
· Once a home is recognized by VA, subsequent inspections are generally unannounced and typically occur annually or in response to a specific incident or complaint. As we reported in 2022, VA policy calls for inspections of state veterans homes on a regular schedule, approximately yearly, to assess compliance with 189 standards across 16 categories.
· Additionally, VA conducts for-cause inspections—which are typically unannounced—that may arise from complaints or facility reported incidents.
Any applicable standard that VA’s inspectors find to be “not met” during an inspection triggers a deficiency citation to the state veterans home. Each deficiency is classified using a system that CMS developed for its inspections of nursing homes. VA rates each deficiency for its scope—which indicates whether the deficiency is isolated to one patient, a pattern, or widespread; and its severity—which indicates whether the deficiency can cause harm or poses immediate jeopardy to resident health or safety.
State veterans homes must submit a corrective action plan for each deficiency cited during a VA inspection; included in these plans are specific steps that must be taken to correct the deficiency. As we reported in 2022, homes with an accepted corrective action plan in place are “provisionally certified” and are eligible to continue to receive per-diem payments.[11] In the event of continued non-compliance, VA may withhold its per diem payments to state veterans homes. This requires approval by the VA Secretary and may happen if, for example, the home has an egregious deficiency or a history of well-documented non-compliance.
CMS Oversight
While VA is the only federal agency to inspect all state veterans homes, CMS also oversees many of them due to their participation in Medicare or Medicaid as part of CMS’ oversight of over 15,000 certified nursing homes nationwide.[12] We reported that, as of January 2022, 76 percent of state veterans homes were also inspected by CMS.[13] CMS enters into agreements with state survey agencies to inspect these homes for compliance with federal standards, as it does for all nursing homes that receive Medicare or Medicaid payments. CMS policy calls for the inspection of nursing homes, including state veterans homes, every 15 months or less. CMS inspections assess compliance with federal quality standards or may be conducted for cause.
Like VA, CMS requires state veterans homes to develop a corrective action plan for each deficiency in a routine or for-cause inspection, including anticipated dates of correction. Depending on the scope and severity of the deficiency, the state survey agency may revisit the home on behalf of CMS to ensure it implemented the plan and corrected the deficiency. Additionally, unlike VA, CMS has the authority to impose a range of enforcement actions on state veterans homes with deficiencies.
State-Specific Oversight
In response to our national survey conducted in early 2022, state officials in 43 states indicated that they also conduct their own state-specific inspections in addition to the oversight conducted by VA and CMS.[14] States that reported conducting some kind of oversight said they did so through either routine inspections based on state-specific nursing home quality regulations, for-cause inspections, or both. In contrast, 7 states reported they did not have either state-specific nursing home quality regulations or for-cause inspections.[15]
Of the 43 states that reported assessing compliance with state-specific nursing home quality regulations or conducting their own for-cause inspections, 41 reported requiring state veterans homes to use a corrective action plan, separate from any federal plan to bring deficiencies into compliance. Additionally, 37 states reported they have the option to take one or more enforcement actions if a home does not meet state standards. Survey respondents reported various types of enforcement actions their states can take, including issuing monetary penalties or fines (30 states), closing the home (28 states), or suspending admissions to the home (27 states).[16]
VA Has Taken Recommended Actions to Strengthen Oversight, but Has Not Expanded Enforcement Options to Help Ensure Compliance with Standards
In our November 2022 report we identified four areas in which VA could improve its oversight of state veterans homes. Specifically, we recommended that VA (1) improve its data analysis capabilities; (2) improve the effectiveness of corrective action plans by developing a process for following up on plans that lack evidence of timely implementation; (3) ensure its efforts to centralize oversight processes are successful by bringing them into alignment with VA policy; and (4) identify additional enforcement actions that could help ensure state veterans home compliance with quality standards and seek legislative authority to implement them, as appropriate. VA has implemented the first three of these recommendations.
