SOUTHWEST BORDER
CBP Should Improve Oversight of Medical Care for Individuals in Custody
Report to Congressional Requesters
GAO-26-107425
A report to congressional requesters
For more information, contact: Rebecca Gambler at gamblerr@gao.gov or Travis Masters at masterst@gao.gov
What GAO Found
U.S. Customs and Border Protection (CBP), through its components U.S. Border Patrol and Office of Field Operations, detains individuals who unlawfully enter the U.S. at short-term holding facilities. CBP personnel process individuals and determine the next course of action, such as transferring them from custody or removing them from the country. For the past decade, CBP has used contracted medical personnel at facilities along the southwest border to provide health screenings and treatment of basic medical conditions to individuals in custody.

GAO found that CBP developed policies and guidance for providing medical care to individuals in custody but has not consistently implemented them. For example, CBP requires some populations, such as children, pregnant individuals, and adults who indicated they might have an illness or injury, to receive a basic physical exam known as a medical assessment. Although CBP introduced new guidance and improved the percentage of individuals who received medical assessments, GAO found that some individuals still did not receive assessments, as required. For example, 57 percent of adults with a potential illness or injury and 20 percent of pregnant individuals did not receive medical assessments from August 2023 to August 2024, as required. Without an oversight mechanism to ensure that people in custody receive the required medical assessments, CBP may not be aware of medical needs and cannot ensure it takes the appropriate next steps for any necessary medical care.
GAO also found that CBP and contracted medical personnel did not consistently implement additional care requirements for individuals in custody who had serious injuries or illnesses (i.e., those who were medically high-risk). For example, from August 2023 to August 2024, contracted medical personnel did not conduct medical monitoring checks required for medically high-risk adults and children approximately 40 percent of the time. In July 2025, CBP developed new tools to inform its oversight efforts, but did not explain how it will use them to systematically assess whether medically high-risk individuals received their medical monitoring checks on time. Developing and implementing a mechanism to monitor this requirement and others would help CBP better ensure these individuals receive required care, and personnel are monitoring their conditions.
CBP did not consistently provide medical records and prescriptions—referred to as medical summary forms—as required, to individuals with medical issues leaving CBP custody. By not providing the medical summary forms, CBP can create challenges with continuity of care. GAO also found CBP’s oversight reports did not include data from facilities that do not have contracted medical personnel. These facilities send individuals to local hospitals or urgent care facilities for medical care, including medical assessments. Without these data, CBP cannot ensure all individuals in custody received required medical assessments to decrease the risk of adverse medical outcomes.
Moreover, GAO’s analysis showed that CBP did not consistently manage or oversee its medical services contracts. For example:
· CBP did not clearly specify minimum staffing levels it requires of the contractor in the medical services contract. As such, CBP cannot ensure it has sufficient contracted medical personnel to meet its needs for providing medical care at its facilities; and
· CBP has not analyzed the costs and benefits of providing certain types of care through contracted medical personnel versus sending individuals to local hospitals. Performing a cost benefit analysis gives CBP the opportunity to identify potential cost savings.
GAO also identified gaps in CBP’s contract oversight, which could be remedied with a contract administration plan. For example, GAO found that CBP officials with contract oversight duties did not visit CBP facilities to directly observe performance under the medical services contracts until 2024. While CBP received reports from the contractor, it did not have metrics to measure contractor performance. Without a plan that includes roles and responsiblities and performance metrics, CBP is missing opportunities to obtain a more complete and quantifiable understanding of contractor performance.
CBP did not always submit contractor past performance evaluations as required. Ensuring that CBP complies with the requirements to submit these evaluations annually and at the end of the performance period would allow CBP to use more current information in its ratings. Such compliance would also better position officials to make informed decisions when awarding future medical services contracts.
U.S. Customs and Border Protection (CBP) Submission of Contractor Past Performance Evaluations for the Medical Services Contracts as of August 2025

GAO found that CBP met many of its medical quality management program requirements in overseeing the quality of care that contracted medical personnel provide. However, CBP does not have guidance that includes clear responsibilities for the Office of the Chief Medical Officer and did not track corrective actions taken after some medical events. Doing so would help CBP ensure the safety and quality of all medical services provided to individuals in CBP custody.
Why GAO Did This Study
From fiscal years 2021 through 2024, CBP encountered about 2 million individuals along the southwest border each year, resulting at times in overcrowding in its facilities. In May 2023, the death of an 8-year-old girl in CBP custody raised concerns about CBP's provision of medical care.
This report focuses on the southwest border and examines the extent to which CBP has (1) developed and implemented policies for providing medical care for individuals in its custody and (2) managed its contracts for medical services and provided oversight of its contractor.
To conduct this audit, GAO reviewed CBP documentation, including medical care guidance and other documentation related to screening and assessing individuals for medical issues. GAO observed CBP and contractor implementation of policies, challenges, and management of medical care at 31 CBP facilities along the southwest border, selected among areas with higher encounters.
Additionally, GAO analyzed data for fiscal years 2021 through 2024 (the most recent available at the time of our review) to assess the extent to which CBP components implemented its medical policies, its guidance, and federal internal control standards. GAO reviewed CBP contract file documentation for the three medical services contracts in this same period. GAO compared documentation of monitoring and performance activities against contract requirements, agency policies, and procurement regulations.
GAO interviewed CBP officials in headquarters and field locations to gain their perspectives on its provision of medical care. GAO also interviewed contracting officials regarding their efforts and responsibilities in managing and overseeing the contractor.
What GAO Recommends
GAO is making 14 recommendations to CBP, including to:
· Implement an oversight mechanism to ensure individuals get required medical assessments;
· Implement an oversight mechanism for required medical care related to medically high-risk individuals, such as medical monitoring checks;
· Develop and implement a mechanism to ensure that individuals with medical issues have their medical summary forms any time they leave CBP custody;
· Monitor whether individuals at facilities without contracted medical personnel receive medical assessments under CBP guidance;
· Specify the minimum staffing level needs for contracted medical personnel in any future medical services contracts;
· Analyze the costs and benefits of limiting the types of care that contracted medical personnel can provide versus sending individuals to local hospitals and document any resulting cost savings;
· Develop a contract administration plan for any future medical services contracts;
· Comply with the timing requirements in the Federal Acquisiton Regulation to ensure that contractor past performance evaluations for any future medical services contracts are submitted at least annually and also at the end of the period of performance; and
· Update existing guidance to include clear responsibilities and track corrective actions for sentinel events, among other medical quality management actions.
DHS concurred with thirteen recommendations. It did not concur with one recommendation to document the factors CBP personnel should consider when determining whether individuals are at-risk based on serious physical or mental injuries or illnesses for the purpose of expeditious processing under CBP’s standards. GAO maintains that DHS should do so to ensure consistent implementation of CBP’s expedited processing requirement.
Abbreviations
|
CBP |
U.S. Customs and Border Protection |
|
COR |
contracting officer’s representative |
|
DHS |
Department of Homeland Security |
|
FAR |
Federal Acquisition Regulation |
|
ICE |
U.S. Immigration and Customs Enforcement |
|
MQM |
Medical Quality Management |
|
OCMO |
Office of the Chief Medical Officer |
|
OFO |
Office of Field Operations |
|
TEDS |
National Standards on
Transport, Escort, Detention, and |
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
January 14, 2026
Congressional Requesters
From fiscal years 2021 through 2024, the Department of Homeland Security’s (DHS) U.S. Customs and Border Protection (CBP) apprehended about 2 million individuals along the southwest border each year, resulting at times in overcrowding in its facilities. In May 2023, the death of an 8-year-old girl while in CBP custody raised concerns about CBP’s provision of medical care.
CBP is responsible for detecting and interdicting individuals unlawfully entering the U.S. CBP personnel detain apprehended individuals at short-term holding facilities (U.S. Border Patrol facilities or ports of entry) to complete processing and determine the next course of action. This can include transferring the individuals to the custody of another agency, removing them from the country, or releasing them. In addition, CBP is responsible for providing medical care for apprehended individuals in its custody. For nearly a decade, CBP has used contracted personnel at its facilities along the southwest border to provide on-site medical services for individuals in custody.
We and others have reported on issues with CBP’s provision of medical care. For example, in July 2020, we identified gaps in CBP’s implementation and oversight of medical care and made recommendations to address those issues.[1] Among other findings, we found that CBP had not provided agents and officers training on recognizing medical distress in children. We recommended CBP develop and implement this training and CBP did so. We also found that CBP did not have reliable information on deaths, serious injuries, and suicide attempts and had not consistently reported deaths of individuals in custody to Congress. We recommended that CBP provide additional guidance on the procedures for reporting deaths in custody and CBP did so. DHS’s Office of Inspector General and Office of the Immigration Detention Ombudsman have also raised concerns with CBP’s medical services contracts, citing staffing shortages of medical personnel at CBP facilities and inconsistent contractor compliance with contract terms, such as staffing and accuracy of financial invoices.[2]
In light of renewed concerns, you asked us to review CBP’s provision of medical care for individuals in its custody along the southwest border and CBP’s management of its contracts for medical services. This report examines (1) the extent to which CBP has developed and implemented policies for providing medical care for individuals in its custody and (2) the extent to which CBP has managed its contracts for medical services and provided oversight of the contractor.
To address these objectives, we conducted site visits to 31 CBP facilities along the southwest border in Arizona, California, and Texas from June through September 2024. Of these 31 facilities, 28 had contracted medical personnel onsite and three did not. We selected locations from areas with the highest overall volume of encounters and most growth in volume from fiscal year 2023 to fiscal year 2024.[3] During these visits, we observed facility operations and interviewed CBP officials and contractor personnel providing medical services at these facilities. We also interviewed officials with DHS and CBP headquarters, including officials within the U.S. Border Patrol, the Office of Field Operations (OFO), and CBP’s Office of the Chief Medical Officer (OCMO).
To assess the extent to which CBP has developed and implemented medical care policies, we reviewed CBP policies and guidance related to medical care, such as CBP’s 2015 National Standards on Transport, Escort, Detention, and Search (TEDS).[4] We also analyzed data from November 2020 through August 2024 from CBP’s electronic medical records system, Border Patrol’s system that records apprehensions and custodial activities, and OFO’s system that records data.[5] We analyzed these data to determine the extent to which CBP provided medical assessments to medically at-risk groups as required by CBP’s medical directives and guidance. We also reviewed the timeliness and frequency of enhanced medical monitoring for medically high-risk individuals in custody, as required under 2023 CBP guidance.
To assess data reliability, we discussed data collection methods with agency officials, conducted electronic testing to identify potential anomalies, and reviewed agency procedures for data quality. Although some records had missing data in certain fields or could not be matched across systems for selected analyses, we determined that the data were sufficiently reliable for the purposes of assessing the extent to which individuals received certain medical care, as well as identifying possible trends and patterns in CBP’s provision of medical care. We assessed CBP’s medical care activities against its medical care policies and guidance, such as CBP’s 2019 Enhanced Medical Directive and June 2023 Medical Process Guidance.[6]
To assess CBP’s contract management and oversight, we reviewed contract file documentation for the three medical services contracts, which were awarded to the same contractor and in effect from fiscal years 2021 through 2025. This review included in-depth examinations of contracts and modifications for the 2020 contract (which was in effect in fiscal years 2021 through 2023) and the Bridge I contract, and modifications for the Bridge II contract through December 2024 (the latest modification we had at the time of our analysis). We also examined statements of work issued through July 2025, contracting officer’s representatives’ appointment letters, and acquisition plans. (The Bridge II contract was in effect during our review.) We reviewed contractor past performance evaluations, contractor staffing data, and documentation of CBP oversight activities, such as the Acquisition Management Division’s site visit checklist. We compared CBP’s contract management and oversight duties to DHS guidance, federal internal controls, and Federal Acquisition Regulation (FAR) provisions related to the contract ceiling price, exercising options, and contract data elements.[7] In addition, we compared CBP’s contractor past performance evaluation documentation for the medical services contracts to relevant FAR provisions and government-wide guidance. We also interviewed DHS and CBP officials responsible for contract administration and oversight of medical services. Appendix I provides more information about our objectives, scope, and methodology.
We conducted this performance audit from March 2024 to January 2026 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Background
From fiscal years 2021 through 2024, CBP experienced fluctuations in the number of individuals it encountered along the southwest border, as shown in figure 1. For example, CBP reported encountering about 1.7 million individuals along the southwest border in fiscal year 2021 and about 2.1 million in fiscal year 2024. For the first 10 months of fiscal year 2025 (through July 2025), the number of encounters along the southwest border decreased to a total of 422,325, according to CBP data.
Figure 1: U.S. Customs and Border Protection (CBP) Total Encounters Along the Southwest Land Border from Fiscal Years 2021-2024
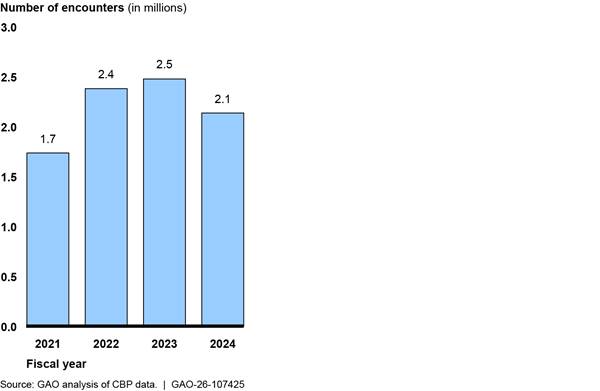
Note: CBP defines encounters as the sum of (1) noncitizens who are not lawfully in the U.S. whom Border Patrol apprehended; (2) noncitizens encountered at ports of entry whom Office of Field Operations determined to be inadmissible; and (3) noncitizens processed for expulsions as part of CBP’s efforts to aid the Centers for Disease Control and Prevention in enforcing its authority under 42 U.S.C. § 265. See 42 U.S.C. § 268(b); 42 C.F.R. § 71.40. Title 42 expulsions began on March 21, 2020, and ended on May 11, 2023. The number of encounters could reflect unique individuals encountered more than once.
In January 2025, the President took several actions on border security and immigration. For example:
· In Proclamation 10888, Guaranteeing the States Protection Against Invasion, the President declared an invasion at the southern border of the U.S., and directed that entry of noncitizens there be suspended. The President also restricted certain noncitizens from invoking provisions of the Immigration and Nationality Act, such as those related to asylum, that would permit their continued presence in the U.S.[8]
· In
Executive Order 14165, Securing Our Borders, the President directed the
Secretary of Homeland Security to detain, to the fullest extent permitted by
law, noncitizens apprehended for violations of immigration law until their
successful removal from the U.S. and to terminate the practice sometimes referred
to as “catch and release.”[9]
Under that discretionary practice, CBP exercised its discretion to release or
parole certain noncitizens under certain conditions, including when other
agencies lacked detention space.[10]
According to Border Patrol officials, as of January 20, 2025, only the Border
Patrol’s Deputy Chief of Operations can approve requests for Border Patrol
personnel to release individuals into the U.S. for any reason, including
extreme medical conditions.
CBP Processing and Medical Care for Individuals in Custody
Within CBP, Border Patrol is responsible for patrolling the areas between ports of entry to prevent individuals and goods from entering the U.S. illegally. Border Patrol may apprehend individuals between ports of entry for suspected illegal entry, which is a civil immigration offense and may also be prosecuted criminally. Border Patrol may also encounter and arrest individuals suspected of or known to have committed other criminal activities, such as drug or human trafficking. OFO is responsible for operating U.S. ports of entry. This includes inspecting all people who arrive at a port of entry to determine their citizenship or nationality, immigration status, and admissibility. After determining an individual’s admissibility into the U.S. or while making an apprehension, respectively, OFO and Border Patrol may hold individuals in short-term custody in holding facilities located at ports of entry, Border Patrol stations, and other locations to complete processing and determine the next appropriate course of action.
|
U.S. Customs and Border Protection (CBP) Health Interview Questions CBP requires contracted medical or CBP personnel to use the CBP health interview form, Form 2500, to ask individuals in custody along the southwest border about their medical history and current medical issues, including any mental health issues or thoughts about hurting themselves. The form includes questions about prescription medications and other drug use; allergies; pregnancy; nursing; illness or injuries; pain; skin rashes; contagious diseases; fever symptoms; cough or breathing symptoms; and nausea, vomiting, or diarrhea symptoms. Source: CBP documentation. | GAO‑26‑107425 |
While processing individuals, contracted medical or CBP personnel conduct verbal health interviews—13 scripted questions to identify potential medical issues. For more information about these questions, see the sidebar.
Contracted medical personnel on-site at CBP facilities may also conduct medical assessments or medical encounters:
· Medical assessments include evaluating an individual’s medical history and current vitals, reviewing any symptoms, and conducting a physical exam. Contracted medical personnel are to record potential medical issues and other information they collect during medical assessments in CBP’s electronic medical records system.
· Medical encounters are evaluations to address a specific medical issue, injury, or illness identified during health interviews, medical assessments, or throughout an individual’s time in custody. During medical encounters, contracted medical personnel record the individual’s diagnoses in CBP’s electronic medical records system, which automatically assigns them a risk designation based on an approved diagnosis list.
CBP policy requires additional care for detained individuals at higher medical risk, as discussed below. See figure 2 for an example of an office at a CBP facility where contracted medical personnel conduct medical assessments or medical encounters.

Individuals detained in CBP custody may receive medical care at various points after being encountered at the southwest border. Figure 3 shows the processing steps for individuals Border Patrol apprehended between ports of entry after crossing the southwest border and the processing steps for individuals OFO found inadmissible at ports of entry.
