COVID-19
Lessons Can Help Agencies Better Prepare for Future Emergencies
Report to Congressional Committees
August 2024
GAO‑24‑107175
United States Government Accountability Office
View GAO‑24‑107175. For more information, contact Jessica Farb at (202) 512-7114 or FarbJ@gao.gov.
Highlights of GAO‑24‑107175, a report to congressional committees
August 2024
COVID-19
Lessons Can Help Agencies Better Prepare for Future Emergencies
Why GAO Did This Study
The COVID-19 pandemic brought significant challenges to the nation's public health and economy. Since March 2020, Congress has provided about $4.65 trillion in federal funds to help the nation respond to and recover from the pandemic. Agencies across the government have worked to implement the federal response.
The CARES Act includes a provision for GAO to report regularly on the public health and economic effects of the pandemic and the federal response. This report includes updates on the public health effects and economic conditions since the pandemic, including updates on federal COVID-19 relief funding. It also describes lessons learned from the pandemic that could help federal agencies better prepare for future emergencies.
To describe lessons learned for federal agencies, GAO analyzed issued GAO reports. GAO also collected information on agency actions to address GAO COVID-19 recommendations.
What GAO Recommends
GAO is making one new recommendation to the Department of the Treasury to include key lessons from the COVID-19 emergency financial assistance provided to the aviation industry in its efforts to compile resources to prepare for future financial disasters. A Treasury official told us that Treasury agrees with our recommendation and will take steps to implement it.
What GAO Found
The nation continues to recover from the public health and economic effects of the COVID-19 pandemic. For example, COVID-19 was the tenth leading cause of death in 2023, as compared to being the third leading cause of death in 2020 and 2021. Available data also show that inflation declined between March 2023 and March 2024, but remained higher than pre-pandemic levels.
GAO identified lessons from the COVID-19 pandemic that could help federal agencies better prepare for, respond to, and recover from future emergencies. These lessons draw on GAO’s COVID-19 oversight work, which includes 428 recommendations to federal agencies and 24 matters for congressional consideration as of April 2024. Of these recommendations, 220 remain open. Moreover, these recommendations include those related to the three areas GAO added to its High Risk List during the COVID-19 public health emergency:
1. the Department of Health and Human Services’ leadership and coordination of public health emergencies,
2. the Department of Labor’s Unemployment Insurance system, and
3. the Small Business Administration’s emergency loans to small businesses.
Agencies across the government could improve their preparedness for future emergencies by fully implementing GAO’s recommendations.
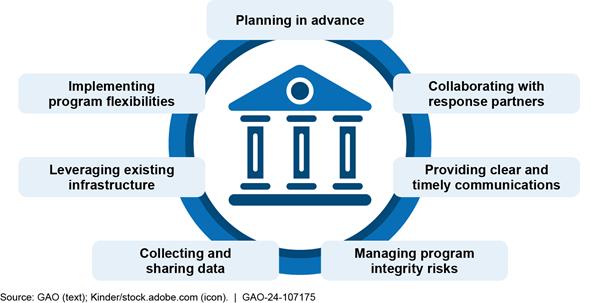
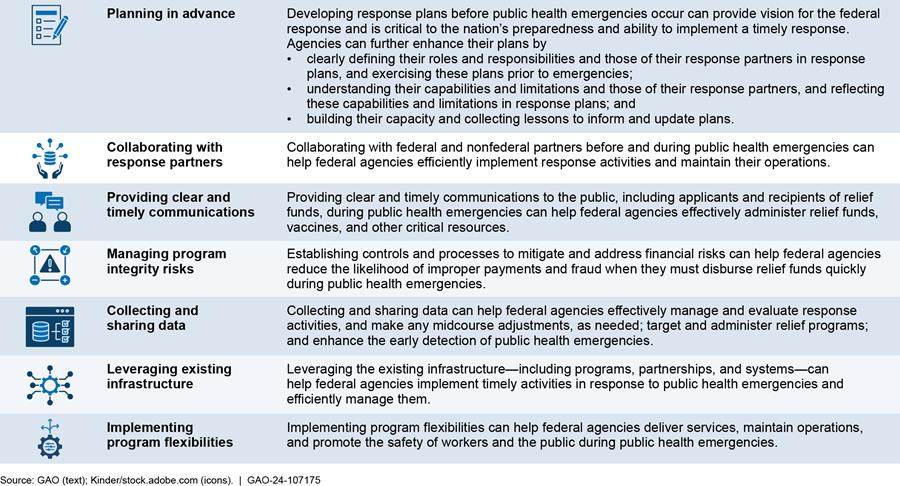
Lessons that could help federal agencies better prepare for future emergencies fall into seven topic areas. These lessons highlight instances where government agencies did well in responding to the pandemic, as well as instances where the government response could have been much better.