VA Has Implemented Three GAO Recommendations to Strengthen Oversight of State Veterans Homes
As of March 2025, VA has implemented three of the recommendations we made in our November 2022 report. In doing so, VA has strengthened its oversight of state veterans homes in the following three areas:
· Data analytic capabilities. We found that VA officials were limited in their ability to efficiently analyze state veterans home oversight data. We recommended that VA develop a plan to ensure its data system would have the capabilities to aggregate and analyze state veterans home data by multiple units of measurement, including by state and home, and across survey years. In September 2023, VA provided evidence of a plan for developing a system for state veterans home data.
· Oversight of corrective action plans. We found that VA officials did not have a process for following up with state veterans homes about accepted corrective action plans, which are required for all deficiencies cited during a VA inspection. We recommended that VA implement a process for consistently following up with homes that have not implemented their corrective action plans by agreed upon dates. In September 2023, VA provided us with evidence that the agency developed and implemented a process to follow up with homes within 1 month of the agreed upon completion date. VA also provided evidence that they have improved their survey tracking tool to help staff manage these dates.
· Formalizing its oversight structure. We found that VA had not formalized changes in its oversight structure which it initiated in January 2022. At that time, VA began centralizing oversight of state veterans homes by shifting responsibilities for many tasks previously conducted by the 105 representatives at the VA medical center of jurisdiction to four new national program managers in VA’s central office. VA officials said that centralizing state veterans home oversight at the national level would help improve data consistency, communication, and planning, while ensuring all oversight is aligned in a single national office. As discussed in our November 2022 report, we found these centralization efforts to be promising and recommended that VA formalize this new oversight structure, which it did. Specifically, VA issued an interim notice in October 2023 outlining its centralization efforts and new oversight requirements for state veterans homes. This notice, renewed in August 2024, serves as policy until a new state veterans home directive is published by VA.
VA Has Not Implemented GAO Recommendation to Identify and Implement a Range of Enforcement Actions
We reported in 2022 that VA could further improve compliance with quality standards by identifying a range of enforcement actions. VA officials said its one available action—withholding per diem payments—has never been used because they considered it too severe for most situations, as it could result in veterans being transferred out of the state veterans home. At the time of our 2022 report, VA officials said it had been over a decade since the agency considered withholding a noncompliant home’s per diem.[17]
As we reported in November 2022, VA’s enforcement options are limited compared with CMS (see fig. 1). CMS can impose civil money penalties of varying amounts, rather than withhold payments, among other enforcement actions. In this way, CMS has a range—from mild to severe—of enforcement actions available to help get nursing homes in compliance. These actions are based on the scope and severity of the deficiencies, ratings that VA also uses in its inspection process. The administrator at one state veterans home we interviewed said due to the difference between VA and CMS enforcement powers, they were more concerned about deficiencies cited by CMS than by VA.
Figure 1: Enforcement Actions Available for VA and Selected Enforcement Actions Available for CMS for Noncompliance with Quality Standards, as of November 2022
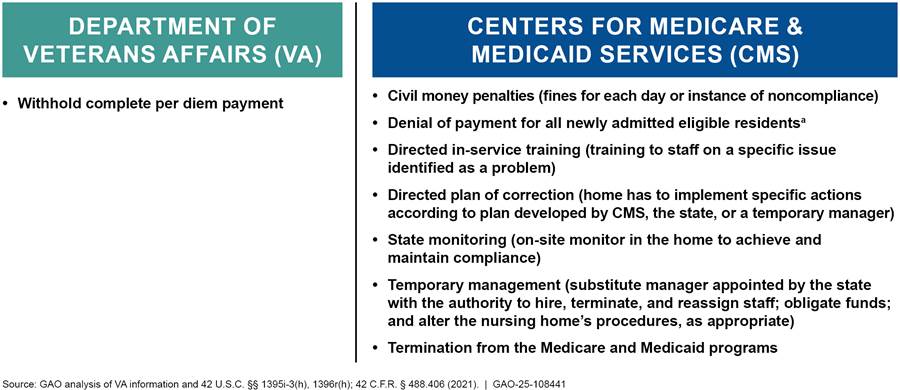
aCMS may also deny payment for all Medicare- or Medicaid-covered residents, but this remedy is seldom used. According to CMS, it is mindful of the potential consequences of such actions when assessing whether to impose or continue a payment suspension.