Figure 3: Processing Steps for Individuals Encountered Between Ports of Entry by Border Patrol and at Ports of Entry by Office of Field Operations (OFO)
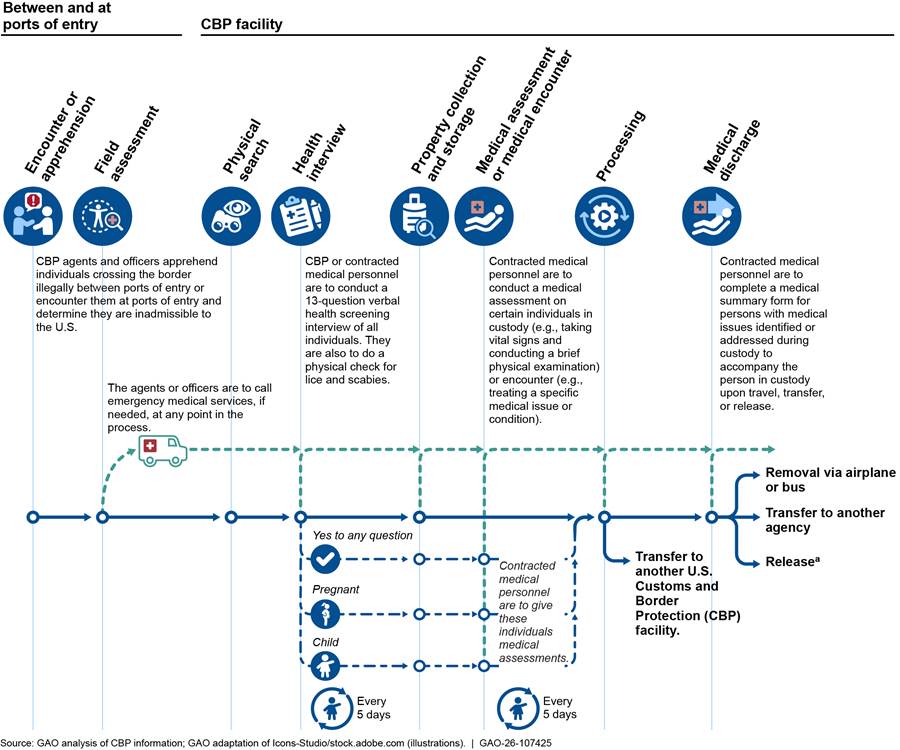
aIn Executive Order 14165, Securing Our Borders, the President directed the Secretary of Homeland Security to detain, to the fullest extent permitted by law, noncitizens apprehended for violations of immigration law until their successful removal from the United States and to terminate the practice sometimes referred to as “catch and release.” Exec. Order No. 14165, 90 Fed. Reg. 8467 (Jan. 20, 2025). Under that discretionary practice, CBP exercised its discretion to release or parole certain noncitizens under certain conditions, including when other agencies lacked detention space. As of July 2025, CBP officials told us they only release individuals in rare, emergent circumstances. Additionally, under CBP’s 2023 medical process guidance, contracted medical personnel are to conduct medical assessments on all children 12 and under and unaccompanied children every 5th day in custody. At any point in the process, individuals can be transferred to or between CBP facilities. When that happens, individuals may receive health interviews and medical assessments at one or multiple locations.
Medical Services Contracts
CBP has used contracted personnel to provide health screenings, limited onsite diagnoses, and treatment of basic medical conditions at its facilities along the southwest border since 2015. At that time, CBP contracted for medical services at three Border Patrol facilities. CBP expanded the contracts over time, with a peak of 79 facilities along the southwest border in July 2024. In May 2025, CBP reduced the number to 44, which CBP officials attributed, in part, to decreases in the number of individuals along the southwest border.
CBP cumulatively obligated over $1 billion from fiscal year 2016 through August 2025 for its medical services contracts, according to federal procurement data. Table 1 provides a breakdown of the obligation information as of August 2025.[11]
Table 1: Obligations for U.S. Customs and Border Protection Medical Services Contracts in Effect, Fiscal Year 2016–August 2025
|
Contracts |
Total obligations as of August 2025 |
Total period of performance as of August 2025 |
|
|
2015 Medical Services Contract |
$113,399,862.53 |
September 30, 2015–September 29, 2020 |
|
|
2020 Medical Services Contract |
$421,385,258.87 |
September 30, 2020–March 29, 2023 |
|
|
2023 Bridge I Medical Services Contract |
$197,988,653.01 |
March 30, 2023–November 29, 2023 |
|
|
2023 Bridge II Medical Services Contract |
$402,641,997.58 |
November 30, 2023–August 27, 2025a |
|
|
Total |
|
$1,135,415,771.99 |
Not applicable |
Source: GAO summary of federal procurement data. | GAO‑26‑107425
Note: The 2015 contract includes six task orders that were placed under a General Services Administration blanket purchase agreement. The 2020 contract and the two bridge contracts were task orders placed under a federal supply schedule contract established by the Department of Veterans Affairs. Generally, blanket purchase agreements are agreements between agencies and vendors with terms in place for future use to fulfill repetitive needs; funds are obligated when orders are placed. Similarly, federal supply schedules are contracts awarded to multiple vendors that provide similar products and services. For the purpose of this review, we generally refer to the task orders as “contracts” or “medical services contracts.”
aOn May 30, 2025, CBP’s Office of Acquisition added three additional option periods to the 2023 Bridge II contract to extend the period of performance by 90 days from May 30, 2025, through August 27, 2025, and then extended it again through September 27, 2025. In addition, CBP awarded the Bridge III medical services contract on September 28, 2025, after we provided DHS with our draft report for review and comment. Thus, we did not include the Bridge III contract within the scope of our review.
In September 2020, CBP awarded a contract for medical services to Loyal Source Government Services.[12] Starting in March 2023, CBP executed a series of bridge contracts—all awarded to the incumbent contractor—due to a delay in the award of the next contract.[13] One reason for the delays was bid protests. As of May 2025, the incumbent contractor and other prospective vendors had filed more than 10 bid protests related to the procurement of the next medical services contract. CBP took corrective action in response to the protests, including amending the solicitation and requesting revised quotes from vendors. In the interim, CBP has awarded bridge contracts. The Bridge II contract was in effect through August 27, 2025, at the time of our review.[14]
The DHS Office of the Chief Procurement Officer, Office of Procurement Operations, has been in the process of awarding the next medical services contract since December 2023. At that time, CBP’s Head of the Contracting Activity transferred the source selection and contract award responsibility from CBP’s Office of Acquisition to DHS’s Office of the Chief Procurement Officer, Office of Procurement Operations, due to CBP government officials potentially disclosing unauthorized procurement-sensitive information. See figure 4 for a timeline of key events and decisions related to the recent CBP medical services contracts.
Figure 4: Timeline of U.S. Customs and Border Protection’s (CBP) Medical Services Contracts’ Key Procurement Events and Decisions, September 2020 – May 2025
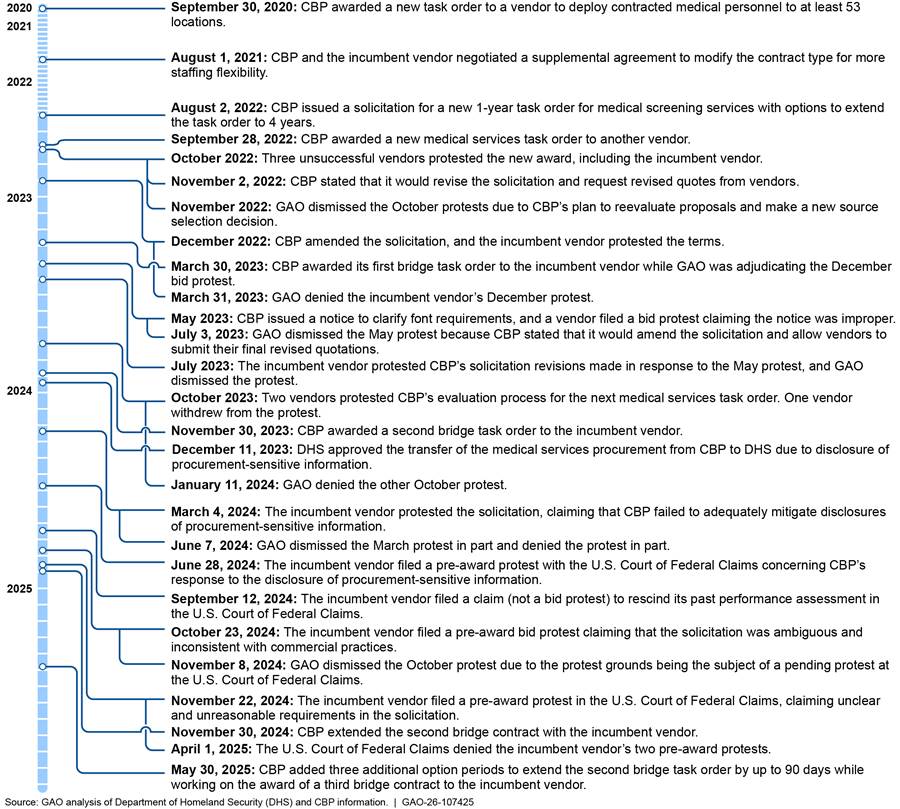
Note: GAO has responsibilities for deciding bid protests, which are separate from its audit activities. 31 U.S.C. § 3552. While there is no government-wide definition for bridge contracts, we have defined it as an extension of an existing contract beyond the period of performance (including base and option years), or an award of a short-term sole-source (noncompeted) contract to the incumbent contractor to avoid a gap in service when an existing contract is set to expire but there is a delay in awarding a follow-on contract.
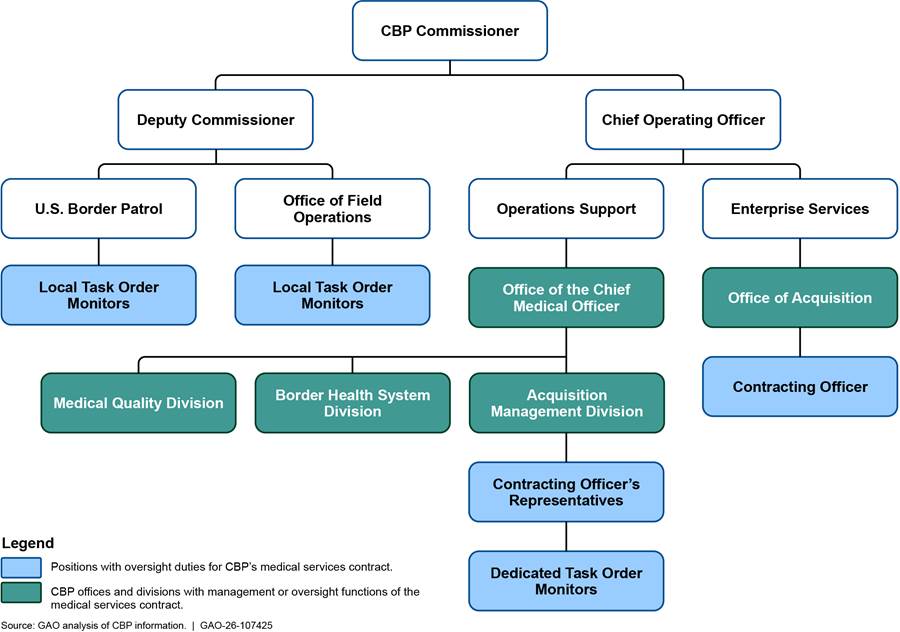
CBP Roles and Responsibilities for Medical Services Management and Oversight
Several CBP offices are responsible for managing and overseeing medical services. CBP’s Office of Acquisition procures goods and services for CBP. Office of Acquisition contracting officers have authority to enter into, administer, and terminate contracts and make related determinations, as well as responsibility to ensure the contractor complies with the contract’s terms and conditions.[15] Contract oversight is largely the responsibility of the contracting officer and the contracting officer’s representatives (COR), if appointed to a particular contract, who assist the contracting officer. Contracting officers may also appoint technical monitors (also referred to as task order monitors) to assist in contract oversight.[16] Task order monitors generally work with CORs.
CBP’s Office of the Chief Medical Officer (OCMO) is responsible for providing medical direction and oversight for CBP’s medical support efforts. Three offices within OCMO play a role in managing CBP’s medical care for individuals in its custody, as shown in figure 5:
· The Border Health System Division is to manage and implement CBP’s policies and guidance related to medical care.
· The Medical Quality Division is to manage and provide oversight of the clinical aspects of medical care, including the contractor’s quality assurance program.
· The Acquisition Management Division is to conduct contractor oversight through CORs and task order monitors. For example, CORs appointed on the medical services contract are to monitor contractor invoices and ensure that background investigation packets are complete.[17]
Figure 5: U.S. Customs and Border Protection (CBP) Offices and Positions with Management or Oversight of Medical Services
CBP Has Developed Medical Care Policies and Guidance, but Has Not Consistently Implemented Them
CBP has developed policies and guidance for providing medical care to individuals in custody along the southwest border. CBP OCMO took several steps to facilitate the implementation of its 2023 medical care guidance across CBP, such as improving the availability of supervising physicians. However, CBP did not consistently ensure that children, pregnant individuals, or sick or injured adults received medical assessments, as required by its guidance. Further, CBP and contracted medical personnel did not consistently implement requirements for medically high-risk individuals in CBP custody, such as ensuring that these individuals are expeditiously processed and receive additional medical checks. We also found that CBP has limited oversight into medical care provided to individuals at facilities without contracted medical personnel. Furthermore, CBP personnel did not consistently provide individuals their medical records and prescriptions when they left custody, as required by CBP policy.
CBP Developed Policies and Guidance for Providing Medical Care to Individuals in Custody
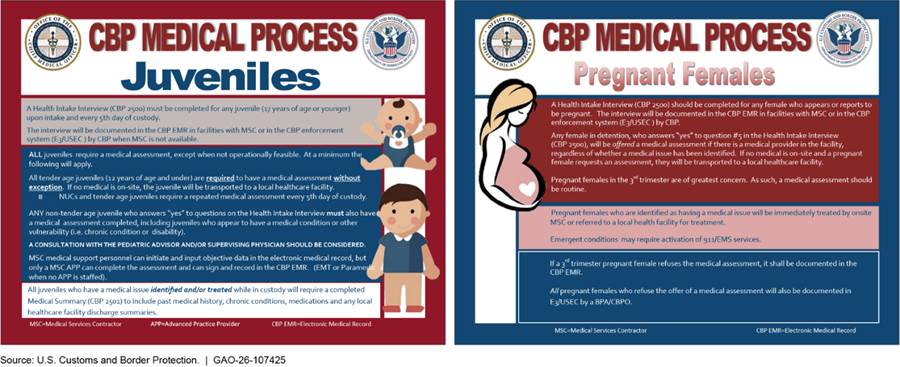
CBP has developed policies and guidance related to the medical care that CBP and contracted medical personnel are to provide individuals detained in its short-term holding facilities, as shown in Table 2. According to OCMO officials, CBP made several improvements to its medical care guidance for individuals in custody after the death of an 8-year-old girl in CBP custody in May 2023. For example, CBP developed medical process guidance in June 2023 and an addendum with additional medical care and monitoring requirements across CBP in October 2023. This addendum includes risk designations based on individuals’ medical status.
Table 2: Overview of U.S. Customs and Border Protection’s (CBP) Key Policies and Guidance on Medical Care for Individuals in Custody Along the Southwest Border as of August 2025
|
Document and date issued |
Medical process requirements |
|
National Standards on Transport, Escort, Detention, and Search (TEDS) (2015) |
· CBP personnel generally should not detain individuals for longer than 72 hours. Personnel are required to monitor detention areas; visually inspect individuals for signs of injury, illness or other physical or mental concerns; report any injury or illness; and ensure medication and medical documentation accompanies individuals in custody when they are transferred. CBP personnel should also document observed or reported injuries or illnesses in the appropriate electronic system of record and provide or seek appropriate medical care in a timely manner. |
|
CBP Directive No. 2210-004 Enhanced Medical Support Efforts (December 2019) |
· CBP or contracted medical personnel must conduct health interviews for all children in custody (17 years old and under) along the southwest border. Additionally, individuals with observed medical issues are to receive a health interview or a medical assessment or be referred to a local health unit. · CBP personnel must ensure that contracted medical personnel conduct a medical assessment for: · Children aged 12 and under, · Adults who responded “yes” to one of the health interview questions asking if they have had medical issues, including individuals who are pregnant, or · Individuals with a known or reported medical concern. |
|
CBP Office of the Chief Medical Officer Medical Process Guidance (June 2023) |
· In addition to the requirements noted above related to health interviews, CBP or contracted medical personnel must document health interview responses for individuals who: · Responded with a “yes” on an initial verbal health interview, including pregnant individuals, or · Have a potential illness, injury, medication requirement, or other medical issue. · All children are to receive a health interview every 5th day in custody. · The above individuals, as well as children aged 13 and above, are also required to receive a medical assessment (which includes checking vitals, reviewing symptoms, and conducting a physical exam) from contracted medical personnel or a local health provider within 24 hours of arrival. Additionally, contracted medical personnel are to conduct medical assessments on all children 12 and under and unaccompanied children every 5th day in custody. · Contracted medical personnel are to conduct medical encounters to evaluate and treat acute medical issues onsite, as appropriate. |
|
CBP Office of the Chief Medical Officer Medical Process Guidance Annex A: Elevated in-Custody Medical Risk (October 2023) |
· When completing a medical assessment or a medical encounter, contracted medical personnel must select a diagnosis in the electronic medical records system, which automatically assigns a risk designation and adds specific care requirements for the individual. CBP developed the following risk designations: · Red—individuals in custody at elevated/high medical risk (e.g., chest pain, heat stroke, abdominal open wound). · Orange—individuals with an acute issue (e.g., an active infection, such as strep or flu) who are receiving treatment. · Yellow—individuals with a well-controlled chronic issue. · Green—individuals with no known medical issues. |
Source: GAO summary of CBP documentation. | GAO‑26‑107425
Note: CBP expanded the medical care requirements in its 2023 guidance, though the new guidance stated it did not replace or supersede the 2019 directive.
CBP Took Various Steps to Implement Aspects of Its Medical Care Guidance
CBP OCMO took several steps to facilitate the implementation of its 2023 medical care guidance. For example, OCMO worked with the medical services contractor to ensure that on-call supervising physicians—pediatric advisors for children or supervising physicians for adults—were available for consultation at all times. Following the death of an 8-year-old girl in May 2023, the DHS Office of Health Security found that the supervising physician contact roster for CBP’s medical services contract was out of date. OCMO officials stated that they requested the medical services contractor resolve this issue by updating the roster. CBP officials stated the contractor subsequently implemented a unified hotline number rather than a roster, where a physician answers calls in a rotating system at all times.[18]
During our 2024 site visits to 28 CBP facilities with contracted medical personnel onsite, personnel at three facilities in Arizona and Texas told us the on-call supervising physicians had sometimes been unavailable in the past. However, they said they had seen consistent improvement in the availability of the physicians to consult on cases for medically high-risk individuals in CBP custody after CBP worked with the contractor to resolve this issue. We requested that the contracted medical personnel call the pediatric advisor or supervising physicians at most of the facilities we visited, and these physicians were available for consultation every time.[19]
Moreover, OCMO and the medical services contractor ensured that CBP locations had requisite medical supplies, as called for in its medical services contract. During our visits to CBP facilities, we observed that the medical supplies contractors needed were available. Contracted medical personnel stated they generally had the medical supplies they needed to provide basic medical care.[20] Figure 6 includes photographs of basic medical supplies (e.g., over-the-counter medications, antiseptics, and bandages) stored at various CBP facilities.

Furthermore, OCMO developed job aids and standard operating procedures to help guide CBP and contracted medical personnel through key steps of the 2023 guidance, as shown in figure 7.
OCMO also began producing internal daily oversight reports related to medical interactions at CBP facilities with contracted medical personnel, such as the number of individuals in custody who received medical assessments and medical encounters. Additionally, OCMO produced monthly reports for DHS’s Office of Health Security with information such as top diagnoses of medically high-risk children and adults. As of March 2025, OCMO’s Border Health System Division was developing a compliance program using data to improve the tracking and monitoring of CBP’s compliance with aspects of its medical care policies and guidance. For example, CBP developed a dashboard to monitor whether children 12 years old and under have received a medical assessment every 5th day they are in custody, as required in CBP’s 2023 medical process guidance.