|
|
PLANNING IN ADVANCE Advanced plans—including national-level strategies and department- and agency-level plans—provide vision for how the federal government will respond to public health emergencies and are critical to the nation’s preparedness and ability to implement a timely response. Agencies can further enhance their preparedness by · clearly defining their roles and responsibilities and those of their response partners in response plans, and exercising these plans prior to emergencies; · understanding their capabilities and limitations and those of their response partners, and reflecting these capabilities and limitations in response plans; and · building their capacity and collecting lessons to inform and update plans. GAO found instances where federal agencies could improve their preparedness by taking such steps. For example, the Department of the Treasury has not incorporated lessons GAO identified from the COVID-19 assistance programs to the aviation industry into its efforts to compile resources to prepare for future financial disasters. Taking such steps could help Treasury make timely decisions and avoid encountering past challenges when responding to future emergencies. Further, GAO has made recommendations to federal agencies to improve their emergency response plans. For example, GAO recommended that the Department of Health and Human Services develop plans outlining steps to mitigate shortages in needed medical supplies, develop a comprehensive testing strategy, and develop an approach for assessing and addressing known challenges and future risks associated with advanced development and manufacturing of medical countermeasures, including vaccines. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
COLLABORATING WITH RESPONSE PARTNERS Collaborating with response partners—including federal and nonfederal partners—before and during public health emergencies can help agencies efficiently implement response activities and continue operations. Federal agencies can facilitate this collaboration by identifying partners key to implementing the response, regularly coordinating with identified partners, and ensuring partners understand their roles and responsibilities in implementing the response. GAO has made recommendations to agencies across the federal government to improve their collaboration with response partners. For example, GAO recommended that the Department of Health and Human Services share its plans to mitigate medical supply shortages with response partners and maintain up-to-date guidance for partners on requesting and receiving assets from the Strategic National Stockpile. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
PROVIDING CLEAR AND TIMELY COMMUNICATIONS Federal agencies can enhance their efforts to effectively administer relief funds, vaccines, and other critical resources during a public health emergency by providing clear and timely information to · applicants and eligible entities of federal relief funds, · recipients of federal relief funds, and · the public. GAO has made recommendations to federal agencies to improve their communications during public health emergencies. For example, GAO recommended that the Small Business Administration develop a comprehensive strategy for communicating with potential and actual program applicants in the event of an emergency. GAO stated that its strategy should include guidelines for the types of information and timing of information to be provided to program participants throughout an emergency. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
MANAGING PROGRAM INTEGRITY RISKS Establishing controls and processes can help federal agencies manage program integrity risks when they must disburse emergency relief funds quickly during an emergency. Specifically, prepayment controls and processes can help agencies minimize the likelihood of improper payments and fraud. Further, postpayment controls and processes can help agencies identify and recover improper and fraudulent payments when the quick disbursement of funds makes prepayment controls difficult to apply fully. GAO has made recommendations to federal agencies to better manage program integrity risks in emergency assistance programs. For example, GAO recommended that the Department of Labor design and implement an antifraud strategy for unemployment insurance programs that is consistent with leading practices outlined in GAO’s Fraud Risk Framework. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
COLLECTING AND SHARING DATA Collecting and sharing data can help federal agencies · effectively manage response activities, evaluate performance in meeting response program goals, and make midcourse adjustments as needed; · target and administer relief fund programs; and · enhance the early detection of public health emergencies. GAO has made recommendations to federal agencies to enhance their ability to collect and share data before and during public health emergencies. For example, GAO recommended that the Department of Health and Human Services develop a plan to establish an electronic nationwide public health situational awareness network and identify measurable steps for completing this network. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
LEVERAGING EXISTING INFRASTRUCTURE Leveraging the existing infrastructure—including programs, partnerships, and systems—can help federal agencies implement timely activities to respond to a public health emergency and efficiently manage them. Specifically, federal agencies can use existing infrastructure to facilitate the delivery of services, distribute federal relief funds, and manage and oversee response programs. GAO identified instances during the COVID-19 pandemic where federal agencies successfully leveraged the existing infrastructure. For example, the Department of the Interior and the Indian Health Service leveraged existing program mechanisms to efficiently distribute COVID-19 relief funds to tribal recipients during the pandemic. GAO has made recommendations to federal agencies to seek such opportunities. Further, GAO suggested that Congress consider enacting automatic increases in federal Medicaid spending during economic downturns to increase federal Medicaid support in a more timely and targeted fashion. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
|
|
IMPLEMENTING PROGRAM FLEXIBILITIES Implementing flexibilities—such as telehealth and telework—during a public health emergency can help federal agencies · deliver services to program beneficiaries, · maintain activities to support critical operations, and · promote the safety of workers and the public. GAO has recommended that federal agencies examine the extent to which flexibilities utilized during the COVID-19 pandemic could be incorporated in standard operations or used during future emergencies. For example, GAO recommended that the Food and Drug Administration fully assess whether and how alternative tools could help meet drug oversight objectives when in-person inspections are not possible in the future. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
This is a work of the U.S. government and is not subject to copyright protection in the United States. The published product may be reproduced and distributed in its entirety without further permission from GAO. However, because this work may contain copyrighted images or other material, permission from the copyright holder may be necessary if you wish to reproduce this material separately.
Abbreviations
ASPR Administration for Strategic Preparedness and Response
CDC Centers for Disease Control and Prevention
CFO chief financial officer
CIADM Centers
for Innovation and Advance Development and
Manufacturing
CMS Centers for Medicare & Medicaid Services
CPI Consumer Price Index
DHS Department of Homeland Security
DOD Department of Defense
DOL Department of Labor
DOT Department of Transportation
FDA Food and Drug Administration
FEMA Federal Emergency Management Agency
HHS Department of Health and Human Services
HRSA Health Resources and Services Administration
IRS Internal Revenue Service
OMB Office of Management and Budget
SBA Small Business Administration
SIGPR Office
of the Special Inspector General for Pandemic
Recovery
SLFRF Coronavirus State and Local Fiscal Recovery Funds
USDA United States Department of Agriculture
VA Department of Veterans Affairs
VHA Veterans Health Administration
August 1, 2024
Congressional Committees
The COVID-19 pandemic was an unprecedented global crisis resulting in about 1.2 million reported deaths in the U.S. as of April 27, 2024.[1] While the Secretary of the Department of Health and Human Services (HHS) terminated the federal public health emergency on May 11, 2023, the nation is still recovering from the public health and economic effects of the pandemic while working to identify and respond to new COVID-19 variants.[2]
Since March 2020, the CARES Act and five additional laws provided about $4.65 trillion in federal funding to help the nation respond to and recover from the pandemic.[3] The COVID-19 response included a focus on mitigating COVID-19 health risks and providing federal assistance to support individuals and public and private entities. Agencies across the federal government worked to implement this federal response.
The CARES Act includes a provision for GAO to report regularly on the public health and economic effects of the pandemic and the federal response.[4] We have issued 11 comprehensive reports examining the federal government’s continued efforts to respond to and recover from the COVID-19 pandemic. In addition, we have issued over 200 standalone reports, testimonies, and science and technology spotlights focused on different aspects of the pandemic.
In our body of work on COVID-19 oversight, we have made 428 recommendations to federal agencies in addition to 24 matters for congressional consideration to improve implementation, oversight, and transparency of the federal response. We also made recommendations to federal agencies to better prepare for future emergencies. As of April 2024, 220 of the recommendations from our COVID-19 oversight work remain open. Federal agencies had fully addressed 198 of these recommendations and partially addressed 35 of these recommendations.[5] Additionally, Congress has taken steps to fully address two matters for congressional consideration.