Having a range of enforcement actions could help VA tailor its enforcement for the scope and severity of deficiencies identified. In our analysis of deficiencies cited in VA inspections, we found deficiencies ranged in their scope and severity:
· The most common scope and severity ratings for deficiencies in both 2019 and 2021 were lower-level ratings—isolated in scope and no actual harm.
· However, over 21 percent of the deficiencies with corrective action plans that were past the due date in 2021 were rated as causing actual harm.
· Over 40 percent of homes for which we had annual inspection data from both 2019 and 2021 were cited for the same deficiency, meaning they failed to meet the same standard in both years.
The range of deficiencies’ scope and severity ratings indicate that some deficiencies may be more appropriately addressed with less severe actions than complete withholding of per diem payments from the home.
As such, in our November 2022 report, we recommended VA identify additional enforcement actions and seek legislative authority to implement them, as appropriate. VA concurred with this recommendation, and officials told us during our audit work they were considering a legislative proposal to Congress for the authority to impose fines or withhold a percentage of per diem payments to address noncompliance with quality standards. However, VA officials said in 2025 they are no longer pursuing any changes to current statutes or regulations.
Instead of identifying new enforcement actions and pursuing legislative authority, in 2024 VA developed a new enforcement plan to strengthen timelines, increase the amount of follow-up with homes that have deficiencies, provide VA medical centers the option to pause admission referrals, and allow VA to “delay” granting provisional certification to a home.[18] While these actions might enhance oversight of state veterans homes, they do not provide VA with the range of tools needed to compel compliance with quality standards. Instead, VA is limited to the one compliance tool it already has in place—withholding a home’s per diem payments—the most severe penalty.
We maintain that having a range of enforcement options would give VA the tools to align enforcement actions with the scope and severity of the deficiency. Such a process would help ensure compliance and fiscal integrity, one of VA’s goals for its state veterans home program. It would also align VA’s practices with those used by CMS, which uses a range of remedies that allow it to account for the scope and severity of a deficiency.[19] With a range of remedies, VA would be better positioned to compel state veterans homes to address issues of noncompliance, better ensuring quality care for aging veterans.
In conclusion, while CMS and states can have an oversight role for state veterans homes, VA is the only federal entity that oversees all state veterans homes. While the department has taken steps to improve its oversight, VA’s oversight could be strengthened if it had a range of available enforcement actions to help ensure its standards are met. We will continue to monitor VA’s efforts to address this recommendation.
Chairwoman Miller-Meeks, Ranking Member Brownley, and Members of the Subcommittee, this concludes my statement. I would be pleased to respond to any questions you may have.
GAO Contact and Staff Acknowledgments
If you or your staff have any questions about this testimony, please contact Sharon M. Silas at silass@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this statement. GAO staff who made key contributions to this testimony are Karin Wallestad (Assistant Director), Erin C. Henderson (Analyst-in-Charge), Topher Hoffmann, and Jennifer Whitworth.
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on X,
LinkedIn, Instagram, and YouTube.
Subscribe to our Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]In general, the three settings provide similar nursing home care, in which veterans receive skilled nursing care, recreational activities, and other services. While the cost of care varies across the three settings, in fiscal year 2023, the average daily cost for veterans receiving VA- supported nursing home services was lowest in state veterans homes.
[2]See GAO, VA Nursing Home Care: Opportunities Exist to Enhance Oversight of State Veterans Homes, GAO‑23‑105167 (Washington, D.C.: Nov. 14, 2022); GAO, COVID-19: Urgent Actions Needed to Better Ensure an Effective Federal Response, GAO‑21‑191 (Washington, D.C.: Nov. 30, 2020); and GAO, VA Nursing Home Care: VA Has Opportunities to Enhance Its Oversight and Provide More Comprehensive Information on Its Website, GAO‑19‑428 (Washington, D.C.: July 3, 2019).