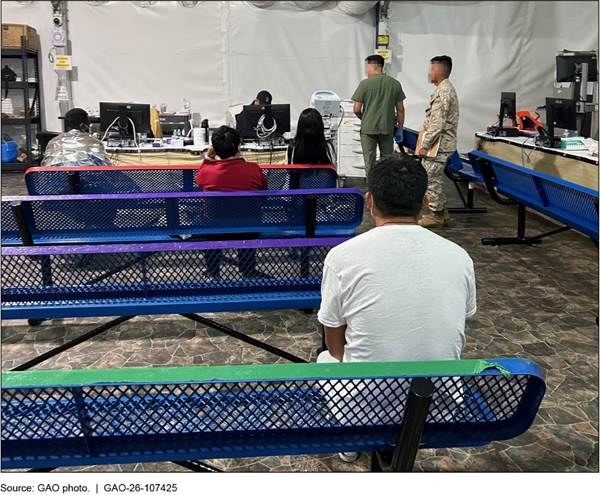
CBP Did Not Consistently Ensure That Individuals in Custody Received Medical Assessments When Required
While in CBP custody, certain individuals are required to receive a medical assessment—a basic physical exam and review of symptoms, vitals, and medical history. However, CBP has not ensured that those individuals in custody consistently receive these assessments. Specifically, CBP’s 2019 directive states that Border Patrol agents and OFO officers must ensure a medical provider conducts a medical assessment for (1) all tender-age children, defined as children 12 years old and under, and (2) all individuals who responded “yes” to one of the questions on the initial health interview, including individuals who are pregnant, along the southwest border.[21] CBP’s 2023 medical guidance expanded these requirements by requiring medical assessments for all children (not just tender-age).[22] Additionally, tender-age children and unaccompanied children must receive a medical assessment every 5 days while in custody. Figure 8 shows individuals waiting for a medical assessment at a CBP facility we visited.
Figure 8: Individuals in U.S. Customs and Border Protection Custody Waiting for a Medical Assessment
Our analysis of data from CBP’s systems found that some individuals in CBP custody did not receive medical assessments as required under the original medical directive (November 2020–July 2023) and the new medical process guidance (August 2023–August 2024).[23]
November 2020–July 2023. We found that less than 50 percent of each group specified by CBP policy to receive a medical assessment while in Border Patrol custody received that assessment during this time period. In particular, about 45 percent of tender-age children, 30 percent of pregnant individuals, and 16 percent of other adults with a “yes” health interview response received a medical assessment.
In comparison, tender-age children in OFO custody had much higher rates of completed medical assessments (92 percent). However, 49 percent of pregnant individuals and only 4 percent of adults with a “yes” health interview response in OFO custody received medical assessments during this time period.[24] See figure 9 for more information regarding the extent to which individuals received medical assessments while in Border Patrol or OFO custody.
August 2023–August 2024. We found that CBP’s implementation of its medical assessment requirement improved across all covered groups since August 2023, particularly among children. For instance, based on our analysis of CBP data, we found that about 98 percent of children in both Border Patrol and OFO custody received a medical assessment from August 2023 through August 2024.
Additionally, among tender-age children and unaccompanied children who remained in Border Patrol or OFO custody for at least 5 days, more than 97 percent of these children received at least one medical assessment for every 5-day period, as required by CBP’s 2023 medical process guidance.
Despite substantial improvements across all groups since the 2019 directive, we found that CBP did not consistently implement its medical assessment policies for adults with a “yes” health interview response and pregnant individuals, as shown in figure 9.
Figure 9: Percentage of Individuals in U.S. Customs and Border Protection (CBP) Custody Who Received a Medical Assessment as Required Per CBP Policy and Guidance, November 2020–August 2024
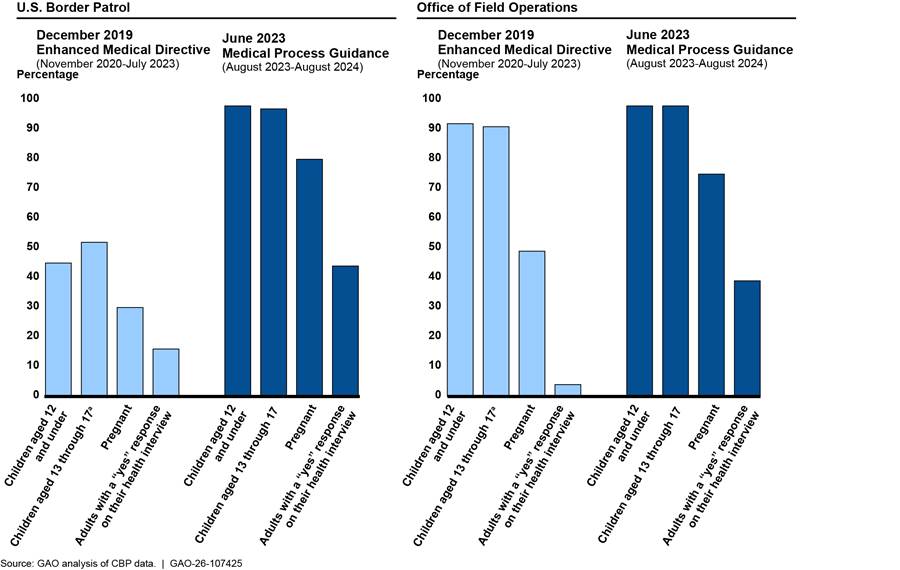
aChildren aged 13 and above were not required to receive a medical assessment under the 2019 directive but were under the 2023 guidance.
One reason that CBP did not consistently implement its medical assessment policy is that contracted medical personnel were sometimes performing medical encounters (evaluations to address acute medical concerns) instead of the required medical assessments. Medical assessments and medical encounters contain many of the same elements, but their purposes are different. According to CBP policy and guidance, medical assessments are required for certain individuals in custody, whereas medical encounters are meant to address an acute medical issue experienced during someone’s time in CBP custody. When individuals receive a medical encounter instead of a medical assessment, they receive some, but not all, of the medical care required by CBP policy and guidance. Notably, medical assessments capture an individual’s medical history while medical encounters do not. As a result, in the event of an emergent medical issue, CBP may not have all the medical information it needs to address the issue effectively.
During our site visits to facilities across Arizona, California, and Texas, contracted medical personnel from 15 of the 28 facilities indicated they performed medical encounters to fulfill the medical assessment requirement or did not understand some of the differences between the two. For example, some contracted medical personnel at sites we visited stated they conduct medical assessments for children and pregnant individuals and conduct medical encounters for any individual who says “yes” to a health interview question. This is not consistent with CBP’s guidance, which states children, pregnant individuals, and individuals with a “yes” to a health interview question are all to receive a medical assessment (a more general examination) and then receive a medical encounter (to address a more specific or acute medical issue), if appropriate.
A senior OCMO official stated that distinguishing between medical assessments and medical encounters is important for medical processing and oversight purposes. This is because OCMO officials use electronic medical records data on medical assessments and medical encounters to assess needs in CBP facilities. For example, a tender-age child with multiple medical assessments has likely been in custody for a longer period, whereas a child with multiple medical encounters is likely ill and could require greater medical attention. As such, it is important for individuals in custody to receive the medical assessments and medical encounters outlined in CBP policy and guidance, according to the OCMO official.
Due to the impact this confusion could have had on the data, we analyzed data from CBP’s systems from August 2023 to August 2024 to determine the extent to which individuals received either a medical assessment, a medical encounter, or both. For this time period, we found 98 percent of children, 96 percent of pregnant individuals, and 86 percent of other adults with a “yes” health interview response received either a medical assessment or a medical encounter (or both), suggesting that contracted medical providers may have performed medical encounters in lieu of medical assessments for some individuals.
Following discussions with us about the issues we identified, in July 2025, CBP officials stated that they re-sent CBP’s medical process guidance to the medical services contractor and planned to meet with the contractor’s leadership to reiterate the differences between medical assessments and medical encounters. Communicating this information to the contractor’s leadership is a positive initial step. By ensuring contracted medical personnel in the field, who are responsible for implementing the guidance, receive these clarifications and understand the difference between medical assessments and medical encounters and operational reasons concerning their different usages, OCMO will be better positioned to monitor and assess medical needs in CBP facilities. By clarifying the differences and reasons through additional training or guidance, CBP will also ensure that individuals in custody receive the medical care required by CBP policy and guidance.
Our analysis of data from CBP’s systems also found that some individuals in CBP custody received neither a medical assessment nor a medical encounter under the 2023 medical process guidance from August 2023 through August 2024. Specifically, 14 percent of adults with a “yes” health interview response received neither a medical assessment nor a medical encounter (more than 5,000 individuals). Additionally, despite the high rates of children and pregnant individuals who received either a medical assessment or a medical encounter, over 9,000 children and pregnant individuals received neither one. See table 3 for more information on the numbers of individuals who did not receive either one.
Table 3: Individuals in U.S. Customs and Border Protection (CBP) Custody Who Did Not Receive a Medical Assessment or a Medical Encounter from Contracted Medical Personnel, August 2023-August 2024
|
Population |
Percentage who did not receive a medical assessment or a medical encounter |
|
Children under 13 |
2% (5,454 out of 300,490) |
|
Children aged 13 through 17 |
3% (3,650 out of 143,928) |
|
Pregnant individuals |
4% (260 out of 5,969) |
|
Other adults with a “yes” health interview response |
14% (5,632 out of 41,510) |
Source: GAO analysis of CBP data. | GAO‑26‑107425
Note: Contracted medical personnel conduct medical assessments on certain individuals, which include a physical exam and an evaluation of an individual’s medical history, current vitals, and symptoms. Medical encounters are evaluations to address a specific medical issue, injury, or illness identified during health interviews, medical assessments, or throughout an individual’s time in custody. CBP’s June 2023 medical process guidance requires medical assessments for all children and individuals who responded “yes” to one of the questions on the initial health interview, including pregnant individuals. While one of the CBP health interview questions asks if individuals are pregnant, we use “other adults with a ‘yes’ health interview response” to refer to non-pregnant adults with an affirmative response to any other health interview question.
CBP officials stated that some individuals may not have received either a medical assessment or a medical encounter due to administrative oversight. For example, CBP officials stated they may have missed providing a medical assessment or a medical encounter to individuals when there were large numbers of encounters along the southwest border. Additionally, a CBP official stated that there may have been a small number of instances where contracted medical personnel conducted a medical assessment or a medical encounter but did not document it.
Additionally, there may have been brief periods where the electronic medical records system was down, according to officials. Consequently, contracted medical personnel would have to document the assessment or the encounter on paper and may not have subsequently recorded that in the electronic medical records system. They also noted that some individuals may have declined medical service, been referred to a local healthcare facility, or were not in custody long enough to receive medical care.
At the time of our review, OCMO’s oversight reports detailed the number of medical assessments contracted personnel performed, but did not include information on whether individuals who were required to receive medical assessments actually received them. After discussions with us about the issues we identified, in July 2025 CBP developed new tools to help oversee whether these individuals correctly received medical assessments as required. For example, OCMO developed an observation checklist and an onsite assessment tool for its personnel to utilize on visits to CBP facilities, allowing OCMO personnel to record whether they observe contracted medical personnel providing medical assessments as required. OCMO also developed a tool to review medical records for individuals in custody and assess whether they received required medical care, including medical assessments. These new tools should help OCMO collect consistent information during visits and records reviews.
However, OCMO did not explain how it will use these tools to systematically oversee facilities across the southwest border. For example, OCMO did not include a plan for implementing these tools, including how many oversight visits they will conduct, how many medical records they will review, or how they will select facilities and medical records to ensure individuals in custody received medical assessments when required.
Standards for Internal Control in the Federal Government calls for agencies to design control activities, including mechanisms that enforce management’s directives, to achieve objectives and respond to risks.[25] Without an oversight mechanism to ensure individuals receive medical assessments as required by CBP policy and guidance, CBP cannot be assured that it is aware of the medical needs of the children, pregnant individuals, and adults with an injury or illness in its custody, or that contracted medical personnel provided required follow-on medical evaluations for known medical needs.
CBP Did Not Consistently Implement Policies and Guidance for Processing and Monitoring Medically High-Risk Individuals
CBP Did Not Expeditiously Process Some Medically High-Risk Individuals
CBP policy requires personnel to expedite processing for medically high-risk individuals, but CBP did not do so for all such individuals during the period we reviewed. More specifically, CBP’s National Standards on Transport, Escort, Detention, and Search (TEDS) states that CBP personnel should generally not detain individuals for longer than 72 hours.[26] TEDS also states that, when operationally feasible, CBP personnel should expeditiously process at-risk individuals to minimize their time in CBP custody. Under TEDS, agents and officers may determine that an individual in custody is at-risk based on an observed or reported serious physical or mental injury or illness.[27]
In May and October 2023, the Acting CBP Commissioner issued memorandums reaffirming that CBP personnel should consider expeditiously processing at-risk or medically fragile individuals. The May 2023 memorandum also stated that CBP personnel should consider releasing at-risk or medically fragile individuals with a Notice to Appear (a charging document to appear in immigration court) to minimize their time in CBP custody.[28]
In May 2025, CBP rescinded these memorandums, stating that they were misaligned with current agency guidance and new immigration enforcement priorities.[29] According to one OCMO official, the rescinded memorandums conflicted with the January 2025 Executive Order restricting the practice of releasing individuals in CBP custody with a Notice to Appear.[30] However, the May 2025 memorandum states that CBP personnel should continue to adhere to TEDS.
During our 2024 site visits to CBP facilities in Arizona, California, and Texas, CBP personnel stated that they generally prioritized processing high-risk individuals, such as individuals with medical conditions, to minimize their time in custody. Our analysis of CBP data from October 2023 through August 2024 supported these statements. We found that CBP held medically high-risk individuals (defined as individuals designated “red” under CBP’s October 2023 medical process guidance addendum) in custody for approximately 48 hours on average, which is less than the 72-hour standard identified in TEDS. CBP also processed medically high-risk individuals on average nearly twice as fast as low-risk individuals in custody.[31]
However, of the individuals designated medically high-risk in CBP custody from October 2023 through August 2024, we found that 17 percent were in custody for 72 hours or more (1,123 out of 6,755).[32] For more information about the time medically high-risk and low-risk individuals were in CBP custody, see figure 10.
Figure 10: Time-in-Custody for Individuals Designated Medically High-Risk versus Low-Risk in U.S. Customs and Border Protection (CBP) Custody, October 2023-August 2024
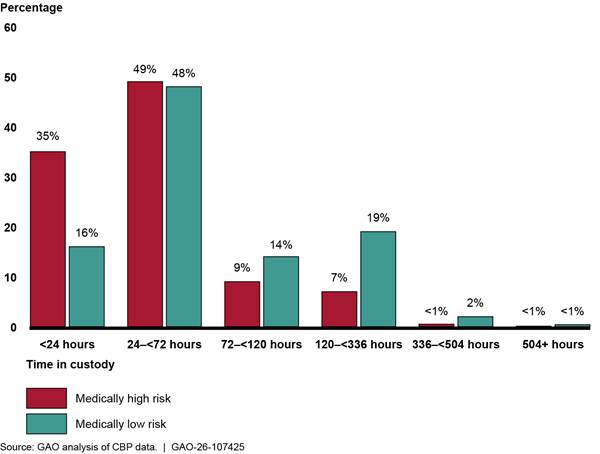
Note: Contracted medical personnel designate whether an individual presents high in-custody medical risk while in CBP custody based on certain diagnoses including chest pain, heat stroke, or an abdominal open wound, among other things. Therefore, this analysis only includes individuals that saw contracted medical personnel for these risk designations while in CBP custody. We compared individuals who were only designated “red” medical risk, the highest level of risk, throughout their time in custody (6,755 individuals) with individuals who were only designated “green,” the lowest level (58,713 individuals). We did not include individuals whose risk level changed during their time in custody (e.g., individuals who were initially designated red and were later downgraded to lower levels of risk, such as orange, yellow, or green).
To ensure that Border Patrol and OFO personnel are aware of medically at-risk individuals in their facilities, CBP officials stated they linked the electronic medical records system and processing systems in 2024. This linkage means that if a contracted medical provider designates someone as medically high-risk in the electronic medical records system, they are also marked at-risk in the Border Patrol and OFO processing systems.[33]
OCMO and Border Patrol officials stated that some individuals designated medically high-risk may be safe to remain in custody for longer periods of time and therefore do not need to be expeditiously processed. Officials stated that “medically high-risk” is a broad category and encompasses individuals with a wide variety of conditions and injuries. For example, OCMO officials stated that a child with autism would be designated medically high-risk but would not necessarily require expeditious processing if provided appropriate accommodations while in custody. However, CBP has not documented the specific factors Border Patrol and OFO personnel should consider when determining whether medically high-risk individuals should be considered at-risk for the purpose of expeditious processing.
Furthermore, CBP officials stated that other factors outside of CBP’s control affect how quickly they can process individuals in custody. For example, if an individual in custody is considered a national security risk or expressed a fear of returning to their home country, CBP may be required to follow other processes that may lengthen an individual’s time-in-custody, regardless of their medical status. According to one official, an individual being in the hospital may also affect their time-in-custody.
Border Patrol officials also said encounters along the southwest border were high during the period we examined (October 2023 through August 2024). Border Patrol often had to wait for flights to remove individuals or for other agencies like U.S. Immigration and Customs Enforcement to take custody of individuals, resulting in longer times in CBP custody. As such, they stated that Border Patrol agents sometimes made their own determinations about whom to prioritize for processing based on, for instance, the severity of the conditions or injuries that led contracted medical personnel to designate individuals as medically high-risk.
In July 2025, OCMO officials told us they communicate with Border Patrol and OFO on certain medical cases based on the severity of the individual’s medical condition, the availability of support required to manage that condition, and the capabilities of onsite medical care. However, CBP has not documented these factors in policy or guidance, nor communicated them to the CBP personnel responsible for processing individuals.
Medically high-risk individuals are the most vulnerable population within CBP custody, according to CBP guidance. Clearly documenting what factors Border Patrol and OFO personnel should consider when determining whether an individual should be considered at-risk for the purpose of expeditious processing would help ensure personnel are consistently implementing the expedited processing requirement, when it is possible to do so.
Some CBP Locations Did Not Fully Implement Medical Care Requirements for Medically High-Risk Individuals
CBP guidance includes additional requirements for caring for medically high-risk individuals while they are in custody, but CBP did not fully implement these requirements across facilities with contracted medical personnel. According to CBP’s medical process guidance, contracted medical personnel should conduct medical monitoring checks at least every 4 hours on medically high-risk individuals and identify these individuals with a red wristband.[34] According to CBP officials, the red wristbands help ensure that medically high-risk individuals are visible to everyone, including both contracted medical personnel and CBP personnel who are observing and monitoring individuals in custody, as shown in figure 11.