The 428 recommendations from our COVID-19 oversight work include several we have made to agencies related to the three areas we added to our High Risk List during the COVID-19 public health emergency: (1) HHS’s leadership and coordination of public health emergencies, (2) the Department of Labor’s (DOL) Unemployment Insurance system, and (3) the Small Business Administration’s (SBA) emergency loans to small businesses.[6] For example, we recommended
· HHS should develop a coordinated, department-wide action program that encourages collaboration within HHS and includes external stakeholders involved with the public health response to identify and resolve challenges.[7]
· DOL should develop and implement an antifraud strategy for Unemployment Insurance programs that is consistent with leading practices for preventing, detecting, and responding to fraud outlined in GAO’s Fraud Risk Framework.[8]
· SBA should ensure that it has identified external sources of data that can facilitate the verification of applicant information and the detection of potential fraud across programs, including loans made under the Paycheck Protection Program and the COVID-19 Economic Injury Disaster Loan program.[9]
This report includes key data updates on the public health effects and economic conditions following the COVID-19 pandemic and the federal response, including data updates on federal COVID-19 relief funding and spending. It also describes lessons from the pandemic that could help federal agencies better prepare for future emergencies.
To describe lessons from the COVID-19 pandemic that could help federal agencies better prepare for future emergencies, we reviewed and analyzed GAO reports and recommendations, including comprehensive and standalone CARES Act reports. We reviewed additional selected documents, such as a report from the Office of the Special Inspector General for Pandemic Recovery (SIGPR) on COVID-19 relief funds provided to the aviation industry and public statements from the Department of Justice on federal fraud-related cases involving federal COVID-19 relief programs.[10] We also interviewed officials from the Department of the Treasury and collected information from various federal agencies, including HHS, to identify actions they have taken as of April 2024 to resolve some of our recommendations, such as recommendations from our CARES Act reports.
We conducted this performance audit from November 2023 to August 2024 in accordance with generally accepted government auditing standards. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on our audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Updates to Public Health, Economic, and Federal COVID-19 Relief Funding and Spending Data
Public Health Effects of the COVID-19 Pandemic
In our comprehensive reports, we tracked data related to the public health effects of the COVID-19 pandemic. The following are updates to key data discussed in those reports.
Mortality
Over the course of the pandemic, the U.S. experienced multiple peaks and lulls in the weekly counts of COVID-19-associated deaths—a key indicator of COVID-19 severity—according to data from the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics.[11] The highest weekly numbers of COVID-19-associated deaths occurred in January 2021 (with about 26,000 deaths) followed by January 2022 and April 2020. Since mid-2022, weekly COVID-19-associated deaths have been much lower, with the peak in January 2023 reaching about 3,900 deaths, according to the latest available data as of May 1, 2024. See figure 1.
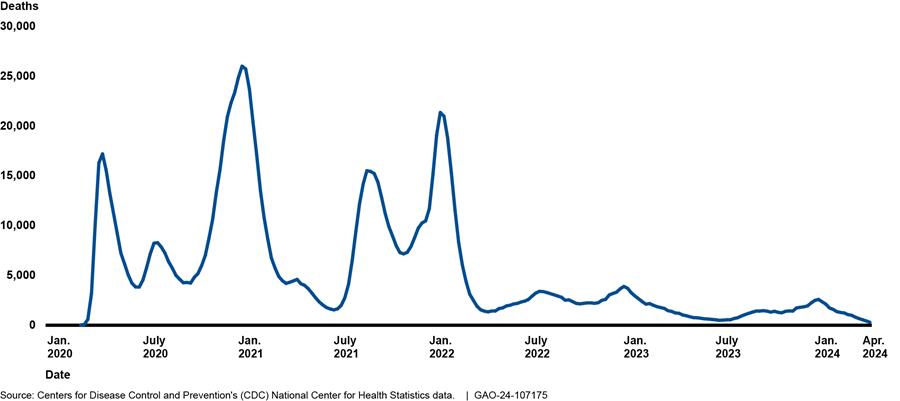
Note: COVID-19-associated deaths are those with COVID-19 listed as an underlying (i.e., primary) or contributing cause of death using the International Classification of Diseases, Tenth Revision (code U07.1). Data are from CDC WONDER as of May 1, 2024. Death counts for certain weeks prior to March 7, 2020, were suppressed due to small numbers. Data for 2020 and 2021 are final. Data from 2022 through April 2024 are provisional and subject to change.
Likewise, annual rates of COVID-19-associated deaths were higher in 2020 and 2021 than in 2022 and 2023. The rate of COVID-19-associated deaths was about 116.7 deaths per 100,000 U.S. residents in 2020 and peaked at 139.3 in 2021 before falling to 73.7 in 2022 and 22.4 in 2023. COVID-19 was the third leading cause of death in 2020 and 2021, fourth in 2022, and tenth in 2023.[12]
Hospitalizations
Over the course of the pandemic, surges in COVID-19 cases have stressed hospital systems and negatively affected health care and public health infrastructure, according to CDC. Similar to COVID-19-associated deaths, the U.S. experienced peaks and lulls in the level of COVID-19 hospitalizations. At its height in January 2022, the number of adult and pediatric patients with confirmed cases of COVID-19 occupying hospital beds rose to nearly 152,000, with a subsequent peak being much lower. COVID-19 hospitalizations reached approximately 42,000 in January 2023. COVID-19 hospitalizations then fell to just under 5,500 in June 2023 before rising again to approximately 30,600 in January 2024. Since January 2024, COVID-19 hospitalizations have steadily declined and totaled less than 5,000 at the end of April 2024.[13] As of May 1, 2024, hospitals are no longer required to report COVID-19 hospital admissions, among other COVID-19-related indicators, to HHS. However, CDC encourages ongoing, voluntary reporting of hospitalization data.
Long COVID
One public health effect of COVID-19 is long COVID, or post-COVID conditions, which, according to CDC, refers to signs, symptoms, and conditions that continue or develop after an initial COVID-19 infection. According to estimates from the Census Bureau’s Household Pulse Survey, conducted April 2 through April 29, 2024, about 18 percent of adults in the U.S. aged 18 and older had experienced long COVID, and about 5 percent were experiencing it at the time of the survey.[14] CDC and other researchers have used multiple approaches to estimate how many people experience long COVID. According to CDC, estimates from these different approaches can vary widely depending on factors such as who was included in the study, as well as how and when the study collected information.