[3]As of January 2022, 160 state veterans homes were officially recognized by VA. Of those, 153 provided nursing home care. The remaining 7 were domiciliaries only.
[4]We have had multiple communications with VA about the status of their efforts to address our recommendations from 2023 to March 2025.
[5]See 38 U.S.C. §§ 1741, 1745. In certain circumstances, VA also pays per diem when there is no overnight stay (i.e., the veteran is temporarily absent from the facility) if the facility has a 90 percent or greater occupancy rate.
[6]See 38 U.S.C. §§ 8131-8138 and § 1744.
[7]38 U.S.C. § 1742(b).
[8]According to VA policy, its payments are equal to the lesser of the annual basic per diem rate—determined annually on a fiscal year basis—or one-half of the daily cost of nursing home care provided to eligible veterans in the state veterans home. VA is required by law to provide the full cost of nursing home care for veterans who need nursing home care for a service-connected disability—which is an injury or disease that was incurred or aggravated while on active duty—and for veterans with service-connected disabilities rated at 70 percent or more. See 38 U.S.C. § 1710A(a). Unless reauthorized, this statutory requirement will terminate on September 30, 2025. For these veterans, VA makes prevailing rate per diem payments. See 38 C.F.R. § 51.41 (2024).
[9]38 U.S.C. § 1742(a); Department of Veterans Affairs, Veterans Health Administration (VHA), Survey Requirements for State Veterans Homes, VHA Directive 1145.01 (Washington, D.C.: Feb. 18, 2021).
[10]VA will inspect the home in accordance with 38 C.F.R. § 51.31 to determine whether the home and program of care meet the applicable requirements of 38 C.F.R. Part 51, Subpart C, and the applicable standards in Subparts D, E, or F.
[11]Provisional certification allows homes to receive per-diem payments while they address deficiencies cited in an inspection through the corrective action plan process. See GAO‑23‑105167.
[12]See 42 U.S.C. §§ 1395i-3(f)(1),1396r(f)(1); 42 C.F.R. Part 483, Subpart B (2024).
[14]We conducted our survey in March through April 2022. At the time of our survey, the 7 states that said they did not conduct their own inspections of state veterans homes were Louisiana, Minnesota, Missouri, Nevada, New Hampshire, New Mexico, and Utah. We deployed the survey in all 50 states and Puerto Rico (Washington, D.C., does not have any state veterans homes), but Wyoming was then excluded from analysis because, at the time of our survey, it reported not having any state veterans homes that provide nursing home care. For our reporting purposes Puerto Rico is included in state summary counts when applicable. For the full survey results including lists of state oversight policies and of all 153 state veterans homes that provided nursing home care at the time of our survey—including their location, number of nursing home beds, and whether they were certified by CMS—see GAO‑23‑105167.
[15]Like all states, these states’ homes are subject to VA inspections and some also receive CMS inspections. At the time of our survey, among the 25 state veterans homes that provide nursing home care in these states, 8 of them—those in New Hampshire and Missouri—were not inspected by CMS because they were not Medicare or Medicaid-certified, and only received oversight from VA.
[16]Other types of enforcement actions that states reported they can take include withholding state payments or funds (21 states), having a different state agency temporarily take over management of the home (16 states), revoking the home’s license (4 states), and imposing fines or imprisonment for operating a facility without a license (1 state).
[17]Since withholding per diem payments could result in residents being transferred out of the home, officials told us in 2022 that this would only be considered if the deficiency is egregious, the home makes no attempt to fix the deficiency, and the home has a history of well-documented non-compliance. The Secretary of VA would have to approve the withholding of per diem payments, according to VA officials.
[18]According to VA officials, VA medical centers may pause admission referrals on a case-by-case basis and would still be able to receive referrals from other sources. Per diem payments are not withheld unless provisional certification is denied.
[19]VA generally used the CMS model for developing its inspection methods. See 42 U.S.C. §§ 1395i-3(h)(2)(B), 1396r(h)(3)(C); 42 C.F.R. § 488.406 (2024).