Figure 11: A Red Wristband Requirement for Medically High-Risk Individuals in U.S. Customs and Border Protection (CBP) Custody
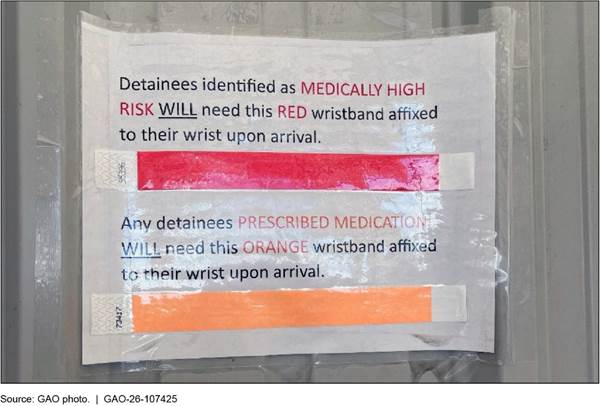
Note: Despite the text associated with the orange wristband above, CBP policy does not require wristbands for individuals who require prescribed medication. Some facilities we visited used other colors for this purpose, while other facilities did not use wristbands for this purpose at all.
During our 2024 site visits to CBP facilities in Arizona, California, and Texas, we found that some facilities were following this guidance, while others were not. For example, contracted medical personnel at the facilities we visited generally stated that they performed medical monitoring checks on medically high-risk children every 4 hours. However, contracted medical personnel reported differing intervals for enhanced medical monitoring checks of medically high-risk adults. For instance, at 7 of the 28 facilities with contracted medical personnel that we visited, contracted medical personnel stated that they conduct medical monitoring checks on medically high-risk adults in custody every 4 hours, as required. However, contracted medical personnel at five facilities stated they conduct checks on medically high-risk adults every 8, 12, or 24 hours.[35]
Our analysis of data from CBP’s systems from October 2023 through August 2024 found inconsistent implementation of the additional medical monitoring checks required for adults and children in custody.[36] Specifically, we found medically high-risk children and adults received the required enhanced medical monitoring checks every 4 hours approximately 43 percent of the time.[37] Additionally, about one third of the facilities we visited did not use red wristbands to identify medically high-risk individuals and personnel at several others reported differing understandings of the red wristbands’ meaning. Specifically, we observed personnel from 11 of 28 facilities using red wristbands to identify and monitor high-risk individuals in custody, while personnel at 10 facilities did not. Furthermore, at seven facilities, the contracted medical personnel stated they use red wristbands to identify and monitor high-risk individuals, but Border Patrol agents or OFO officers at those facilities did not know what the bands were for or stated they did not use them (and thus would not be able to more closely monitor these individuals).[38]
OCMO officials stated that CBP personnel may be unfamiliar with the requirements for medically high-risk individuals in custody because it is rare to encounter such individuals at CBP facilities across the southwest border. For instance, one CBP official estimated they had seen no more than 20 medically high-risk individuals in custody across the southwest border per day in March 2025. The CBP officials also stated that it is the contracted medical personnel’s responsibility to diagnose and designate these individuals, put the red wristbands on them, and conduct the appropriate medical monitoring checks. During our site visits, we observed reminders in the electronic medical records system that reminded contracted medical personnel of these requirements.
At the time of our review, OCMO’s oversight mechanisms did not allow it to monitor whether CBP and contracted medical personnel have implemented all of the requirements for medically high-risk individuals in custody. For example, OCMO tracked the total number of medical monitoring checks individuals received but did not monitor whether the frequency of the checks complied with its guidance. For example, it did not monitor if a medically high-risk individual in custody received a medical monitoring check every 4 hours.
As previously mentioned, in July 2025 CBP developed an observation checklist and an onsite assessment tool for OCMO officials’ site visits to CBP facilities. The checklist and tool include checks and questions to assess the extent to which medically high-risk individuals receive required care. For example, the observation checklist requires personnel to observe whether contracted medical personnel are monitoring medically high-risk individuals at appropriate intervals and distributing red wristbands as required. OCMO also developed a medical records review tool, which assesses compliance with various medical care requirements, including whether the individual was assigned an appropriate risk designation and whether contracted medical personnel contacted the supervising physician or pediatric advisor for medically high-risk individuals. Additionally, OCMO developed a dashboard listing the medically high-risk individuals in custody along the southwest border, their diagnoses, and the date and time of their most recent medical monitoring check. This could allow OCMO to identify, on a case-by-case basis, individuals who are overdue for medical monitoring checks at a particular point in time.
Developing the tools and dashboard are positive steps, since they will provide important information to inform OCMO’s oversight efforts. However, OCMO did not explain how it will use the tools and dashboard to systematically oversee medical care for medically high-risk individuals in custody. For example, OCMO did not explain how many oversight visits they will conduct, how many medical records they will review, or how they will select facilities and medical records for review. Furthermore, OCMO did not explain how it will use the dashboard to systematically assess whether medically high-risk individuals received their medical monitoring checks on time.
Standards for Internal Control in the Federal Government call for agencies to design control activities, including mechanisms that enforce management’s directives, to achieve objectives and respond to risks.[39] Developing and implementing an oversight mechanism to ensure contracted medical personnel consistently implement CBP’s additional requirements for medically high-risk individuals, such as the 4-hour medical monitoring checks and red wristbands, would help CBP better ensure these individuals are receiving required care and that personnel are monitoring their medical conditions.
CBP Improved its Ability to Monitor Whether Physicians Were Contacted for Certain Medically At-Risk Individuals
During our review, we found that CBP’s electronic medical records system did not have accurate records regarding whether contracted medical personnel contacted supervising physicians (physicians on-call). However, CBP recently improved the system to allow for better monitoring. CBP’s 2023 medical process guidance states that contracted medical personnel must contact a supervising physician when they determine that an adult in custody is medically high-risk. During our review, contracted medical personnel could not input whether they contacted a supervising physician in the electronic medical records system because the field was automatically populated to “Yes” and the response could not be changed—even if they did not call the physician, according to CBP officials.[40]
CBP officials stated they intentionally locked this field in the system in October 2023 due to concerns that contracted medical personnel were not consistently calling supervising physicians as required. Specifically, officials stated that they decided to lock the field to help contracted medical personnel understand that calling the supervising physician is mandatory. One CBP official indicated the contracted medical personnel could include a note in a free-text field if they did not call the supervising physician.
However, after discussions with us in July 2025, OCMO revised its electronic medical records system to ensure that contracted medical personnel could accurately input whether they called a supervising physician. By allowing contracted medical personnel to accurately input this information, CBP improved its ability to collect quality information and accurately assess whether contracted medical personnel contacted the supervising physician for medically high-risk individuals in CBP custody, as required. This should help improve CBP’s awareness of day-to-day clinical operations and provide CBP greater assurance that supervising physicians provided contracted medical personnel guidance on cases involving serious injury or illness.[41]
CBP Has Limited Oversight into the Medical Care of Individuals at Facilities Without Contracted Medical Personnel
CBP has limited oversight into medical care provided to individuals at facilities without contracted medical personnel. CBP’s 2023 medical process guidance states that if there are no contracted medical personnel at a CBP facility, individuals in custody at that facility who are required to receive a medical assessment may be referred to a local medical provider (e.g., an urgent care facility or a hospital). Additionally, that guidance states individuals with life-threatening or emergent medical needs should be referred to a local medical provider. However, OCMO officials stated that if a CBP facility does not have contracted medical personnel, they generally cannot monitor whether an individual in custody there received a medical assessment. This is because OCMO’s oversight reports—which are based on the electronic medical records system data populated by contracted medical personnel—do not include facilities without contracted medical personnel.
Specifically, OCMO personnel track and monitor daily reports on medical interactions at facilities with contracted medical personnel, such as the number of individuals in custody that received medical assessments, medical encounters, and medical checks. They also monitor data on the number of individuals contracted medical personnel see and refer to local hospitals for serious conditions. However, these reports do not include information on the extent to which individuals at facilities without contracted medical personnel received the medical care required by CBP policy and guidance, such as medical assessments, at local hospitals or urgent care facilities.
As CBP has reduced the number of facilities with contracted medical personnel in 2025, the number of facilities that OCMO does not monitor has grown.[42] One OCMO official stated this has not yet created oversight challenges because the overall number of encounters and individuals in CBP’s custody is low. The official stated that OCMO can check whether specific individuals received an off-site medical assessment or medical encounter by checking whether an individual left CBP’s facility, based on the individual’s records in the Border Patrol or OFO processing systems. However, this would require them to look at specific records of individuals in custody and OCMO officials were not systemically monitoring these records.
CBP officials noted that CBP needs to determine how to ensure individuals in custody at facilities without contracted medical personnel receive required medical care. For example, an OCMO official stated that if encounters along the southwest border rose, they would likely need to consider how to revise their monitoring reports to include care at local medical facilities. OCMO officials stated that they also communicate with CBP components as needed about specific individuals in custody. However, the component outreach is ad hoc and only occurs when the component determines it may need assistance from OCMO. These efforts do not allow OCMO to monitor whether individuals at facilities without contracted medical personnel, such as sick adults or pregnant individuals, received required medical assessments from a local health provider.
Standards for Internal Control in the Federal Government state agencies should use quality information to monitor whether they are achieving their objectives.[43] Without including information in its monitoring reports about facilities without contracted medical personnel and individuals who received medical care at local medical facilities, CBP does not have complete, quality information to ensure all individuals in its custody received the medical care required by guidance. Furthermore, without tracking this information, CBP does not have insight into the medical care individuals receive, if any, at facilities without contracted medical personnel CBP-wide.
CBP Did Not Consistently Provide Required Medical Documentation to Individuals Leaving CBP Custody
When individuals leave CBP’s custody, whether through release or transfer to another agency, CBP policy requires that they receive documentation of their medical records and medication needs. However, CBP has not consistently provided such documents to individuals leaving its custody. More specifically, TEDS states that CBP agents and officers must ensure that medical records accompany individuals transferring out of CBP custody.[44] Additionally, CBP policy and guidance require medical documents and prescriptions in the individuals’ property and in CBP’s files to go with individuals with medical issues transferring to an external agency.[45] If CBP releases or transfers individuals out of its custody before they receive their medication, they must also have a written prescription, according to CBP guidance. CBP provides this documentation by completing a medical summary form, which details an individual’s medical disposition, medication, and follow-up care requirements. Under CBP policy, medical summary forms are completed by contracted medical personnel and should accompany individuals who had medical issues identified or addressed while in CBP custody when they leave CBP custody.
However, we found that CBP components were not consistently providing medical summary forms to individuals leaving its custody. For example, in March 2025, a senior OCMO official stated that OCMO had conducted an internal review of CBP’s electronic medical records system data and found that CBP does not routinely provide medical summary forms to individuals who are being released or transferred to an agency other than ICE. CBP did not take further action based on this review and deferred to the components to provide the forms. During our site visits, CBP officials and contracted medical personnel from three CBP facilities also stated that individuals sometimes leave CBP custody before receiving a medical summary form, which would include records of their prescription medications. We also spoke with four nongovernmental organizations that provided services to individuals released from CBP custody along the southwest border in 2024. All four organizations stated they provided services for individuals who did not have any kind of medical records detailing the medical care they received while in CBP custody.
Border Patrol headquarters officials confirmed that individuals in custody who saw medical personnel should have their medical summary forms when they leave CBP custody. However, Border Patrol officials stated that recent changes in CBP’s processing of individuals have made it harder to consistently provide these forms. For example, some individuals who have left CBP custody may return to CBP facilities from the custody of other agencies to be transported to their removal flights. In these instances, Border Patrol officials noted they do not confirm that the individuals have a medical summary form when they leave CBP’s custody for a second time, even though CBP requires it.
A January 2025 OCMO memorandum on medical summary documentation stated that the medical summary form should be considered “the most important part of the medical documentation” to ensure continuity of care and identify medical risks for transporting individuals.[46] Without a medical summary form, individuals may not have the information they need to resume medical treatment or treat issues that were identified in CBP custody upon transfer to another agency, release, or repatriation. Developing a mechanism to ensure that individuals who had medical issues identified or addressed receive their medical summary forms any time they leave CBP custody would also help CBP ensure that other agencies who transport or assume custody of these individuals are aware of their medical needs.
CBP Did Not Consistently Manage or Oversee Its Medical Services Contracts
As previously mentioned, CBP used contracted medical personnel in 44 CBP facilities along the southwest border as of May 2025 (at its peak, CBP used them in 79 facilities as of July 2024), but we identified gaps in how CBP managed its 2020 and two bridge medical services contracts. For example, CBP did not establish clear criteria for sufficient staffing levels in its 2023 Bridge II contract. Additionally, CBP has not analyzed the costs and benefits of its decisions to limit the types of care contracted medical personnel can provide to identify opportunities for potential cost savings. Further, CBP has made missteps in its management of contract costs, option amounts, and contract periods in its three contracts. In addition, CBP has gaps in its oversight of contractor performance. For instance, the agency has not developed a plan for administering the contract and monitoring the medical services contractor’s performance, has not ensured that staff designated as task order monitors for the contract have the appropriate certifications for their role, and has not annually submitted all its contractor past performance evaluations as required. Finally, while CBP met many of the requirements it set for itself in overseeing the quality of care that contracted medical personnel provide, OCMO’s Medical Quality Division did not document some of those activities as required.
CBP Had Gaps in Its Management of Its Bridge II Medical Services Contract
CBP Did Not Specify Clear Criteria for Sufficient Staffing Levels in the CBP Medical Services Contract
CBP’s Bridge II medical services contract, awarded in November 2023 with a period of performance through August 27, 2025, provided the contractor with flexibility in the biweekly schedule that it submits to CBP.[47] For example, it stated that the contractor shall provide CBP with a biweekly schedule of contracted medical personnel (providers and staff) and the contractor is expected to adhere to a 95 percent performance target of its biweekly staffing schedule, subject to exceptions. However, the contract did not specify minimum acceptable staffing levels that the contractor is required to meet for medical personnel at CBP facilities.
In addition, CBP did not establish contractually required performance targets for assessing staffing levels. For example, CBP’s Bridge II contract initially stated that the contractor was expected to maintain the 95-percent adherence to the contractor’s biweekly staffing schedule. Subsequently, in August 2025, CBP removed the percentage adherence expectation language from its updated statement of work.
The DHS Acquisition Manual, which provides the department’s acquisition procedures, stresses the importance of defining requirements (what goods or services the agency needs) in acquisition planning.[48] According to the manual, the program office shall support the contracting officer in ensuring that requirements are clearly defined and specified. In addition, the DHS Desk Guide for Developing and Managing Contract Requirements states that requirements should be defined in terms of minimum needs and there should be a way to measure the progress during performance and at completion.[49]
Our review of CBP’s Bridge II medical services contract found that the contract did not include criteria for what CBP should use to determine sufficient staffing levels, nor did CBP require the contractor to meet a performance target percentage for staffing levels that was outlined in the Bridge II contract. For example, the Bridge II contract’s statement of work required the contractor to submit a biweekly staffing schedule to CBP, but it did not specify a minimum number of staff that the contractor must provide.[50] According to the contracting officer for the medical services contract, the contract was intentionally structured to provide the contractor with the flexibility to respond to changing operational demands. While we acknowledge that flexibility is appropriate in this case, CBP should specify minimum staffing levels to the contractor to ensure that CBP is getting the staffing level that it needs.
|
Staffing Level List (i.e., Medical Laydown) The Office of the Chief Medical Officer (OCMO) Border Health System Division’s staffing level list consists of the facilities that the Division designated as priorities and the contracted medical personnel staffing levels each facility needs. According to OCMO, this list is based on the number of medical interactions at each facility and how remote the area around the facility is, among other factors. Source: GAO analysis of U.S. Customs and Border Protection information. | GAO‑26‑107425 |
CBP included a staffing level list (also referred to as the medical laydown) as an appendix to the two bridge contracts (see sidebar for information included in the staffing level list). The list included names of CBP facilities, their daily hours of operation, and the number of contracted medical personnel needed at each facility per shift. However, CBP did not clearly state in the contract what the purpose of the staffing level appendix was, nor were officials able to explain to us how, if at all, the staffing level appendix relates to staffing requirements for the contractor or to the contractor’s biweekly staffing schedule. As a result, it was unclear to what extent, if at all, the staffing level list was used as an expectation of staffing requirements in the contractor’s biweekly schedules.
OCMO used the staffing level list as a baseline to monitor the number of contracted medical personnel at each CBP facility in real time, as reflected in its electronic medical records system. However, according to OCMO, the contractor has not always achieved the levels of staffing identified in the list. In addition, as we previously stated, DHS’s Office of the Immigration Detention Ombudsman cited staffing shortages of medical personnel at certain CBP facilities using the staffing level list as a baseline and made a related recommendation that CBP concurred with.[51]
OCMO used the staffing level list as a baseline, according to OCMO and Office of Acquisition officials. However, CBP’s official position was that the contractor was required to provide CBP a biweekly schedule and was expected to meet 95 percent of that schedule as a performance target but is not contractually required to do so. The contracting officer explained that in this biweekly schedule, the contractor listed the number of contracted medical personnel scheduled to work at each CBP facility for the next two weeks. However, the Bridge II medical services contract did not require the contractor to use the staffing level list as a baseline for its biweekly staffing schedule.
In August 2025, CBP incorporated updates to its statement of work during an extension to the Bridge II contract. The updated statement of work included additional information on the staffing level appendix. It stated that the staffing list in the appendix represents the initial baseline of medical staffing support, and that the list will be updated monthly or as needed given operational changes. This is a good initial step, but the statement of work is still not clear about whether the contractor is required to provide support at the levels identified in the staffing level list appendix. Furthermore, the updated statement of work did not include language specifying a minimum staffing level for the biweekly schedule and removed any language about CBP expecting the contractor to adhere to 95 percent of the contractor’s biweekly staffing schedule. Moreover, since CBP incorporated the statement of work toward the end of the Bridge II contract, it is too soon to determine the impact of the potential changes.[52]
Staffing is one key element of the contract and having the contracted medical personnel that CBP needs in facilities helps ensure that individuals in custody receive medical care as specified in CBP guidance. While CBP has taken steps to clarify the purpose of the staffing level list, CBP needs to make clear in any future medical services contracts what staffing levels the contractor is required to provide and how CBP will measure contractor compliance with the staffing levels. Without clearly specifying minimum needs in any future medical services contracts for what the biweekly schedule should include, CBP cannot ensure that the contractor is providing sufficient staff to meet its needs for providing medical care at its facilities. Furthermore, without requiring the contractor to meet a performance target percentage for its staffing levels, CBP is not positioned to consistently hold the contractor accountable to meeting staffing level requirements.
CBP Has Not Analyzed the Costs and Benefits of its Decisions to Limit the Types of Care Contracted Medical Personnel Can Provide and to Reduce Staffing Levels
CBP has specified the types of medical care the contractor is expected to provide for individuals in custody at CBP facilities. This includes types of care that contracted medical personnel cannot provide under the contract, necessitating they refer individuals to local health providers. However, CBP has not analyzed the costs and benefits of its decisions to limit the types of care contracted medical personnel can provide and to reduce the staffing levels of contracted medical personnel. Centers for Disease Control and Prevention guidance for public health decision-making includes analyzing the costs and consequences of different public health interventions.[53] For example, a cost-effectiveness analysis can be used to compare the cost of a program to its health outcomes, such as illnesses and deaths averted. Similarly, a cost-benefit analysis can be used to compare monetary costs of a program to its expected monetary benefits, such as the cost of implementing the program to savings expected to accrue from the program.