Economic Conditions following the COVID-19 Pandemic
In our comprehensive reports, we tracked data related to the economic conditions following the COVID-19 pandemic. The following updates describe selected trends we observed since the pandemic.
The national economy has continued to recover from the economic downturn of early 2020, sparked by the COVID-19 pandemic. However, economic growth has slowed from its 2021 rate, according to the Bureau of Economic Analysis. Real gross domestic product grew by 5.8 percent in 2021, but slowed to 1.9 percent in 2022, 2.5 percent in 2023, and 1.6 percent annual rate in the first quarter of 2024. The increase in the first quarter of 2024 primarily reflected increases in consumer spending, housing and business investment, and state and local government spending. The strength of the national economic recovery will depend on factors such as evolving geopolitical tensions and monetary policy actions.
Based on data covering price trends through March 2024, inflation had declined compared with a year ago but remained elevated compared with pre-pandemic levels.[15] Annual inflation indicators were 2.7 percent or higher in March 2024, which was significantly lower than the 4.2 percent in March 2023.[16] Yet, inflation was still slightly higher than averages of about 2 percent in recent decades.[17]
Indicators of more recent price pressures, including indicators that focus on underlying inflation trends, have increased moderately. Specifically, underlying inflation trends ranged from 0.3 percent to 0.5 percent in January, February, and March 2024.[18] These monthly trends indicate a lack of further progress toward the easing of inflation in recent months.
The labor market has continued to recover from the pandemic, but job growth showed signs of cooling according to DOL data on unemployment and other labor market conditions through March 2024. The unemployment rate remained low at 3.8 percent in March 2024 and was only slightly higher than the 54-year record low of 3.4 percent in January 2023. Meanwhile, both the employment-to-population ratio and labor force participation rate have changed little over the past year and remained lower than in the pre-pandemic period.[19] Additionally, as of March 2024, hiring and job opening rates continued to fall over the past year, suggesting the labor market has gradually cooled.
Federal COVID-19 Relief Funding and Spending
Six laws provided about $4.65 trillion in funding to help the nation respond to and recover from the COVID-19 pandemic. See figure 2.
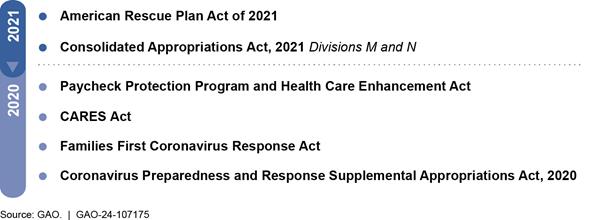
Note: The COVID-19 relief laws consist of the six laws providing comprehensive relief across federal agencies and programs that the Department of the Treasury uses to record and track COVID-19 relief spending, in accordance with guidance issued by the Office of Management and Budget.
In our comprehensive reports, we presented data tracking how agencies were obligating and expending COVID-19 relief funding. The following are updates to these data as of April 30, 2024, the most recent date for which government-wide information was available at the time of our analysis.
The federal government obligated a total of $4.57 trillion of the $4.65 trillion in COVID-19 relief funding, as reported by federal agencies to Treasury, in accordance with Office of Management and Budget (OMB) guidance.[20] Further, the federal government had expended about $4.41 trillion of this COVID-19 relief funding. For the top nine spending areas, agencies reported that COVID-19 relief funding obligations totaled $3.69 trillion (81 percent of total obligations), and expenditures totaled $3.61 trillion.[21] Table 1 provides additional details on government-wide COVID-19 relief funding, obligations, and expenditures by major spending areas as of April 30, 2024.
|
Major spending area (dollars in billions) |
COVID-19 relief funding |
Total |
Total |
|
Economic Impact Payments (Department of the Treasury) |
859.8 |
859.3 |
859.3 |
|
Business Loan Programs (Small Business Administration) |
830.0 |
828.1 |
828.0a |
|
Unemployment Insurance (Department of Labor) |
697.9 |
697.5 |
689.0 |
|
Coronavirus State and Local Fiscal Recovery Funds (SLFRF) (Department of the Treasury) |
350.0 |
349.9 |
349.9b |
|
Public Health and Social Services Emergency Fund (Department of Health and Human Services) |
337.3 |
332.6 |
298.6 |
|
Education Stabilization Fund (Department of Education) |
277.3 |
277.3 |
236.0 |
|
Coronavirus Relief Fund (Department of the Treasury) |
150.0 |
149.9 |
149.8 |
|
Supplemental Nutrition Assistance Programs (Department of Agriculture) |
121.0 |
98.4 |
102.3c |
|
U.S. Coronavirus Refundable Credits (Department of the Treasury) |
98.8 |
92.2 |
92.2 |
|
Other areas (includes over 300 accounts)d |
927.7 |
883.4 |
803.9 |
|
Totale |
4,649.9 |
4,568.5 |
4,408.9 |
Source: GAO analysis of data from the Department of the Treasury and applicable agencies. | GAO‑24‑107175
Note: COVID-19 relief funding, obligation, and expenditure data shown for the major spending areas are based on data reported by applicable agencies to Treasury’s Governmentwide Treasury Account Symbol Adjusted Trial Balance System. Federal agencies use this system to provide proprietary financial reporting and budgetary execution information to Treasury. These amounts can fluctuate from month to month. COVID-19 relief funding is the cumulative amount of funding provided in the six COVID-19 relief laws that Treasury uses to record and track COVID-19 relief spending, in accordance with Office of Management and Budget guidance. Further, the $4.65 trillion total reflects rescissions of COVID-19 relief funding enacted in the Fiscal Responsibility Act of 2023, Pub. L. No. 118-5, 137 Stat. 10, 23-30, div. B, tit. I (2023), and other laws. The most recent date for which government-wide information was available at the time of GAO’s analysis was April 30, 2024.
aThe Small Business Administration’s Business Loan Program account includes activity for Paycheck Protection Program loan guarantees and certain other loan subsidies. These expenditures relate mostly to the loan subsidy costs (i.e., the loan’s estimated long-term costs to the U.S. government).