However, CBP has placed limitations on the types of care contracted medical personnel can provide, even if personnel are qualified to provide that care, and has not based these limitations on a cost-benefit analysis. More specifically, CBP has specified that contracted medical personnel must refer certain types of care to local health systems, such as hospitals or urgent care centers. These types of care include complex, urgent, or emergent medical conditions. However, for other types of care that contracted medical personnel are licensed to provide onsite at CBP facilities, CBP has not conducted a cost-benefit analysis to assess its decisions regarding the types of care contracted medical personnel can provide. For example:
· COVID-19 tests. Contracted medical personnel do not administer COVID-19 tests in CBP facilities. According to contracted medical personnel, if a contracted medical provider believes that an individual in custody should be tested for COVID-19, they must send that person to a local hospital for testing. In contrast, some contracted medical personnel said they do administer tests for influenza at CBP facilities.
· Intravenous lines. Contracted medical personnel do not administer intravenous lines. For example, at one facility we visited, a contracted medical provider described a recent situation in which an individual in custody needed IV fluids for heat exhaustion. Although the contracted medical provider is a registered nurse and is certified to administer IVs, the individual in custody had to wait 20 minutes for an ambulance before receiving IV treatment.
· Oxygen. Contracted medical personnel do not administer oxygen to individuals in custody even though they are trained and licensed to perform those services. However, an OCMO official told us OCMO is planning to equip facilities with oxygen administration capabilities before the end of fiscal year 2025. CBP officials stated they plan to have contracted medical personnel administer medical grade oxygen to patients with dangerously low blood oxygen levels because it is a potentially life-saving intervention, which is consistent with CBP’s goal of providing basic lifesaving medical interventions to individuals in custody. Additionally, they noted the American Academy of Pediatrics has indicated oxygen and oxygen delivery systems are essential for all sites delivering medical care to children.
A CBP official said OCMO developed the contracted medical personnel’s scope of practice in 2015 to reflect CBP’s goal of providing rudimentary medical screening and basic medical resources at a small number of facilities. Since then, the official said, OCMO has not expanded the scope of practice because doing so would add medical equipment and other costs. The official noted that staffing shortages of contracted medical personnel also make it difficult to add to their scope of practice, and individuals requiring emergency or in-depth medical care would still need to go to the hospital.
Further, in February 2025, OCMO officials stated that CBP has reduced staffing levels for the medical services contract to improve cost efficiency and respond to the decreased number of individuals in custody across the southwest border. Since CBP reduced the number of facilities along the southwest border with contractor medical personnel—from 79 facilities in 2024 to 44 in 2025—CBP officials stated they have seen a higher number of hospital referrals.[54] For example, at facilities without contracted medical personnel, CBP officers and agents are to take consenting pregnant individuals and all children in custody to the hospital for required medical assessments, even if they are healthy.[55] At facilities with contracted medical support staff but no medical provider, any individuals who need to take medication may also be referred to the hospital given limitations on the contracted medical support staffs’ ability to administer medication.
However, CBP has not assessed whether these decisions to limit contracted medical personnel’s scope of practice and reduce contracted staffing levels are cost effective when compared with the costs of hospital referrals. For example, OCMO has not compared the cost of providing COVID tests in CBP facilities, which contracted medical personnel are licensed to provide, with the cost of sending individuals to the hospital for COVID testing.
Sending individuals to the hospital creates both direct and indirect costs for the government. CBP has historically charged offsite medical care costs to U.S. Immigration and Customs Enforcement’s (ICE) annual operations and support appropriation by submitting claims from offsite medical providers through ICE’s Medical Payment Authorization Request system. In fiscal year 2023, ICE obligated about $76 million for medical costs related to individuals in CBP custody. Hospital referrals also require CBP facilities to redirect agent or officer resources away from the facilities and enforcement activities to transport and supervise individuals while they are in the hospital. Furthermore, a 2024 analysis by the DHS Science and Technology Directorate found that having a medical services contract saved CBP approximately $75 million in fiscal year 2022, compared with the costs of providing medical care through local hospitals. The savings stemmed from reducing hospital and transportation costs and reducing the number of hours agents and officers spent supervising individuals in the hospital.
Hospital referrals are necessary and critically important in emergency situations. However, decreasing staffing levels for the medical services contract and reducing the number of personnel to a single support staff at some facilities could lead to individuals being sent to the hospital for non-emergency care. While reducing the number of contracted medical personnel at CBP facilities may reduce contract costs, sending individuals to the hospital for services that are within contracted medical personnel’s scope of practice has the potential to increase costs to the government. Without comparing the costs of providing non-emergency care through contracted medical personnel to the costs of providing that care at the hospital or other local health system facility and documenting any resulting savings, CBP could miss opportunities to be efficient and maximize the value of contracted medical personnel.
CBP’s Office of Acquisition Made Missteps in Administering Its Medical Services Contracts
We found several missteps in CBP’s administration of the three medical services contracts at the time of our review. A May 2021 CBP acquisition alert recommends that CBP officials identify previous issues and problems as it prepares for contract administration for all CBP awards over the simplified acquisition threshold ($250,000, with some exceptions during our review).[56] In addition, we and others have identified the importance of program and project management to identify and apply lessons learned from projects to limit the chance of recurrence of previous failures or difficulties.[57] And, according to federal internal control standards, management should identify, analyze, and respond to risks related to achieving its defined objectives, as well as apply corrective actions to remediate internal control deficiencies on a timely basis.[58]
|
Medical Services Contract-Related Terms The medical services contract is a hybrid contract with both time-and-materials and firm-fixed-price elements. Time-and-materials: payments to contractors are based on the number of labor hours billed at a fixed hourly rate—which includes wages, overhead, general and administrative expenses, and profit—and the cost of materials, if applicable. For the medical services contract, this includes its medical professional providers and support staff. Firm-fixed-price: a price that is not subject to any adjustment based on the contractor’s cost experience in performing the contract. For the medical services contract, this includes backend administrative staff, project managers, security, recruiters, and other corporate human resource personnel. Cost ceiling: the contractor’s “not to exceed” amount in the contract. The government does not have to pay the contractor beyond the ceiling but can adjust the ceiling with written notice. Obligation amount: the amount that the government is legally committed to paying for goods or services it ordered or received. Contract option: if a contract includes options, the government may choose to purchase additional supplies or services or extend the terms of the contract but does not have to if it is not in its best interest. If the government chooses to use the option, it is called exercising the option. FAR 2.101. Source: GAO analysis of the Federal Acquisition Regulation (FAR) and acquisition documents. | GAO-26-107425 |
We reviewed CBP’s three medical services contracts that were in effect from fiscal years 2021 through 2025 and identified missteps CBP made in how it administered the contracts. We also found that CBP did not identify lessons learned or risk areas to apply corrective actions to improve how it administers its medical services contracts. For example:
· CBP did not consistently define the contract cost ceiling. CBP did not consistently define the dollar amount that the contractor should not exceed in the contract modifications of its two 2023 bridge medical services contracts. For instance, CBP officials used the contract value amount or the obligation amount, which were different dollar values, as the “not to exceed” ceiling at various points during the administration of the Bridge I and Bridge II contracts. This inconsistent tracking of the “not to exceed” amount can cause confusion about when the contractor starts to work over the “not to exceed” amount, at its own risk. See the sidebar for more information on the cost ceiling.
· CBP exceeded the contract cost ceiling and paid contractor invoices late. The costs CBP incurred exceeded the cost ceiling in the time-and-materials portion of the 2020 medical services contract without prior approval of the contracting officer. CBP attributed this to paying the medical services contractor $13 million for invoices that CBP processed late. As a result, CBP had to increase obligations to pay the contractor.[59] The Federal Acquisition Regulation (FAR) allows the government to pay for hours that the contractor worked above the ceiling with written notice from the government. CBP provided this notice to the contractor, but only after the contract period of performance had ended.[60]
· CBP inconsistently exercised option amounts and periods. CBP exercised contract options (options to extend medical services) for different dollar amounts than what the contract specified and at times for different (partial) time periods than what the contract specified. Specifically, CBP exercised options at a different amount than the option price in 19 of the 23 options exercised on the 2020 and 2023 Bridge II contracts. For example, CBP exercised one option period in the Bridge II contract for about $19 million when it should have been for about $25 million. In addition, CBP partially exercised four contract options in the two contracts. For example, although CBP set each option period in its contracts for about 30 days, CBP exercised a 30-day option for 14 days instead in the 2020 medical services contract. Doing so was inconsistent with CBP’s documented determination of how it would exercise the option periods.[61]
CBP’s Office of Acquisition officials identified various reasons for the missteps in its administration of the medical services contracts. For example, officials attributed the late invoices in part to the contractor’s invoicing system. The officials explained that until January 2023, the contractor used a manual invoicing process, and it could take the contractor more than 120 days to submit invoices to CBP. CBP’s acquisition officials stated they only became aware of the late invoices when OCMO discovered a large amount of unliquidated funding. In addition, CBP’s Office of Finance raised concerns about the timely use and accountability of funds for the 2020 medical services contract. Additionally, CBP’s acquisition officials were unaware that they had exercised some options at different dollar amounts and partially exercised some options until we pointed it out to them.
CBP’s Office of Acquisition officials said that they hold weekly meetings with OCMO’s Border Health System and Acquisition Management Divisions to discuss lessons learned on contracting strategies for acquiring medical services, among other issues. However, the Office of Acquisition has not conducted any lessons learned analyses on how it managed and administered the medical services contracts, including identifying and implementing corrective actions.
While these missteps individually may not be major issues, they collectively raise concerns about the quality of contract administration for a contract that CBP considers high-risk. In addition, CBP plans to continue contracting for medical services for the foreseeable future. Therefore, reviewing the medical services contracts for any errors and lessons learned would better position CBP to identify and analyze risk areas and apply corrective actions to help ensure that CBP minimizes administrative errors and missteps in future such contracts. CBP officials told us CBP is in the beginning stages of creating an acquisition program for its electronic medical records system and is planning to move medical service, which includes the medical services contract, as a sub-program under it. As it assesses the needs and develops requirements for that program, CBP could analyze lessons learned from administering its prior and current medical services contracts. This analysis would help CBP officials understand the root cause of the missteps and ensure it takes the appropriate corrective actions for the administration of any future medical services contracts, should CBP continue to contract for this service.
CBP Has Gaps in Its Oversight of Contractor Performance for Medical Services
CBP Did Not Develop a Contract Administration Plan for Its Bridge II Medical Services Contract
CBP managed its Bridge II medical services contract through weekly meetings with the CBP offices with oversight responsibilities for medical services.[62] CBP officials stated that during these meetings, they discussed challenges, initiatives to improve how contracted medical personnel provide medical care, and any changes CBP needed to make to the contract’s statement of work. However, CBP did not develop a contract administration plan for its medical services contracts.
The DHS COR Guidebook and a May 2021 CBP acquisition alert recommend that CBP develop a contract administration plan in advance of the contract award for effective oversight of all contracts exceeding the simplified acquisition threshold.[63] According to the guidebook, a contract administration plan documents the approach for monitoring and managing a contract award at a level of detail appropriate to the complexity of the acquisition. It describes activities necessary to monitor the contractor’s performance to ensure that the government receives the required products or services in a timely and cost-effective manner. The plan also specifies who is responsible for overseeing the contractor’s work, the process for documenting acceptance or rejection of work products, and the level and types of surveillance to be used to monitor performance, including what metrics CBP will use to measure performance.
CBP did not have a contract administration plan or an equivalent document detailing how CBP personnel should conduct oversight of the Bridge II medical services contract (which was above the simplified acquisition threshold). The total value of the Bridge II contract was about $311 million including the base period of performance and all option periods at the time of award.[64] In addition, according to OCMO’s Acquisition Management Division and CBP’s Office of Acquisition, the medical services contract is considered high-risk given its dollar value and complexity. According to Office of Acquisition officials, they did not prepare a contract administration plan because it was not required and other documents, such as the contract’s statement of work, included information that would be in a contract administration plan. Instead, they reviewed and discussed the terms, conditions, and award clauses with CBP officials from the program and contracting offices, as well as with the medical services contractor.
However, we identified gaps in CBP’s contractor oversight for the Bridge II contract. For example, CBP did not clearly identify the level and type of oversight to be used to monitor contractor performance in its medical services contract. Office of Acquisition officials stated that the COR appointment letters contained this type of information.[65] While the COR appointment letters for the medical services contract listed the scope of responsibilities for CORs, they did not include the level of detail that a contract administration plan would include, such as specific information on what method would be used to monitor contractor performance and the frequency of site visits. Although the CORs were responsible for performing oversight activities and providing input to contractor performance evaluations, the primary COR for the Bridge II contract told us that they did not directly observe performance under the medical services contract until 2024, after an internal reorganization. In addition, according to a senior official from OCMO’s Acquisition Management Division, most local on-site task order monitors, whose role is to assist CORs in contractor oversight, did not provide sufficient contractor oversight, including reporting contractor performance to the CORs.
Furthermore, CBP did not include ways to measure the adequacy of contractor performance in its Bridge II contract, which would be part of a contract administration plan. Office of Acquisition officials stated that they currently measure contractor performance based on a list of deliverables that the contractor is required to submit to CBP. These deliverables were included as an appendix to the medical services contract. They included credentialing files for contracted medical personnel and staffing reports.[66] We found that the only measure of contractor performance for each deliverable in the Bridge II contract was the due date. For example, the Bridge II contract’s statement of work required the medical services contractor to submit risk management and quality assurance reports and stated that OCMO shall determine the format and elements of the report, but the statement of work did not include details on what information CBP required from the contractor and how it would measure the adequacy of its content in meeting CBP’s requirements. With a contract administration plan, according to DHS and CBP guidance, CBP would address all post-award activities necessary to monitor the contractor’s performance, including indicators of satisfactory performance.
During our review, CBP began developing some elements of a contract administration plan for the Bridge II contract. For example, a senior official from OCMO’s Acquisition Management Division stated that during the CORs first site visit in 2024, they identified and documented medical risk areas, such as medication management and the contractor’s access to the electronic medical records system. However, the senior official also stated that they did not assess performance since the contract lacks outcome-based performance metrics. In addition, as previously mentioned, the OCMO’s Border Health System Division is developing a compliance program using data to improve its tracking and monitoring of the medical care that contracted medical personnel provide.
While the CORs conducting site visits and identifying medical risk areas are good steps toward better contract administration, a more detailed contract administration plan would help CBP provide consistent contractor oversight for future medical services contracts, should CBP continue to contract for this service. According to the DHS COR Guidebook and CBP’s May 2021 acquisition alert, a detailed plan addresses all post-award activities necessary to monitor the contractor’s performance by clearly and specifically laying out in a single document the oversight responsibilities of all relevant entities, how the entities should conduct oversight, and the specific performance indicators to evaluate contractor performance.
Our prior work identified similar challenges with contract administration plans at CBP. Specifically, we found that CBP did not have such plans for any of its eight contracts for temporary soft-sided facilities—steel-framed tent-like structures—that we reviewed.[67] We also identified instances where the CORs did not have the information they needed to provide contractor oversight. We recommended that CBP take action to ensure that contract oversight officials prepare and implement contract administration plans in accordance with DHS and CBP guidance. CBP concurred with the recommendation and stated that it will update its guidance to require contracts with certain high-dollar thresholds to use a contract administration plan and provide targeted training to individuals responsible for contract administration and oversight. In addition, at the end of July 2025, after discussions with us about the issues we identified, OCMO stated that CBP will update its guidance to require that contract oversight personnel develop and document a tailored contract administration plan for high-risk contracts. OCMO also stated that CBP will use such plans to proactively monitor them, clarify roles and responsibilities, and enhance accountability. While this is positive, OCMO did not provide us with documentation of any plans or efforts underway to develop such a plan for any future medical services contracts.
As CBP updates its guidance regarding contract administration plans, it should ensure that it develops one for any future medical services contracts. Without a detailed contract administration plan that identifies roles and responsibilities and includes performance metrics specifically for the medical services contract, CBP is missing opportunities to provide consistent and measurable contractor oversight and to obtain a more complete and quantifiable understanding of contractor performance.
CBP Did Not Certify or Appoint Task Order Monitors for the Bridge II Medical Services Contract
CBP designated task order monitors for its Bridge II medical services contract but did not certify or appoint them consistent with DHS guidance. DHS’s COR Guidebook provides guidance for task order monitors (referred to as technical monitors in the guidance), including required qualifications, training, and communication with the COR about technical direction. It requires technical monitors to be certified at the same level as the COR and receive an appointment from the contracting officer.[68] In addition, DHS Acquisition Workforce policy requires CORs for high-risk or major investments, such as the medical services contracts, to be certified at the highest level.[69] According to the Office of Acquisition and OCMO’s Acquisition Management Division, the Bridge II medical services contract is considered high-risk given its dollar value and complexity. This requirement helps ensure that the CORs have the knowledge and experience needed to oversee more complex contracts. Table 4 outlines the certification requirement levels for DHS CORs and task order monitors, who are required to be certified at the same level as a COR, according to the DHS COR Guidebook (which refers to task order monitors as technical monitors).
Table 4: Department of Homeland Security (DHS) Contracting Officer’s Representatives’ (COR) Federal Acquisition Certification Levels
|
Level |
COR Certified Level II |
COR Certified Level III |
|
Initial training requirementsa |
40 hours |
60 hours |
|
Biennial continuous learning requirementsb |
40 hours |
40 hours |
|
Prior COR experience |
1 year |
2 years on contracts of moderate-to-high complexity |
|
Contract complexity |
Moderate-to-high complexity, including both supply and service contracts |
High-risk or major investments, such as time-and-materials or hybrid contracts; and complex and mission critical contracts |
Source: GAO analysis of DHS and the Office of Management and Budget COR guidance documents | GAO‑26‑107425
Note: DHS requires either a Level II or a Level III COR certification due to the complexity of DHS’s contracting portfolio.
aThis includes courses on COR roles and responsibilities and fundamental contract regulations.
bAs part of the initial training and continuous learning requirements, CORs must also complete courses on ethics and procurement integrity and human trafficking.
CBP relies on Border Patrol agents and OFO officers who, according to CBP officials, have not had COR-certified training or received appointments from the contracting officer to serve as task order monitors for the Bridge II medical services contract. Moreover, according to the DHS COR Guidebook, task order monitors (referred to as technical monitors in the COR Guidebook) are also required to have relevant experience appropriate for the specific duties delegated by the contracting officer.