bMost of the SLFRF funds were allocated to states, the District of Columbia, and local governments. In April 2024, GAO reported that as of September 30, 2023, which was the most recently available data at the time of the report, states and the District of Columbia reported obligating 73 percent ($142.4 billion) and spending 53 percent ($103.7 billion) of their $195.8 billion in SLFRF awards. A total of 26,442 localities—including cities, counties, and smaller localities—reported obligating 64 percent ($80.1 billion) and spending 47 percent ($59.4 billion) of their $126.1 billion in SLFRF awards. See GAO, COVID-19 Relief: State and Local Fiscal Recovery Funds Spending as of September 30, 2023, GAO‑24‑107472 (Washington, D.C.: Apr. 10, 2024).
cDepartment of Agriculture officials told GAO that the Supplemental Nutrition Assistance Programs spending amounts were not reported to the Governmentwide Treasury Account Symbol Adjusted Trial Balance System correctly for April 2024. As a result, the reported expenditures are greater than the obligations. Agriculture is working to identify the error and correct these amounts for future reporting.
dSeveral provisions in the Families First Coronavirus Response Act and the American Rescue Plan Act of 2021 authorized increases in Medicaid payments to states and U.S. territories. At the time of enactment, the Congressional Budget Office estimated that federal expenditures from these provisions would total approximately $76.9 billion through fiscal year 2030. The largest increase to federal Medicaid spending is based on a temporary formula change rather than a specific appropriated amount. Some of the estimated costs in this total are for the Children’s Health Insurance Program, permanent changes to Medicaid, and changes not specifically related to COVID-19. This increased spending is not accounted for in the funding provided by the COVID-19 relief laws and is therefore not included in this table.
eAmounts shown in columns may not sum to the totals because of rounding.
As of April 30, 2024, $52.4 billion or 1 percent of the total amount of funding provided for COVID-19 relief remained available for obligation (unexpired unobligated balance). Additionally, $40.1 billion was expired (expired unobligated balance), meaning that this amount was not available for incurring new obligations but was available for recording eligible obligation adjustments. Table 2 provides additional details on funding, obligations, unobligated balances, and expenditures of government-wide COVID-19 relief funding with the largest unexpired unobligated balances.
|
Spending areas (dollars in billions) |
COVID-19 relief funding |
Total obligations |
Total expenditures |
Expired unobligated balance |
Unexpired unobligated balance |
|
Pension Benefit Guaranty Corporation Funda (Pension Benefit Guaranty Corporation) |
77.8 |
53.9 |
53.9 |
0.0 |
23.8 |
|
U.S. Coronavirus Refundable Credits (Department of the Treasury) |
98.8 |
92.2 |
92.2 |
0.0 |
6.8 |
|
Public Health and Social Services Emergency Fund (Department of Health and Human Services) |
337.3 |
332.6 |
298.6 |
0.0 |
4.7 |
|
Disaster Relief Fundb (Federal Emergency Management Agency) |
94.4 |
93.9 |
83.4 |
0.0 |
4.1 |
|
Tenant-Based Rental Assistance (Department of Housing and Urban Development) |
6.2 |
3.6 |
3.3 |
0.0 |
2.7 |
|
Emergency Connectivity Fund for Educational Connections and Devices (Federal Communications Commission) |
7.2 |
6.0 |
4.5 |
0.0 |
1.7 |
|
State Small Business Credit Initiative (Department of the Treasury) |
9.7 |
8.8 |
2.8 |
0.0 |
0.9 |
|
Centers for Disease Control and Prevention-Wide Activities and Program Support (Department of Health and Human Services) |
25.2 |
24.3 |
17.9 |
0.0 |
0.8 |
|
Other areas (includes over 250 accounts) |
3,993.3 |
3,953.2 |
3,852.4 |
40.0c |
6.9 |
|
Totald |
4,649.9 |
4,568.5 |
4,408.9 |
40.1 |
52.4 |
Source: GAO analysis of data from the Department of the Treasury and applicable agencies. | GAO‑24‑107175
Note: COVID-19 relief funding, obligation, and expenditure data shown for the major spending areas are based on data reported by applicable agencies to Treasury’s Governmentwide Treasury Account Symbol Adjusted Trial Balance System. Federal agencies use this system to provide proprietary financial reporting and budgetary execution information to Treasury. These amounts can fluctuate from month to month. COVID-19 relief funding is the cumulative amount of funding provided in the six COVID-19 relief laws that Treasury uses to record and track COVID-19 relief spending, in accordance with Office of Management and Budget guidance. Further, the $4.65 trillion total reflects rescissions of COVID-19 relief funding enacted in the Fiscal Responsibility Act of 2023, Pub. L. No. 118-5, 137 Stat. 10, 23-30, div. B, tit. I (2023), and other laws. The most recent date for which government-wide information was available at the time of GAO’s analysis was April 30, 2024.
aUnder section 9704 of the American Rescue Plan Act of 2021, classified at 29 U.S.C. 1305(i), 1432, the Pension Benefit Guaranty Corporation will receive the necessary funding from the General Fund of the U.S. Treasury through fiscal year 2030 to provide payments to qualifying multiemployer plans, as defined in this law, so that the plans can pay benefits at plan levels through the end of plan year 2051. The requested amount will fund the Special Financial Assistance payments to qualifying plans and the Pension Benefit Guaranty Corporation’s related administrative and operating expenses. Neither the plans nor the Pension Benefit Guaranty Corporation are required to repay amounts received under this American Rescue Plan Act of 2021-established program, which is funded by appropriations from the General Fund of the U.S. Treasury.
bFunding provided to the Disaster Relief Fund is generally not specific to individual disasters. Therefore, Treasury’s methodology for determining COVID-19-related obligations and expenditures does not capture obligations and expenditures for the COVID-19 response based on funding other than what was provided in the COVID-19 relief laws. Further, Treasury’s methodology includes all obligations and expenditures based on funding in the COVID-19 relief laws, including those for other disasters. In its Disaster Relief Fund Monthly Report dated May 7, 2024, the Department of Homeland Security reported COVID-19-related obligations totaling $127.4 billion and expenditures totaling $105.3 billion as of April 30, 2024.
cThe Department of Agriculture’s Supplemental Nutrition Assistance Program comprised about $34.0 billion, or 85 percent, of the total expired unobligated balance as of April 30, 2024.
dAmounts shown in columns may not sum to the totals because of rounding.
Lessons from the COVID-19 Pandemic Can Help Federal Agencies Better Prepare for Emergencies
A government-wide approach was needed to respond to and recover from the unprecedented scope and scale of the COVID-19 pandemic. Based on a review of our COVID-19 oversight work, as well as our oversight work on other public health emergencies, we identified lessons learned that federal agencies could use to better prepare for, respond to, and recover from future public health emergencies. These lessons learned highlight areas where government agencies did well in response to the COVID-19 pandemic and areas where the government response could have been improved. We categorized these lessons into seven topic areas. See figure 3. Across these seven areas, federal agencies have opportunities to enhance the nation’s preparedness for future public health emergencies by taking steps to implement recommendations we made in our body of work on COVID-19 oversight.
Planning in Advance
|
|
Lessons Learned on Planning in Advance Advanced plans—including national-level strategies and department- and agency-level plans—provide vision for how the federal government will respond to public health emergencies and are critical to the nation’s preparedness and ability to implement a timely response. To further enhance their preparedness, federal agencies should · clearly define their roles and responsibilities and those of their response partners in response plans, and exercise these plans prior to emergencies; · understand their capabilities and limitations and those of their response partners, and reflect these capabilities and limitations in response plans; and · build their capacity and collect lessons to inform and update plans. We have found instances where federal agencies could improve their preparedness by taking such steps. For example, the Department of the Treasury has not incorporated lessons GAO identified from the COVID-19 assistance programs to the aviation industry into its efforts to compile resources to prepare for future financial disasters. Taking such steps could help Treasury facilitate timely decisions and avoid encountering past challenges when responding to future emergencies. Further, we have made recommendations to federal agencies to improve their emergency response plans. For example, we recommended that the Department of Health and Human Services develop plans outlining steps to mitigate shortages in needed medical supplies, develop a comprehensive testing strategy, and develop an approach for assessing and addressing known challenges and future risks associated with advanced development and manufacturing of medical countermeasures, including vaccines. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
National-level strategies. A whole-of-nation approach is needed to prepare for, respond to, and recover from significant public health emergencies, such as the COVID-19 pandemic. National-level strategies that are developed prior to an emergency can provide vision for and facilitate implementation of a timely response. Further, these strategies inform federal departments’ and agencies’ emergency response plans that guide their response activities. For example, the National Biodefense Strategy provides strategic vision for preparedness and response planning and outlines specific goals and objectives to help the nation prepare for and respond to nationally significant biological incidents.[22] The White House issued an update in October 2022 to the National Biodefense Strategy, which was originally issued in 2018. We have ongoing work to assess this updated strategy and actions to implement it. As part of this work, we will continue to monitor implementation efforts related to the updated strategy.
Our prior work has examined the 2018 National Biodefense Strategy. This strategy included two goals that specifically address preparedness and response actions needed to limit the effects of biological incidents. These goals were meant to inform key federal agencies’—such as HHS and the Department of Homeland Security (DHS)—interagency response and crisis action plans for nationally significant biological incidents, such as response plans to pandemics. However, we have reported gaps in planning for and responding to nationally significant biological events, such as the COVID-19 pandemic. These gaps have limited agencies’ ability to achieve preparedness and response goals outlined in the 2018 National Biodefense Strategy. For example:
· In February 2020, we found that early efforts to implement the strategy represented only the start of a process and a cultural shift that may take years to fully develop, and agencies faced challenges that they must overcome to ensure success in the long term.[23] For example, individual agencies faced a lack of planning and guidance to support the implementation of an enterprise-wide approach to biodefense.[24]
We recommended that HHS take steps to ensure that challenges experienced early during the strategy’s implementation are adequately addressed. As of February 2024, HHS communicated it had taken some steps in collaboration with other federal agencies and departments to address our recommendation; however, HHS no longer has the authority to implement it. According to the updated 2022 National Biodefense Strategy, the White House now leads efforts to implement the strategy. Our ongoing work will continue to monitor implementation efforts related to the updated strategy.
· In August 2021, we identified gaps in the nation’s biodefense enterprise, which limited the federal government’s ability to implement the preparedness and response goals of the National Biodefense Strategy. We recommended that DHS, the Department of Defense (DOD), HHS, and the U.S. Department of Agriculture (USDA) take steps to define a set of capabilities that account for the unique elements specific to responding to nationally significant biological incidents.[25] As of March 2023, these departments had been working with partners to comprehensively review the federal government’s bio-preparedness policies and plans. According to the updated 2022 National Biodefense Strategy, the White House now leads efforts to implement the strategy. Our ongoing work will continue to monitor efforts to implement the updated strategy.
Department- and agency-level response plans. Department- and agency-level response plans that are developed before emergencies occur and are aligned with national strategies can further guide federal efforts when responding to public health emergencies, such as the COVID-19 pandemic. Without such plans, federal and response partners’ actions can be piecemeal and can cause confusion. For example, we found that a comprehensive national plan could help the U.S. aviation system streamline its response to emergencies.[26] We had previously reported that both the federal government and the aviation industry took actions early in the pandemic intended to limit the spread of COVID-19 through air travel. We stated at the time that, while these actions were helpful, some aviation stakeholders highlighted their piecemeal nature, which may have contributed to confusion early in the pandemic.[27]
Early in the COVID-19 pandemic, we urged Congress to require the Department of Transportation (DOT) to develop a national aviation preparedness plan for communicable disease outbreaks. We had previously recommended in 2015 that DOT develop such a plan, but the recommendation remained unaddressed.[28] In June 2020, we emphasized that the absence of a national plan undermined the ability of the public health and aviation sectors to coordinate a response or provide consistent guidance to airports and airlines. We also noted the plan could serve as the basis for testing communication mechanisms among responders and ensure staff have received appropriate training to reduce exposure. Furthermore, we noted that the existence of a national plan might have reduced some of the confusion among aviation stakeholders and passengers early in the pandemic.[29]
In December 2022, legislation was enacted that required DOT to develop an aviation preparedness plan for communicable disease outbreaks.[30] In April 2024, officials within DOT’s Federal Aviation Administration told us that they are drafting such a plan. As part of this process, officials are coordinating internally within the administration; with other federal agencies, including DHS and HHS; and international stakeholders. Once that is complete, coordination will begin with other external stakeholders, including airlines, airports, and labor organizations, according to the Federal Aviation Administration. Officials anticipated finalizing the plan by the end of December 2024.