However, without an appointment letter, we found that CBP used local task order monitors informally and that local task order monitors did not have specific duties delegated by the contracting officer. As a result, the types of oversight these task order monitors provided and their interactions with the contractor varied. For example, one task order monitor in California stated that they provided oversight of medical services personnel, including ensuring that contracted medical personnel had their badges and wore appropriate clothing. In contrast, a task order monitor in Arizona told us they primarily handled facility-related issues by e-mail or phone and checked that the number of hours that contracted medical personnel billed matched the number of hours recorded in the contractor’s sign-in sheet. The Arizona task order monitor stated that they generally did not go into the facilities where the contracted medical personnel were working, whereas the California task order monitor spent time in the facility. In addition, the California task order monitor stated that monitors were not COR-certified and did not receive structured guidance on how to provide contractor oversight.
According to a senior official from OCMO’s Acquisition Management Division, many local task order monitors for the medical services contract are currently not certified at the same level as CORs, as DHS COR guidance requires. In addition, the contracting officer for the Bridge II medical services contract stated that CBP has not formally appointed the task order monitors through an appointment letter. Furthermore, at the time of our review, a senior official from OCMO’s Acquisition Management Division was not aware of the requirement for local task order monitors to be certified at the same level as the primary COR, which is level III for the medical services contract (see Table 4 above). Acquisition Management officials also stated they are hiring dedicated (full-time) task order monitors to act as local CORs for any future medical services contracts. Initially, officials stated that they planned to certify these dedicated task order monitors as CORs, but at a lower certification level than the primary COR for the medical services contract. This approach is not consistent with direction in the DHS COR guidebook. As previously mentioned, high-risk or major investments like the medical services contracts are required to have the CORs (or the equivalent task order monitors) certified at the highest level. In addition, CBP officials told us that the contracting officer will appoint these dedicated task order monitors. In July 2025, after discussions with us about the issues we identified, OCMO stated that it plans to train and certify the dedicated task order monitors at the appropriate level.[70] CBP did not provide documentation of these plans.
By implementing these plans, however, CBP will be better positioned to ensure it has qualified personnel performing contract oversight on a high-risk contract and representing the government as they interact with the contractor. Training and certifying task order monitors at the same level as the primary COR helps to ensure that they are capable of providing oversight consistent with COR-delegated responsibilities and contract terms. Being appointed by the contracting officer, who is ultimately responsible for contract management, helps ensure that the contracting officer is informed about the person performing oversight duties and that only authorized individuals are performing contract oversight on their behalf. In addition, the appointment letter provides notice to the contractor of the individuals authorized to act as task order monitors and represent the government in their oversight functions.
CBP Did Not Always Submit Its Annual Contractor Past Performance Evaluations
CBP did not always complete its contractor past performance evaluations for the three medical services contracts in effect from fiscal years 2021 through 2025. The FAR states that past performance evaluations shall be prepared at least annually and at the time the work under a contract or order is completed.[71] The FAR requirement also includes evaluations for orders placed under a federal supply schedule contract or a task-order contract awarded by another agency, as was the case for CBP’s medical services contracts.[72] Additionally, Contractor Performance Assessment Reporting System guidance, which is applicable to all federal agencies, states that agencies should complete past performance ratings within 120 days following the end of the period of performance.[73]
CBP did not submit a required past performance evaluation for its 2020 medical services contract. Additionally, CBP did not submit all its required past performance evaluations for the 2020 and Bridge II medical services contracts in a timely manner. Specifically:
· CBP did not submit one of the required evaluations for the 2020 medical services contract. Instead, CBP submitted an evaluation that covered the 18-month period of performance from September 30, 2021, through March 29, 2023. Doing so was inconsistent with the FAR, which requires two evaluation submissions, one annual evaluation and one evaluation at the end of the period of performance. When asked for an explanation, a COR stated that CBP forgot to submit an annual evaluation because someone incorrectly marked a prior evaluation as final instead of annual, so the office did not receive an automatic alert for the next evaluation.
· CBP submitted the other required past performance evaluation for the 2020 medical services contract, but it was late. CBP completed an annual evaluation for the 2020 medical services contract 10 months after the first year of performance (instead of within the 120-day time frame specified in guidance). According to Office of Acquisition officials, this delay occurred because the COR who had been responsible for evaluating and documenting contractor performance left the position. As a result, the new COR needed time to gather contractor performance information.
· In addition, as of August 2025, approximately 9 months after the end of the first year of performance for the Bridge II contract (awarded in November 2023), CBP had not submitted its annual contractor past performance evaluation. According to officials from the Office of Acquisition, CBP is again planning to submit one evaluation to cover the entire Bridge II contract period of performance instead of the two required evaluations (one annual and one at the end of the period of performance). The end of the Bridge II contract period of performance was originally planned for November 29, 2024. CBP initially extended the Bridge II contract by 6 months to May 29, 2025, then extended it again for 3 months, through August 27, 2025. As a result, the past performance evaluation will now cover a 21-month period of performance from November 30, 2023, through August 27, 2025.[74] This approach is inconsistent with the FAR.
Figure 12 provides more information on CBP’s submission of contractor past performance evaluations as of August 2025.
Figure 12: U.S. Customs and Border Protection’s (CBP) Contractor Past Performance Evaluations for the Medical Services Contracts as of August 2025
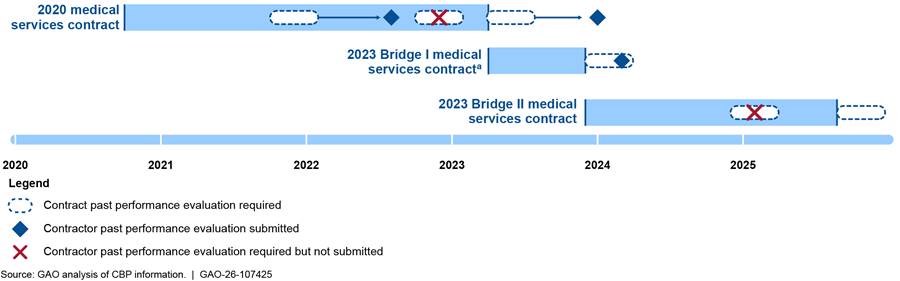
Note: On May 30, 2025, CBP added three additional option periods to the 2023 Bridge II contract to extend the period of performance by 90 days through August 27, 2025. In addition, CBP extended the Bridge II contract again through September 27, 2025, and awarded the Bridge III medical services contract on September 28, 2025, after we provided DHS with our report for review and comment. Thus, we did not include the Bridge III contract within the scope of our review.
aThis evaluation was subsequently revised in July 2025 due to a litigation settlement.
According to an official from the Office of Acquisition, the FAR and Contractor Performance Assessment Reporting System guidance supports the practice of submitting one evaluation covering the entire period of performance for contracts exceeding one year in cases where the agency extends performance for 6 months. CBP extended its 2020 medical services contract by 6 months and extended the Bridge I medical services contract by 5 months. For the Bridge II contract, CBP had extended it for about 9 months as of August 2025. However, the FAR clearly states that past performance evaluations shall be prepared at least annually and at the time the work under a contract or order is completed. In addition, Contractor Performance Assessment Reporting System guidance states that, because the FAR requires an annual past performance evaluation, annual evaluations are required at least every 12 months throughout the entire period of performance of the contract or order. As a result, CBP did not submit all the past performance evaluations required by the FAR for its medical services contracts.
Complying with the timing requirements in the FAR for submitting contractor past performance evaluations for any future medical services contracts would help ensure timely completion of contractor past performance evaluations and would allow CBP to use more current information in its ratings. In addition, source selection officials would be better positioned to make informed decisions when awarding future contracts with more timely evaluations.
OCMO’s Medical Quality Division Fulfilled Many Program Requirements, but Did Not Document Some Required Program Elements
CBP met many of the requirements it set for itself in overseeing the extent to which medical services contractors ensure the quality of healthcare services and patient safety. However, CBP did not document some of those activities as required. The OCMO Medical Quality Division (formerly a committee within OCMO) oversees the Medical Quality Management Program. This is a joint program made up of two components—Medical Quality Management (MQM) representatives from the medical services contractor and MQM representatives from OCMO. Together, both components of the MQM program help ensure that the medical services contractor delivers care that promotes patient safety and meets guidelines for quality healthcare, in alignment with the contract’s requirements. The medical services contractor and MQM OCMO work together to collect and share data on five critical elements, specified in the MQM Guidance and Instruction, as shown in figure 13.[75]
Figure 13: U.S. Customs and Border Protection’s (CBP) Five Elements for Ensuring the Medical Services Contractor’s Performance is Consistent with CBP’s Medical Quality Management Requirements.
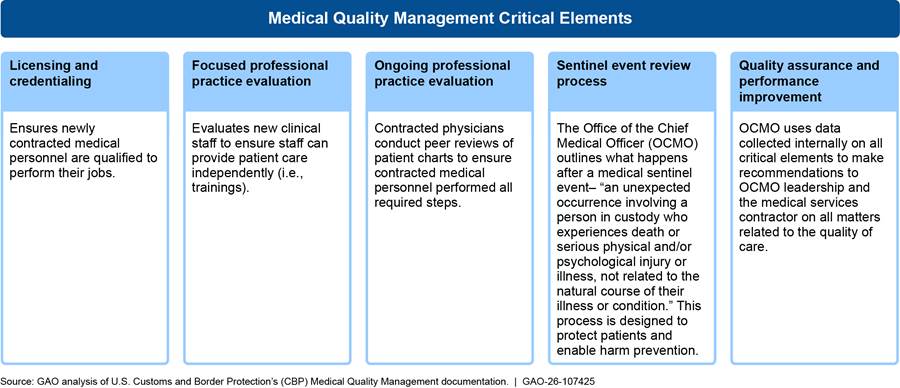
During our review of MQM documentation from fiscal years 2022 through 2025, we found that OCMO fulfilled many of the MQM program requirements.[76] For example, CBP OCMO verified that 100 percent of the contracted medical personnel included in the internal audit were appropriately qualified as part of the licensing and credentialing critical element of the MQM program. Additionally, according to MQM’s fourth quarter 2024 report, 100 percent of advanced practice practitioners completed their training and evaluation period prior to being scheduled for independent shifts.
However, CBP did not complete all the documentation required for the quality assurance and performance improvement or sentinel event review elements of the program.[77] As part of the quality assurance and performance improvement element, CBP’s MQM guidance requires MQM to create an action plan for performance improvement initiatives, measure the current process, list actionable steps, and document and measure results after implementing suggested changes. Similarly, according to CBP’s medical sentinel event review process policy, OCMO is required to use a medical sentinel event tracker to document corrective actions resulting from the sentinel event review process and track the implementation status of those corrective actions.[78] The sentinel event tracker is supposed to be updated with all relevant information after every sentinel event review is complete.
These requirements are consistent with the Joint Commission’s Comprehensive Accreditation Manual for Hospitals’ process for sentinel events.[79] The Joint Commission is a nonprofit organization that accredited and certified 23,000 healthcare organizations and programs in the United States. The manual requires healthcare facilities to create corrective action plans after sentinel events. Corrective action plans are to include, (1) who is responsible for implementation; (2) when the action will be implemented (including any pilot testing); (3) how the effectiveness of the actions will be evaluated; (4) how the actions will be sustained; (5) the point at which alternative actions will be considered if improvement targets are not met; and (6) an alternative corrective action.[80]
Our review of OCMO’s MQM documentation from fiscal years 2022 through 2025 found that it did not consistently include elements required by CBP guidance. For example, OCMO’s documentation of quality assurance and performance improvement initiatives included a brief summary of implemented changes, such as a hospital referral document that the Division developed in 2023. However, it did not include other aspects required in the guidance, such as an action plan for the quality assurance related corrective actions, documented results, or measurements of the effectiveness of the corrective actions.
Similarly, with respect to sentinel event review, MQM documented a list of sentinel events and some corresponding corrective actions. However, the list does not include all of the elements required by CBP guidance and the Joint Commission’s Comprehensive Accreditation Manual for Hospitals, such as the expected implementation date, implementation status, or who was responsible for implementation. For example, the sentinel list includes sentinel events involving self-harm and suicide attempts from 2023 and lists some corrective actions related to those events. However, the list does not document whether the corrective actions were approved or implemented, or who is responsible for implementing them.
OCMO officials attributed these gaps in documentation to unclear, outdated guidance. Specifically, OCMO MQM officials stated that CBP’s MQM guidance does not have well-defined roles and responsibilities and does not specify whether OCMO or the medical services contractor should be responsible for specific MQM requirements. For example, while the guidance requires MQM to continuously analyze data on the medical services contractor’s performance to make data-driven improvements, it does not state whether these actions should be taken by the contractor or by OCMO. OCMO also stated that the Medical Quality Division is small, and staff are generally informed about decisions and changes without the required formal documentation.
OCMO has taken several positive steps to implement MQM program requirements. However, updating existing guidance to clearly define who is responsible for documenting corrective actions as part of the quality assurance and sentinel event review processes would provide OCMO greater assurance that its efforts are improving the safety and quality of medical services provided to individuals in CBP custody. Such guidance should include requirements for documenting detailed plans for proposed corrective actions, their implementation status, and the results of corrective actions. Documenting the effects of implementing MQM recommendations could help CBP better assess the impact of the changes and help the Medical Quality Division recommend additional improvements. Similarly, comprehensively tracking sentinel event corrective actions would further support OCMO’s efforts to ensure the safety and quality of medical services provided to individuals in CBP custody. Tracking the status of sentinel event corrective actions may also help ensure the same types of events do not occur again.
Conclusions
In recent years, CBP has been responsible for providing medical services to millions of individuals in its custody in facilities along the southwest border. Individuals in CBP custody arrive with a variety of medical conditions ranging from easily treatable to life threatening injuries. At many facilities, CBP has relied on contracted medical personnel to implement its medical policies and guidance, such as by providing basic medical exams and treating acute conditions.
In assessing CBP’s implementation of its medical care policies and guidance for individuals in custody, we found that CBP and contracted medical personnel inconsistently implemented medical assessments for certain groups and monitoring requirements for individuals considered to have higher medical risk. Without an oversight mechanism to ensure individuals correctly receive required medical assessments, CBP does not have assurance that it is aware of the medical needs of the groups, such as children, pregnant individuals, and ill or injured adults, or that contracted medical personnel provided appropriate follow-up medical evaluations for known medical needs.
CBP has also not ensured that certain medically high-risk individuals in its custody are processed expeditiously or that such individuals receive enhanced medical monitoring, as outlined in custody standards and medical guidance. Until CBP clearly documents the factors personnel should consider to determine an individual is at-risk under its short-term custody standards and ensures contracted medical personnel implement its medical policies and guidance consistently, medically vulnerable people may be at higher risk of experiencing an adverse health event while detained.
Moreover, some CBP facilities do not have contracted medical personnel, requiring CBP to send individuals to local medical providers for required medical care. CBP does not monitor whether individuals in custody at these facilities received required medical assessments. Without this oversight, CBP does not have complete, quality information to monitor whether all individuals are receiving the medical care required under CBP policy. CBP is also not consistently ensuring that individuals who had medical issues identified or addressed while in CBP custody receive documentation of their medical records and medication needs when they leave the agency’s custody. Leaving CBP custody without these records, referred to as medical summary forms, makes it more challenging for individuals to resume medical treatment upon transfer to another agency, release, or repatriation. Developing and implementing a mechanism to ensure that individuals receive their medical summary forms any time they leave CBP’s custody would also help CBP ensure that other agencies who transport or assume custody of these individuals are aware of their medical needs.
In assessing how CBP managed and oversaw its three medical services contracts, we identified problems with CBP’s administration of the contracts, as well as its oversight over certain aspects of the Bridge II contract. For example, CBP did not specify minimum staffing levels that it requires the contractor to provide in its Bridge II contract, nor did CBP require the contractor to meet a performance target percentage for the contracted medical personnel staffing levels. Without specifying clear criteria for sufficient staffing levels and establishing a performance target in its future medical services contracts, CBP risks its facilities not having sufficient staff to meet its needs for providing medical services. Moreover, CBP has not analyzed the costs and benefits of the types of care that contracted medical personnel can provide versus sending individuals to local hospitals for nonemergency medical care. By not doing so, CBP could miss opportunities for efficiency and maximizing the value of contracted medical personnel.
CBP made missteps in contract management, such as exercising contract options for different dollar amounts and time periods than the contract specified. Without analyzing lessons learned and applying corrective actions, the agency could make similar errors in administering future medical services contracts. Furthermore, without a detailed contract administration plan, which clearly identifies roles and responsibilities for monitoring performance and includes performance metrics, CBP cannot provide consistent oversight of the medical services contract. Additionally, CBP used task order monitors to help oversee the medical services contract but has not ensured that they have the appropriate certifications or are appointed by the contracting officer. This risks having underqualified personnel monitoring high-risk contracts.
CBP has also completed contractor past performance evaluations but has not always submitted them consistent with the FAR and applicable guidance. Until CBP ensures evaluations of the medical service contractor’s past performance occur at least annually as well as at the end of the period of performance, the agency cannot make fully informed decisions when awarding future contracts. Finally, CBP does not have all the documentation required for actions taken in its medical quality management program. Updating existing guidance to include clear roles and responsibilities for documenting plans and tracking corrective actions would help assure OCMO that its efforts are improving the safety and quality of medical services provided to individuals in CBP custody.
Recommendations for Executive Action
We are making the following 14 recommendations to CBP:
The CBP Commissioner should ensure that the Office of the Chief Medical Officer takes action, such as providing additional training or guidance, to ensure contracted medical personnel understand the difference between medical assessments and medical encounters, and reasons for the difference. (Recommendation 1)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer develops and implements an oversight mechanism to ensure individuals receive required medical assessments. (Recommendation 2)
The CBP Commissioner should clearly document in policy or guidance the factors that CBP personnel should consider to determine an individual in custody is at-risk based on serious physical or mental injuries or illnesses for the purpose of expeditious processing under CBP’s standards for short-term custody. (Recommendation 3)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer develops and implements an oversight mechanism for CBP and contracted medical personnel to ensure medically high-risk individuals in custody receive required medical care, including medical monitoring checks and red wristbands. (Recommendation 4)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer includes information in monitoring reports on individuals at facilities without contracted medical personnel to ensure they receive the medical care required under CBP guidance. (Recommendation 5)
The CBP Commissioner should develop and implement a mechanism to ensure that individuals who had medical issues identified or addressed while in CBP custody have their medical summary forms any time they leave custody. (Recommendation 6)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer and the Office of Acquisition specify in any future medical services contracts, including bridge contracts, the minimum staffing level that CBP needs from the contractor. (Recommendation 7)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer and the Office of Acquisition establish a performance target in any future medical services contracts, including bridge contracts, to measure whether the medical services contractor is meeting minimum staffing levels. (Recommendation 8)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer performs a cost-benefit analysis of the medical services contract’s scope of practice and staffing levels to compare the costs of providing nonemergency care through contracted medical personnel at CBP facilities to the costs of providing that care at a hospital or other local health system location and documents any resulting cost savings. (Recommendation 9)
The CBP Commissioner should ensure that the Office of Acquisition conducts a lessons learned analysis on how it administered its medical services contracts, to include identifying and analyzing risk areas and applying corrective actions. (Recommendation 10)
The CBP Commissioner should ensure that the Office of Acquisition, in coordination with the Office of the Chief Medical Officer, develops a contract administration plan for any future medical services contracts, including bridge contracts, to include roles and responsibilities and performance metrics. (Recommendation 11)
The CBP Commissioner should ensure that task order monitors or their equivalents supporting any future medical services contracts, including bridge contracts, are certified at the same level as the primary contracting officer’s representatives and appointed by the contracting officer. (Recommendation 12)
The CBP Commissioner should ensure that the Office of Acquisition complies with the timing requirements to submit contractor past performance evaluations for any future medical services contracts at least annually and also at the end of the period of performance, consistent with the Federal Acquisition Regulation. (Recommendation 13)
The CBP Commissioner should ensure that the Office of the Chief Medical Officer updates existing guidance that includes clear responsibilities for the Office of the Chief Medical Officer Medical Quality Division, including responsibilities to fully document action plans and track corrective actions for the quality assurance and sentinel event review elements of the MQM program. (Recommendation 14)
Agency Comments and Our Evaluation
We provided a draft of this report to DHS for review and comment. DHS provided written comments, which are reproduced in appendix II, and technical comments, which we incorporated as appropriate. In its written comments, DHS concurred with 13 of the 14 recommendations in the report and described actions planned or underway to address them. DHS did not concur with one recommendation in the report. For five of the recommendations with which DHS concurred, DHS also requested that we close those recommendations based on actions DHS took at the conclusion of our audit. We will analyze the documentation DHS provided to assess the extent to which DHS’s actions address our recommendations.