DOT officials told us previously that they have used lessons learned from the COVID-19 pandemic, as well as from the Ebola, SARS, and other communicable disease outbreaks, to inform the draft plan. Finalizing the forthcoming plan, including incorporating lessons learned from the COVID-19 pandemic, will better position DOT and other aviation stakeholders to address a communicable disease threat while minimizing unnecessary aviation disruptions.
In addition to creating response plans, federal agencies should have a coordinated, department-wide approach to identify and resolve challenges encountered while implementing response plans during past emergencies. Without such an approach, agencies are susceptible to repeating past mistakes. For example, in April 2024 we reported that only three of the six HHS component agencies that are involved in public health emergency responses—the Administration for Strategic Preparedness and Response (ASPR), CDC, and the Food and Drug Administration (FDA)—carry out their own after-action programs to identify challenges from past public health emergencies.[31]
Further, we reported that coordination among the existing after-action programs and with other component agencies was rare. Without creating a department-wide after-action program, HHS is missing an opportunity to improve its preparedness. To strengthen HHS’s ability to respond to future emergencies, we recommended that HHS develop and implement a department-wide after-action program that encourages collaboration across HHS component agencies and includes relevant external stakeholders.[32] HHS concurred with our recommendations. Further, HHS stated it is taking steps to address our recommendations by designating ASPR as the lead to ensure swift identification and resolution of lessons learned from public health emergencies through a centralized after-action review process that will include relevant stakeholders.
Agencies should take steps to further enhance their preparedness for future emergencies, including:
· clearly defining roles and responsibilities for all parties involved with implementing response plans and exercising those plans prior to emergencies,
· understanding their and their partners’ capabilities and limitations, and
· building capacity while also collecting lessons to inform and update plans.
Clearly defining roles and responsibilities. The scope and scale of the COVID-19 pandemic highlighted the critical importance of clearly defining the roles and responsibilities for the wide range of federal agencies and other key partners involved when preparing for pandemics and addressing unforeseen emergencies. A lack of clear roles and responsibilities when preparing for an emergency has hampered the federal response in the past. We have reported that a lack of clear roles and responsibilities has been a recurring challenge in HHS’s efforts to respond to the COVID-19 pandemic and other public health emergencies. For example:
· In April 2021, we reported that HHS did not clarify which HHS agency was in charge—including which HHS agency was responsible for managing infection prevention—when it helped repatriate U.S. citizens from abroad and quarantined them domestically at the beginning of the COVID-19 pandemic to prevent the spread of the virus. As a result, confusion ensued, and HHS put repatriates, its own personnel, and nearby communities at risk.[33]
· In April 2024, we reported similar concerns related to HHS’s initial response to the mpox outbreak, which was declared a public health emergency in the U.S. in August 2022.[34] The initial federal response was spread across multiple HHS agencies. Several state and local jurisdictions we interviewed said that HHS appeared to lack a central point of coordination in the beginning, potentially slowing the response. Additionally, in May 2024, we reported that there was confusion at state, local, and territorial levels regarding how to request and receive mpox supplies from the Strategic National Stockpile. This occurred because HHS agencies involved with the stockpile had not clearly defined roles and responsibilities, thereby complicating response efforts.[35]
We have recommended that HHS take steps to clarify agency roles and responsibilities to limit confusion and risks when responding to public health emergencies. For example, we recommended that HHS revise or develop new emergency repatriation response plans that clarify agency roles and responsibilities, including which agency would be responsible for evacuation and quarantine, during a pandemic.[36]
In response, HHS started a series of workgroup meetings with relevant stakeholders to develop a Federal Emergency Repatriation Operations Plan, among other documents. As of April 2024, HHS had drafted this plan and anticipated finalizing it in early summer 2024. To close this recommendation, HHS and its component agencies will have to demonstrate that they have agreed upon a plan that outlines agency roles and responsibilities, including those for an evacuation and quarantine, in the event of a pandemic.
We also recommended that HHS exercise repatriation response plans before a public health emergency to test the plans and update relevant plans based on lessons learned.[37] Regularly exercising preparedness plans with all response partners allows all involved parties to practice operationalizing the plans. Further, regularly exercising plans can help identify any gaps in procedures or barriers to plan implementation, including a lack of clarity around roles and responsibilities, so that they can be addressed before an actual event occurs.
In response to our recommendation, HHS has conducted two repatriation exercises. While these are positive steps, we have also previously stated that we are monitoring for HHS to conduct exercises with all relevant stakeholders, including other federal agencies, based on agreed upon repatriation plans in response to a pandemic. As noted above, HHS is working to finalize its Federal Emergency Repatriation Operations Plan, among other documents. To close this recommendation, HHS and its component agencies will need to conduct exercises with all relevant stakeholders based on agreed upon guidance that outlines agency roles and responsibilities in response to a pandemic.
Understanding agencies’ and response partners’ capabilities and limitations. It is important for federal agencies to understand their and their response partners’ capabilities and limitations, and that these capabilities and limitations are reflected in federal response plans. ASPR, the agency within HHS responsible for leading and coordinating all matters related to federal public health and medical preparedness, relies, in part, on partners to respond to emergencies. However, our prior work has shown that ASPR did not have a complete understanding of the capabilities and limitations of response partners, which created a vulnerability. For example, in September 2019 we reported that the agency did not have a full understanding of the capabilities and limitations of its support agencies, including DOD, DHS, and the Department of Veterans Affairs (VA), during the response to the catastrophic destruction in the U.S. Virgin Islands and Puerto Rico caused by Hurricanes Maria and Irma in 2017. Consequently, ASPR’s needs were not always aligned with the resources that its support agencies could provide, resulting in some deployed resources not being properly and efficiently utilized.[38]
We have also identified concerns with ASPR’s capabilities to fully execute its preparedness and emergency response activities, particularly as these responsibilities have increased. ASPR’s additional responsibilities include managing the Strategic National Stockpile and leading the medical product industrial base expansion effort to help establish a more resilient medical product supply chain for the nation. This was an area of concern during the COVID-19 pandemic and remains a concern.