DHS did not concur with our third recommendation to clearly document the factors that CBP personnel should consider when determining whether an individual in custody is at-risk based on serious physical or mental injuries or illnesses for the purpose of expeditious processing under CBP’s standards. After we sent the draft report to DHS, we made a slight adjustment to the recommendation, adding “or illnesses” to align with the TEDS language. DHS stated that it is not feasible to establish a comprehensive list of factors because CBP encounters individuals with a wide range of physical and mental health conditions, making these determinations complex. DHS also noted that CBP handles these determinations on a case-by-case basis, and prescribing specific factors could constrain the autonomy of field authorities and hinder operational flexibility.
Our recommendation does not specify that DHS document all the physical and mental health conditions CBP personnel may encounter among individuals in its custody. CBP policy requires expeditious processing, when operationally feasible, for individuals with serious physical or mental injuries or illnesses, and OFO officers and Border Patrol agents have been making determinations about which medically high-risk individuals to prioritize. CBP has not documented factors to guide its decisions in this area, even though, during our review, OCMO shared examples of several factors that could influence CBP’s decision to expeditiously process medically high-risk individuals, such as the severity of the medical condition, the availability of support services, and the capabilities of onsite medical care.
Documenting factors that CBP officials should consider, even if such documentation cannot account for every potential situation in a complex operating environment, would help ensure personnel are consistently implementing CBP’s expedited processing requirement. Furthermore, documenting factors would not necessarily remove field authorities’ discretion to consider the unique circumstances of each individual in custody. Rather, it would provide a framework with which CBP officials could assess these circumstances and ensure that operational expediency does not take precedence over the safety of medically high-risk individuals in CBP’s custody. We continue to believe that CBP should clearly document in policy or guidance the factors that CBP personnel should consider to determine an individual in custody is at-risk based on serious physical or mental injuries or illnesses and expeditiously process them under CBP’s standards for short-term custody. Doing so would help ensure CBP personnel are consistently implementing the agency’s expedited processing requirement when it is possible to do so.
As agreed with your offices, unless you publicly announce the contents of this report earlier, we plan no further distribution until 12 days from the report date. At that time, we will send copies to the Secretary of Homeland Security and the Commissioner of CBP. In addition, the report will be available at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions about this report, please contact us at GamblerR@gao.gov or MastersT@gao.gov. Contract points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO Staff who made key contributions to this report are listed in appendix III.

Rebecca Gambler
Director, Homeland Security and Justice

Travis Masters
Director, Contracting and National Security Acquisitions
List of Requesters
The Honorable Gary C. Peters
Ranking Member
Committee on Homeland Security and Governmental Affairs
United States Senate
The Honorable Richard J. Durbin
Ranking Member
Committee on the Judiciary
United States Senate
The Honorable Bennie G. Thompson
Ranking Member
Committee on Homeland Security
House of Representatives
The Honorable Jamie Raskin
Ranking Member
Committee on the Judiciary
House of Representatives
The Honorable Robert Garcia
Ranking Member
Committee on Oversight and Government Reform
House of Representatives
The Honorable Alexandria Ocasio-Cortez
House of Representatives
The
Honorable Teresa Leger Fernandez
House of Representatives
This report examines (1) the extent to which CBP has developed and implemented policies for providing medical care for individuals in its custody and (2) the extent to which CBP has managed its contracts for medical services and provided oversight of the contractor.
We focused our review on CBP operations along the southwest land border because it accounts for the majority of CBP encounters from fiscal years 2021 through 2024 (the most recent four fiscal years).[81] To observe CBP’s implementation of its medical care policies and CBP’s oversight of its medical services contractor, we conducted site visits at CBP facilities along the southwest border. We visited 31 facilities across Arizona, California, and Texas from June through September 2024. We selected locations among Border Patrol sectors and Office of Field Operations (OFO) field offices with the highest overall volume of encounters and the highest growth (i.e., percent change) in the volume of encounters from fiscal year 2023 to fiscal year 2024 (as of March 2024, for the comparable months). We visited facilities at five of the nine Border Patrol sectors along the southwest border—Tucson, San Diego, El Centro, Rio Grande Valley, and Laredo. We also visited facilities at three out of the four OFO field offices along the southwest border—Tucson, San Diego, and Laredo.
Across these sectors and field offices, we visited different types of facilities (e.g., permanent Border Patrol stations, soft-sided facilities, central processing centers, and OFO ports of entry); facilities with and without contracted medical personnel; and facilities in urban and rural areas. During these site visits, we interviewed Border Patrol sector or OFO field office leadership, Border Patrol agents, OFO officers, and contracted medical personnel. We also met with CBP task order monitors about their efforts to implement medical care for individuals in custody and their role in providing contractor oversight as described in CBP’s policies. We observed facility operations, including CBP’s custodial process from initial encounter to transfer or release. While these site visits, observations, and interviews are not generalizable and may not be indicative of medical care provided at all CBP facilities, they provided us with perspectives on the medical care individuals received in CBP facilities and CBP’s oversight of its medical services contractor.
In addition, to gather perspectives on CBP policies for providing medical care, its management of medical services contracts, and oversight of its medical services contractor, we conducted interviews with Department of Homeland Security (DHS), CBP headquarters, and component officials from Border Patrol, OFO, and nongovernmental organizations.[82] Specifically, we met with DHS officials from the DHS Office of the Chief Procurement Officer and Office of Health Security; CBP Office of the Chief Medical Officer, Office of Acquisition, and Office of Professional Responsibility; and Border Patrol’s Law Enforcement Operations Directorate, among others.
To assess the extent to which CBP developed and implemented its policies for providing medical care to individuals in custody, we reviewed CBP policies and guidance, such as CBP’s 2015 National Standards on Transport, Escort, Detention, and Search (TEDS).[83] We analyzed data from (1) CBP’s electronic medical records system for individuals in custody, including medical assessments, medical encounters, and hospital referrals; (2) Border Patrol’s data for the southwest border on individuals’ demographics (e.g., age), health interview responses, and time-in-custody; and (3) OFO data on individuals’ demographics, health interview responses, and time-in-custody. We analyzed various data pertaining to individuals in custody from November 2020 through August 2024.[84] For all data analyses, we only included individuals in custody with complete data and matching records. For example, we excluded records with missing data in the variables we analyzed (e.g., missing age) or records that did not match between the electronic medical records system and processing systems.
To assess the reliability of the CBP data we collected, we completed a number of steps, including (1) discussing data collection methods and internal control processes for ensuring data quality with agency officials responsible for overseeing quality control procedures for these data; (2) reviewing data for reasonableness, accuracy, and consistency, including electronic testing of the data to identify missing data and anomalies; (3) identifying any obvious errors with the data we received and attempting to rectify errors with the agency; and (4) reviewing agency policies, guidance, and practices to ensure that the data are reliable. Although some data records had missing data in certain fields or could not be matched across systems for selected analyses, we determined that the data were sufficiently reliable for the purposes of assessing the extent to which individuals received certain medical care, as well as identifying possible trends and patterns in CBP’s provision of medical care.
We analyzed these data to determine the extent to which CBP’s provision of medical care aligned with CBP’s 2019 medical directive and its 2023 medical process guidance. We also considered the extent to which CBP’s provision of medical care aligned with federal internal control standards, such as the requirement that agencies design control activities to achieve objectives.[85] For example, we analyzed the CBP data to assess whether certain groups, including tender-age children (under 13 years old), non-tender age children (13 to 17 years old), pregnant individuals, and other adults with a “yes” response to CBP’s health screening interview (i.e., sick or injured adults) received medical care as required under CBP policy and guidance. Our assessment analyzed whether these specific groups received the required medical assessments across the southwest border under CBP’s original directive from November 2020 to July 2023 and after its 2023 guidance was fully in place from August 2023 to August 2024.
We also used CBP data to determine how long medically high-risk individuals were held in CBP custody along the southwest border and compared their time in custody to medically low-risk individuals in custody from October 2023 through August 2024.[86] CBP assigns individuals a medical risk designation in the electronic medical records system based on their medical diagnoses. For this analysis, we defined medically high-risk individuals as individuals who were designated “red” medical risk, the highest level of risk, throughout their time in custody. We did not include individuals whose risk level changed during their time in custody (i.e., individuals who were initially designated red and were later downgraded to a lower risk level designated as orange, yellow, or green). We defined medically low-risk individuals as individuals who were designated “green,” the lowest level of medical risk throughout their time in custody. We compared our results to guidelines for detention time frames and processing times in CBP’s National Standards on Transport, Escort, Detention, and Search.[87]
Additionally, we analyzed the extent to which medically high-risk individuals received additional medical care, as required under CBP’s 2023 medical process guidance. More specifically, we used CBP’s electronic medical records data to determine whether medically high-risk individuals (i.e., individuals with a red medical designation) received enhanced medical monitoring checks from contracted medical personnel every four hours, as required. For this analysis, we defined medically high-risk individuals as individuals who were designated red throughout their time in custody. We calculated the time between each enhanced monitoring check for each individual. If the time between checks was 4 hours or less, we counted it as an instance of having received the required check on time. Otherwise, it was counted as an instance of not meeting the requirement. We then calculated the total number of checks performed on time out of the total number of monitoring checks. We included results for individuals in custody with complete data and matching records. For example, we excluded records of individuals with medical encounter information, including risk designation, that did not match with enhanced medical checks in the electronic medical records system.
To assess the extent to which CBP has managed its medical services contracts and provided contractor oversight, we reviewed contract file documentation for the three medical services contracts in effect from fiscal years 2021 through 2025, including the contract and modifications, statements of work, contracting officer’s representatives’ appointment letters, and acquisition plans. The contracts included the 2020 Medical Services task order contract, the 2023 Bridge I medical services task order contract, and the 2023 Bridge II medical services task order contract. We compared them with federal and DHS regulations and guidance, including the Federal Acquisition Regulation (FAR), which generally governs the federal acquisition of supplies and services. Specifically, we compared CBP’s contract management to the FAR provisions related to the contract ceiling price, exercising options, and contract data elements. We also reviewed the Homeland Security Acquisition Manual and a CBP Procurement Directorate Acquisition Alert related to contract administration.[88]
Additionally, we analyzed how CBP administered the three medical services contracts and their modifications. For the 2023 Bridge II medical services task order contract, we included the modification awarded through December 29, 2024 because that was the latest modification CBP had at the time of our analysis. In addition, we compared CBP’s contract administration with federal internal control standards related to risk management.[89] We also reviewed guidance for the acquisition workforce, such as a DHS guide on managing contract requirements and the DHS Contracting Officer’s Representative Guidebook.[90] Furthermore, we reviewed contractor past performance assessment documentation and compared that with the timing requirements in the FAR for when to submit contractor past performance evaluations, and with government-wide Contractor Performance Assessment Reporting System guidance.[91]
We reviewed agency documentation, including CBP’s staffing level lists (also referred to as medical laydowns) and staffing vacancy reports, and compared these documents with contract documentation and other relevant guidance on the provision of medical care, including the Centers for Disease Control and Prevention guidance for public health decision-making.[92] Additionally, we reviewed documentation related to CBP’s medical quality management process to oversee the quality of medical care provided by its medical services contractor. For example, we reviewed reporting to DHS and CBP management about serious, unexpected medical events (also referred to as sentinel events) and compared these efforts with CBP’s Medical Quality Management Guidance and Instruction, CBP’s Medical Sentinel Event Review Processes, and the Joint Commission’s Comprehensive Accreditation Manual for Hospitals.[93]
In addition to the interviews we listed above, we spoke with officials involved in the provision of medical care for individuals in its custody. We also spoke with CBP headquarters officials involved in administering the contract for medical services. This included the contracting officer and contracting officer’s representatives for the medical services contracts.
We conducted this performance audit from March 2024 through January 2026 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
GAO Contact
Rebecca Gambler, GamblerR@gao.gov
Travis J. Masters, MastersT@gao.gov
Staff Acknowledgements
In addition to the contacts listed above, Ashley Davis and Janet McKelvey (Assistant Directors), Kelsey Hawley (Analyst in Charge), Lena Burleson, Isamar (Izzy) Hernandez, and Jenny Shinn made key contributions to this report. Other contributors included Lori Achman, Lauri Barnes, Denise Cook, Michele Fejfar, Taylor Gauthier, Sarah Goubeaux, Eric Hauswirth, Diona Martyn, Minette Richardson, Anne Louise Taylor, and Christopher Zubowicz.
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on X,
LinkedIn, Instagram, and YouTube.
Subscribe to our Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what-gao-does/fraudnet
Automated answering system: (800) 424-5454
Media Relations
Sarah Kaczmarek, Managing Director, Media@gao.gov
Congressional Relations
A. Nicole Clowers, Managing Director, CongRel@gao.gov
General Inquiries
[1]GAO, Southwest Border: CBP Needs to Increase Oversight of Funds, Medical Care, and Reporting of Deaths, GAO‑20‑536 (Washington, D.C.: July 14, 2020).
[2]Department of Homeland Security, Office of Inspector General, Results of July 2023 Unannounced Inspections of CBP Holding Facilities in the Rio Grande Valley Area, OIG-24-20 (Mar. 15, 2024); CBP Needs to Strengthen Its Oversight and Policy to Better Care for Migrants Needing Medical Attention, OIG-21-48 (July 20, 2021); Management Alert – CBP Needs to Award A Medical Services Contract Quickly to Ensure No Gap in Services (Redacted), OIG-20-70 (Sept. 3, 2020); DHS Office of the Immigration Detention Ombudsman, Ombudsman Alert – Critical Medical Understaffing on the Border, OIDO-22-003 (July 12, 2022); DHS Office of the Immigration Detention Ombudsman, OIDO Review – CBP Medical Support Contract for Southwest Border and Tucson, OIDO-23-008 (June 16, 2023). We discuss contracted medical personnel staffing in more detail later in this report.
[3]CBP defines encounters as the sum of (1) noncitizens who are not lawfully in the U.S. whom Border Patrol apprehended; (2) noncitizens encountered at ports of entry whom OFO determined to be inadmissible; and (3) noncitizens processed for expulsions as part of CBP’s efforts to aid the Centers for Disease Control and Prevention in enforcing its authority under 42 U.S.C. § 265. See 42 U.S.C. § 268(b); 42 C.F.R. § 71.40. Title 42 expulsions began on March 21, 2020, and ended on May 11, 2023. The number of encounters could reflect unique individuals encountered more than once.
[4]U.S. Customs and Border Protection, National Standards on Transport, Escort, Detention, and Search (TEDS) (Oct. 2015).
[5]Border Patrol’s processing system for the southwest border includes data on individuals’ demographics (e.g., age), health interview responses, and time-in-custody. OFO’s processing system includes data on individuals’ demographics, health interview responses, and time-in-custody.
[6]U.S. Customs and Border Protection, Directive No. 2210-004, Enhanced Medical Support Efforts (Dec. 2019); U.S. Customs and Border Protection, Medical Process Guidance (June 2023).
[7]The FAR is currently undergoing a complete overhaul called the Revolutionary FAR Overhaul. Executive Order 14275 directs the Office of Federal Procurement Policy to reduce the FAR to what is required by statute and is necessary for streamlined and efficient federal procurement. Exec. Order No. 14275, 90 Fed. Reg. 16,447 (Apr. 15, 2025).
[8]Proclamation No. 10888, 90 Fed. Reg. 8333 (Jan. 20, 2025). As of December 2025, several organizations and individuals had challenged the Proclamation and the Government’s actions to implement and enforce it. Amended Complaint, Refugee & Immigrant Ctr. for Educ. and Legal Servs., et al. v. Noem, et al., Civ. A. No. 1:25-cv-00306 (D.D.C. Feb. 19, 2025), ECF No. 11. On July 2, the district court, among other things, enjoined DHS from implementing aspects of the Proclamation. Order, Refugee & Immigrant Ctr. for Educ. and Legal Servs., et al. v. Noem, et al., Civ. A. No. 1:25-cv-00306 (D.D.C. July 2, 2025), ECF No. 73. The Government appealed this order to the U.S. Court of Appeals for the D.C. Circuit. On August 1, 2025, the appellate court partially denied and partially granted the government’s request for a stay of the district court’s order pending appeal. At the time of reporting, this litigation was ongoing.
[9]Exec. Order No. 14165, 90 Fed. Reg. 8467 (Jan. 20, 2025).
[10]For example, CBP released detained individuals with a Notice to Appear in immigration court or granted parole for an individual to enter and stay temporarily in the U.S. under certain conditions.
[11]For the purpose of this review, we generally refer to the medical services task orders as “contracts” or “medical services contracts.” This report focuses on CBP’s medical services contracts that were in effect from fiscal years 2021 through 2025.
[12]The Department of Veterans Affairs manages a multiple award Federal Supply Schedule program, which includes nine healthcare-related schedules—groups of contracts used to order medical supplies and services—under authority delegated by the General Services Administration. A multiple award Federal Supply Schedule is an indefinite delivery/indefinite quantity contract vehicle. Agencies may place orders—called task orders—under the Federal Supply Schedule indefinite delivery/indefinite quantity contracts. For more information, see GAO, VA Acquisition Management: Steps Needed to Ensure Healthcare Federal Supply Schedules Remain Useful, GAO‑20‑132 (Washington, D.C.: Jan. 9, 2020).
[13]While there is no government-wide definition for bridge contracts, we have defined it as an extension of an existing contract beyond the period of performance (including base and option years) or an award of a short-term sole-source (noncompeted) contract to the incumbent contractor to avoid a gap in service when an existing contract is set to expire but there is a delay in awarding a follow-on contract. For purposes of this report, we will refer to these bridge task orders as “bridge contracts.” For more information, see GAO, Information Technology: Agencies Need Better Information on the Use of Noncompetitive and Bridge Contracts, GAO‑19‑63 (Washington, D.C.: Dec. 11, 2018).
[14]CBP extended the Bridge II contract again through September 27, 2025, and then awarded the Bridge III medical services contract on September 28, 2025, after we provided DHS with our draft report for review and comment. Thus, we did not include the Bridge III contract within the scope of our review.
[15]FAR 1.602-1; 1.602-2.
[16]During our review, CBP used Border Patrol agents and OFO officers as local task order monitors. These monitors were on-site at CBP facilities and typically also had other operational duties. As of March 2025, CBP had hired one dedicated task order monitor and selected six additional dedicated task order monitors, according to the Office of the Chief Medical Officer’s Acquisition Management Division. In addition, according to the Acquisition Management Division, these dedicated monitors will be responsible for several CBP facilities within a region. Local and dedicated task order monitors report to different offices. (See figure 5.)
[17]The contractor is to obtain and submit proof of a completed and thoroughly reviewed CBP background investigation and all appropriate credentials for contract medical personnel candidates to the COR before they can become contracted medical personnel for the medical services contract.
[18]According to CBP officials, if for some reason the physician does not answer, then the onsite contracted medical personnel will contact the contractor’s National Medical Director or Deputy Medical Director directly.
[19]We visited 31 CBP facilities along the southwest border. Of those 31 facilities, 28 had contracted medical personnel onsite and 3 did not. We requested that contracted medical personnel call the supervising physician or pediatric advisor at 23 of the 28 facilities, and the physicians answered 100 percent of the time.
[20]We visited 31 CBP facilities along the southwest border. Of those 31 facilities, 28 had contracted medical personnel onsite and 3 did not. We asked about medical supplies at 21 out of the 28 facilities, and the contracted medical personnel answered they had the medical supplies they needed 100 percent of the time.
[21]CBP’s directive states these requirements are subject to the availability of resources and operational dynamics.
[22]U.S. Customs and Border Protection, Medical Process Guidance (June 2023). The 2023 CBP medical process guidance further elaborated that if pregnant individuals choose not to receive a medical assessment, then contracted medical personnel must document the pregnant individual’s decision in the electronic medical records system. The guidance states that individuals who need a medical assessment may be referred to a medical provider in the local health system if there are no contracted medical personnel at the CBP facility. While one of the health interview questions asks if individuals are pregnant, we use “individuals with a ‘yes’ health interview response” to refer to nonpregnant adults with an affirmative response to any other interview question.
[23]CBP did not have fields to record medical assessments or medical encounters in its electronic medical records system until November 9, 2020. Furthermore, while CBP’s new medical process guidance was issued in June 2023, it was implemented on a rolling basis across the southwest border through August 2023. We gathered data through August 2024, which was the most recent data available at the time of our request. Additionally, we report results for individuals in custody with complete data and matching records. For example, we excluded records with missing data in the variables we used (e.g., missing age) or records that did not match between the electronic medical records system and processing systems.
[24]While one of the health interview questions asks if individuals are pregnant, we use “individuals with a ‘yes’ health interview response” to refer to nonpregnant adults with an affirmative response to any other interview question.
[25]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: Sept. 10, 2014).
[26]U.S. Customs and Border Protection, National Standards on Transport, Escort, Detention, and Search (TEDS) (Oct. 2015).
[27]As of July 2025, CBP officials stated they are making updates and changes to TEDS.
[28]In the May 2023 memorandum, CBP defined at-risk or medically fragile individuals to include individuals with a chronic illness; infants; elderly individuals; minors with an acute injury, medical or mental health condition; pregnant individuals; individuals with complications after giving birth; and individuals with a disabling mental disorder. In the October 2023 memorandum, CBP stated individuals designated medically at-risk by contracted medical personnel (i.e., elevated in-custody medical risk) should continue to be expeditiously processed to minimize the length of time they spend in CBP custody.
[29]U.S. Customs and Border Protection, Rescission of Legacy Policies Related to Care and Custody (Washington, D.C.: May 5, 2025).
[30]Exec. Order No. 14165, 90 Fed. Reg. 8467 (Jan. 20, 2025).
[31]Contracted medical personnel designate whether an individual presents high in-custody medical risk while in CBP custody based on certain diagnoses including chest pain, heat stroke, or an abdominal open wound, among other things. Therefore, this analysis only includes individuals that saw contracted medical personnel for these risk designations while in CBP custody. For this analysis, we compared individuals who were designated “red” medical risk, the highest level of risk, throughout their time in custody (6,755 individuals) with individuals who were designated “green,” the lowest level of medical risk (58,713 individuals). We did not include individuals whose risk level changed during their time in custody (e.g., individuals who were initially designated red and were later downgraded to lower levels of risk, such as orange, yellow, or green).
[32]We included results for individuals in custody with complete data and matching records. For example, we excluded records with missing data in the variables we used (e.g., missing a unique identifier) or records that did not match between the electronic medical records system and processing systems.
[33]Border Patrol’s processing system is e3 and OFO’s processing system is Unified Secondary. CBP personnel collect custodial information from individuals in custody and input that information into their respective systems, such as an individual’s date of birth, sector and station they were held, time-in-custody, and medication information.
[34]CBP’s Office of the Chief Medical Officer Medical Process Guidance Annex A: Elevated in-Custody Medical Risk (October 2023) states medically high-risk individuals shall be evaluated by a medical provider who then must consult with a supervising physician or pediatric advisor, shall be evaluated for medical isolation, shall have their condition documented in the electronic medical records system, and shall have their condition communicated to CBP for consideration for expedited processing.
[35]Officials at the remaining facilities either did not provide a specific frequency of medical checks or did not have contracted medical personnel.
[36]As previously mentioned, CBP issued a medical process guidance addendum in October 2023. CBP’s electronic medical records data began tracking the newly required enhanced medical monitoring actions on October 12, 2023. We gathered data through August 2024, when the most recent data were available at the time of our request.
[37]Specifically, tender-age children received the checks 43 percent of the time, non-tender age children received the checks 41 percent of the time, and adults received the checks 45 percent of the time. For this analysis, we defined medically high-risk children and adults as individuals who were designated “red” medical risk, the highest level of risk, throughout their time in custody. We did not include individuals whose risk level changed during their time in custody (i.e., individuals who were initially designated red and were later downgraded to a lower level of risk, such as orange, yellow, or green). We calculated the time between each enhanced monitoring check for each individual. If the time between checks was 4 hours or less, we counted it as an instance of having received the required check on time. Otherwise, it was counted as an instance of not meeting the requirement. We then calculated the total number of checks performed on time out of the total number of monitoring checks. We included results for individuals in custody with complete data and matching records. For example, we excluded records of individuals with medical encounter information, including risk designation, that did not match with enhanced medical checks in the electronic medical records system.
[38]The remaining three facilities did not have contracted medical personnel.
[40]According to the October 2023 addendum to the CBP medical process guidance, for medically high-risk children, a contracted medical provider must consult with a pediatric advisor (or supervising physician) within 20 minutes to determine the treatment plan, including the potential need for immediate medical transport for outside care. Contracted medical personnel are able to input whether or not they contacted a pediatric advisor in the electronic medical records system.
[41]DHS’s Office of Health Security previously indicated that CBP should improve awareness of day-to-day clinical operations. Specifically, after reviewing CBP’s medical policies and procedures following the death of the 8-year-old girl in May 2023, DHS’s Acting Chief Medical Officer at that time found that OCMO lacked visibility regarding the contract supervising physician’s role and involvement.
[42]For instance, CBP reduced the number of facilities with contracted medical personnel from 79 facilities in July 2024 to 44 facilities in May 2025. As such, CBP no longer monitors whether certain individuals required to get medical assessments received them at the 35 facilities along the southwest border that no longer have contracted medical personnel.
[44]U.S. Customs and Border Protection, National Standards on Transport, Escort, Detention, and Search (TEDS) (Oct. 2015).
[45]U.S. Customs and Border Protection, CBP Directive 5240-010: Short-Term Holding Facilities Handling Storage, Transference, and/or Return of Detainee Personal Property (Aug. 2024) and U.S. Customs and Border Protection, Office of the Chief Medical Officer Medical Process Guidance (June 2023).
[46]U.S. Customs and Border Protection, Office of the Chief Medical Officer, CBP Form 2501 Medical Summary Documentation Memorandum (Jan. 2025).
[47]CBP extended the Bridge II contract again through September 27, 2025, and then awarded the Bridge III medical services contract on September 28, 2025, after we provided DHS with our draft report for review and comment. Thus, we did not include the Bridge III contract within the scope of our review.
[48]Department of Homeland Security, Homeland Security Acquisition Manual (Oct. 2009) (incorporating change 2024-07, July 31, 2024).
[49]Department of Homeland Security, Developing and Managing Contract Requirements Desk Guide for the Acquisition Workforce.
[50]A statement of work typically outlines the specific work that the contractor is to accomplish in a contract and the responsibilities of the contractor.
[51]The DHS Office of the Immigration Detention Ombudsman recommended that CBP personnel with oversight responsibilities for the medical services contract be required to notify senior leadership when medical staffing levels fall below a certain monthly percentage. CBP also concurred with this recommendation. Department of Homeland Security, Office of the Immigration Detention Ombudsman, OIDO-23-008.
[52]Subsequently, CBP awarded the Bridge III medical services contract on September 28, 2025, after we provided DHS with our draft report for review and comment. Thus, we did not include the Bridge III contract within the scope of our review.
[53]Cost-effectiveness analyses and cost-benefit analyses are two economic evaluation approaches that can be used to identify, measure, value, and compare the costs of public health interventions. See Centers for Disease Control and Prevention, Office of the Associate Director for Policy and Strategy, Economic Evaluation, accessed July 10, 2025, https://www.cdc.gov/polaris/php/economics/cost-effectiveness.html.
[54]Contracted medical personnel consist of medical providers, such as nurse practitioners and physician assistants, and medical support staff, such as emergency medical technicians and paramedics.
[55]The 2023 CBP medical process guidance states pregnant individuals in custody will be offered a medical assessment. If they refuse, contracted medical personnel must document the pregnant individual’s decision in the electronic medical records system and CBP personnel must document it in their respective processing systems.
[56]Department of Homeland Security, U.S. Customs and Border Protection, CBP Procurement Directorate Acquisition Alert: Contract Administration (May 21, 2021). CBP awarded the 2020 medical services contract in September 2020, prior to the May 2021 acquisition alert, but CBP awarded the two bridge contracts after the May 2021 acquisition alert went into effect.
[57]For examples, see GAO, Customs and Border Protection: Actions Needed to Enhance Acquisition Management and Knowledge Sharing, GAO‑23‑105472 (Washington, D.C.: Apr. 25, 2023); GAO, Project Management: DOE and NNSA Should Improve Their Lessons-Learned Process for Capital Asset Projects, GAO‑19‑25 (Washington, D.C.: Dec. 21, 2018); and Project Management Institute, Inc., A Guide to the Project Management Body of Knowledge (PMBOK® Guide), Seventh Edition (2021). PMBOK is a trademark of Project Management Institute, Inc.
[59]CBP’s Office of Acquisition officials stated that the payment amount did not go over the initial budget that CBP planned for the medical services effort.
[60]The government is not obligated to pay the contractor for any amount exceeding the ceiling price in the schedule, and the contractor shall not be obligated to continue performance if doing so would exceed the ceiling price set forth in the schedule, unless and until the contracting officer notifies the contractor in writing that they are increasing the ceiling price and specifies the revised ceiling in the notice. Any hours expended, and material costs incurred by the contractor exceeding the ceiling price before the increase shall be allowable to the same extent as if the hours expended and material costs had been incurred after the increase in the ceiling price. FAR 52.232-7(e). A schedule is a set of contracts awarded to multiple vendors that provide similar products and services. See FAR 8.401. We did not identify additional instances of CBP exceeding its estimated cost ceiling in the two subsequent 2023 bridge contracts.
[61]According to FAR 17.207(f), before exercising an option, the contracting officer shall make a written determination for the contract file that exercise is in accordance with the terms of the option.
[62]The CBP offices with oversight responsibilities for the medical services contract include the Office of the Chief Medical Officer’s Border Health Systems Division, the Acquisition Management Division, and the Office of Acquisition.
[63]Department of Homeland Security Office of the Chief Procurement Officer, Contracting Officer’s Representative (COR) Guidebook (Oct. 2024); and U.S. Customs and Border Protection, CBP Procurement Directorate Acquisition Alert (May 2021).
[64]The initial value of $311 million was the total value at the time of award in November 2023. CBP’s total obligations, including extensions to the contract and other factors, was $403 million as of August 2025.
[65]Contracting officers may appoint a COR by letter of appointment, which delegates and outlines specific contract administration functions the COR is responsible for performing for the contracting officer.
[66]A staffing report includes information on the contractor’s recruitment efforts and any issues with the background clearance process.
[67]GAO, Border Security: DHS Needs to Better Plan for and Oversee Future Facilities for Short-term Custody, GAO‑25‑107346 (Washington, D.C.: Sept. 2, 2025).
[68]DHS guidance refers to these officials as technical monitors. However, officials from CBP’s Office of the Chief Medical Officer referred to the Border Patrol agents and Office of Field Operations officers performing this role as task order monitors. We confirmed with CBP that these roles are equivalent. Therefore, for the purpose of this report, we refer to CBP officials fulfilling the equivalent role of a technical monitor as “task order monitors.”
[69]Department of Homeland Security, Office of the Chief Procurement Officer, Acquisition Workforce Certification Program: Federal Acquisition Certification for Contracting Officer’s Representatives, Acquisition Workforce Policy-064-04-001-03 (Aug. 11, 2025).
[70]We recently identified similar issues with the use of technical monitors on other CBP contracts, as well as contracts with the Federal Emergency Management Agency. For more information, see GAO‑25‑107346 and GAO, Disaster Contracting: Opportunities Exist for FEMA to Improve Oversight, GAO‑25‑107136 (Washington, D.C.: Feb. 6, 2025).
[71]Contractor Performance Assessment Reporting System guidance defines annual evaluations as interim evaluations and evaluations upon the completion of the work as final evaluations.
[72]FAR 42.1502. An April 2025 executive order directs agencies to streamline the federal acquisition regulations that govern federal procurement. Exec. Order No. 14275, 90 Fed. Reg. 16,445 (Apr. 18, 2025).
[73]General Services Administration, Guidance for the Contractor Performance Assessment Reporting System (CPARS) (July 2024). The Contractor Performance Assessment Reporting System is an evaluation reporting tool for all past performance on government contracts and orders.
[74]After we provided our draft report to DHS for review and comment, CBP provided documentation that it had extended the Bridge II contract again through September 27, 2025. As a result, the past performance evaluation will now cover a 22-month period of performance.
[75]U.S. Customs and Border Protection, Office of the Chief Medical Officer, Medical Quality Management Guidance and Instruction (Feb. 2023).
[76]According to CBP officials, CBP and the medical services contractor agreed to the Medical Quality Management Program elements in 2020, but our review of the records indicated that they were documented in fiscal year 2022.
[77]A sentinel event is an unexpected occurrence involving a person in custody who experiences death or a serious physical and/or psychological injury or illness, not related to the natural course of their illness or condition.
[78]U.S. Customs and Border Protection Office of the Chief Medical Officer, Medical Sentinel Event Review Processes (Dec. 2023).
[79]The Joint Commission is the largest accrediting body with various standards and guidance for hospitals and other healthcare facilities, including the Department of Defense’s military health system.
[80]The Joint Commission, Comprehensive Accreditation Manual for Hospitals (Jan. 2024).
[81]CBP defines encounters as the sum of (1) noncitizens who are not lawfully in the U.S. whom Border Patrol apprehended; (2) noncitizens encountered at ports of entry whom OFO determined to be inadmissible; and (3) noncitizens processed for expulsions as part of CBP’s efforts to aid the Centers for Disease Control and Prevention in enforcing its authority under 42 U.S.C. § 265. See 42 U.S.C. § 268(b); 42 C.F.R. § 71.40. Title 42 expulsions began on March 21, 2020, and ended on May 11, 2023. The number of encounters could reflect unique individuals encountered more than once.
[82]At our request, CBP’s Office of Field Operations (OFO) provided a list of local nonprofit or nongovernmental organizations it coordinates and works with, in circumstances when noncitizens are released from OFO custody. GAO selected the first organization listed for each of the three OFO field offices to contact. Additionally, one organization was referred to us by an nongovernmental organization we interviewed. We interviewed the following four nongovernmental organizations: Asylum Seeker Screening and Stabilization Program through the University of California San Diego Herbert Wertheim School of Public Health; Catholic Charities of San Diego and Laredo; SAMU First Response; and Jewish Family Service of San Diego.
[83]U.S. Customs and Border Protection, National Standards on Transport, Escort, Detention, and Search (TEDS) (Oct. 2015).
[84]Border Patrol’s processing system is e3 and OFO’s processing system is USEC. CBP personnel collect custodial information from individuals in custody and input that information into their respective systems, such as an individual’s date of birth, sector and station they were held, time-in-custody, and medication information. We gathered data through August 2024, which was the most recent data available at the time of our request.
[85]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: Sept. 10, 2014).
[86]In October 2023, CBP OCMO’s medical process guidance addendum added risk designations and specific care requirements for the individuals in custody. We gathered data through August 2024, which was the most recent data available at the time of our request.
[87]U.S. Customs and Border Protection, National Standards on Transport, Escort, Detention, and Search (TEDS) (Oct. 2015).
[88]Department of Homeland Security, Homeland Security Acquisition Manual (Oct. 2009) (incorporating change 2024-07, July 31, 2024) and U.S. Customs and Border Protection, Contract Administration, CBP Procurement Directorate Acquisition Alert: 2021-05 (May 21, 2021).
[89]GAO, Standards for Internal Control in the Federal Government, GAO‑14‑704G (Washington, D.C.: Sept. 10, 2014).
[90]Department of Homeland Security, Office of the Chief Procurement Officer, Contracting Officer’s Representative (COR) Guidebook (Oct. 2024); and Department of Homeland Security, Developing and Managing Contract Requirements Desk Guide for the Acquisition Workforce (Apr. 2021).
[91]General Services Administration, Guidance for the Contractor Performance Assessment Reporting System (CPARS) (July 2024); FAR 42.1502; and FAR 42.1503(a)(1)(iii).
[92]Centers for Disease Control and Prevention, Office of the Associate Director for Policy and Strategy, Economic Evaluation, accessed July 10, 2025, https://www.cdc.gov/polaris/php/economics/cost-effectiveness.html.
[93]The Joint Commission, Comprehensive Accreditation Manual for Hospitals (Jan. 2024); U.S. Customs and Border Protection Office of the Chief Medical Officer, Medical Sentinel Event Review Processes (Dec. 2023); and Medical Quality Management Guidance and Instruction (Feb. 2023).