Further, as we reported in January 2024, ASPR had not identified critical areas within it that needed workforce assessments or developed a plan to conduct them. It also had not conducted an agency-wide workforce assessment to prioritize the skills and competencies of greatest need to achieve the agency’s goals and mission.[39] Without conducting these assessments, ASPR cannot be assured that its workforce has the skills and competencies in place to perform its responsibilities and ultimately meet its mission of leading the nation’s response to public health emergencies.
To improve its capabilities to fully execute emergency response activities, we recommended that ASPR establish specific goals and performance measures to use for its new hiring office, identify the critical areas that need workforce assessments, develop plans to implement them, and conduct an agency-wide workforce assessment. HHS neither agreed nor disagreed with two of our recommendations and agreed with the other two recommendations. In its comments, HHS discussed plans to support workforce assessment efforts, among other steps to address our recommendations.
Building capacity and collecting lessons to inform plans. Building capacity, collecting lessons from prior emergencies, and using this information to inform response programs and plans can improve federal agencies’ preparedness for future public health and other emergencies.
For example, the Veterans Health Administration (VHA) would be better prepared to quickly estimate resource needs to allow better management and planning by enhancing its modeling capacity. VHA requested supplemental funding to continue operations to meet its mission when the COVID-19 pandemic emerged in 2020 but was not prepared to estimate the amount of supplemental funding needed during such a catastrophic event.
In February 2024, we reported that the agency did not have the modeling capacity to enable it to prepare estimates of the supplemental funding it needed in the event of another pandemic or other catastrophic event. Specifically, VHA lacked modeling capacity, including data collection and the ability to run budget simulations on a continual basis, to systematically assess and manage the risk of catastrophic events.[40] We recommended that the VA Undersecretary for Health should enhance VA’s analytical modeling capacity to better enable VHA to prepare estimates of supplemental funding needed to address catastrophic events. VHA concurred with our recommendation and outlined actions to address it, including chartering a workgroup to evaluate appropriate models and estimate required resources needed in the event of specific catastrophic events, such as a pandemic.
Federal agencies can also better prepare for future emergencies by leveraging lessons learned and incorporating them into response programs and plans. For example:
· Federal agencies can leverage economic lessons from SBA’s Paycheck Protection Program to inform support programs for smaller businesses affected by emergencies. We previously reported that studies have shown that the Paycheck Protection Program increased employment in small businesses, generally improved their financial conditions, and likely strengthened local labor markets. However, we found that some portion of the program assistance did not initially go to areas hit hardest by the pandemic and that smaller businesses faced challenges obtaining program assistance, which may have limited the effect of the program.[41]
In response to such concerns, Congress and SBA made a series of changes that increased lending to businesses that faced challenges obtaining loans, such as targeting minority-owned businesses, in later phases of the program’s implementation. By considering relevant economic conditions and accounting for the unique needs of smaller businesses, agencies could better target relief programs to the hardest hit areas and improve accessibility to federal funds for smaller businesses during emergencies.
· Federal agencies can better prepare for future emergencies by collecting and sharing lessons learned from contracting in response to the COVID-19 pandemic. However, HHS and DHS, two of the top five agencies with the highest COVID-19 contract obligations as of August 31, 2020, did not include lessons learned as part of their COVID-19 response review even though they identified contracting challenges. Establishing mechanisms to formally collect and share lessons learned from stakeholders involved with contracting will help ensure agencies can apply lessons learned and positive processes in response plans for future emergencies.[42] DHS has since taken action to establish mechanisms to collect and share contracting lessons learned from future response efforts. As of April 2024, HHS has ongoing efforts to collect and share such lessons learned.
· HHS can be better prepared to meet the nations’ need for medical countermeasures during emergencies and when responding to threats of widespread illness posed by emerging infectious diseases, including new COVID-19 variants, by incorporating approaches to address known challenges in new plans and programs. Medical countermeasures are drugs, vaccines, and devices to diagnose, treat, prevent, or mitigate the health effects of exposure to chemical, radiological, nuclear, or biological agents, including viruses. Many factors make it difficult to rapidly develop and manufacture medical countermeasures in response to public health emergencies.
HHS created the Centers for Innovation and Advance Development and Manufacturing (CIADM) program in 2012 in response to challenges in developing countermeasures during prior emergencies. Under this program, HHS awarded funding to three contractors to establish sites to develop countermeasures. HHS used these sites to support the manufacturing of COVID-19 vaccines. However, program limitations, such as sites not receiving consistent funding and production work from HHS or external manufacturing partners, hindered the CIADM program’s effectiveness.
In 2022, HHS announced that it was ending the CIADM program and developing a new program model for rapid countermeasure production intended to replace it. We reported in February 2023 that HHS’s plans for this new program model were not fully developed, and it was unclear as to how the program model will address or mitigate known challenges and future risks. To avoid repeating the challenges of the CIADM program, we recommended that HHS incorporate into the development of its new program model an approach to systematically assess and respond to known challenges and future risks associated with advanced development and manufacturing of medical countermeasures. HHS concurred with our recommendation and stated it will work to ensure its new model program aligns with the principles outlined in our recommendation.[43]
· Treasury could be more prepared for future financial disasters by including lessons learned from COVID-19 financial assistance programs to the aviation industry as part of its efforts to compile resources, specifically policies and procedures from programs it has implemented. Treasury had to quickly design several COVID-19 financial assistance programs, including the $46 billion loan program for aviation and other eligible businesses under Section 4003 of the CARES Act. This effort was challenging as Treasury had to establish program infrastructure, develop credit standards, and draft loan documents in a short time frame and under difficult circumstances.
In December 2020, we reported that although Treasury’s policies and procedures for evaluating loan applications were generally consistent with internal controls, the program could have been improved.[44] In particular, at that time we reported that providing emergency financial assistance through multiple programs or multiple paths within a program may better accommodate businesses of varied types and sizes, and that Treasury should clearly communicate timelines for actions to align lender and borrower expectations, among other things. In addition, our prior work has shown that providing federal assistance to businesses facing emergency circumstances requires clear and consistent information be communicated to applicants and eligible entities.[45]
In May 2023, SIGPR reported on a $700 million loan that Treasury made through the loan program to Yellow Corporation, a trucking company formerly known as YRC Worldwide.[46] While Yellow Corporation was not a part of the aviation industry, the loan program was available to businesses critical to maintaining national security.[47] The SIGPR report found deficiencies in Treasury’s approach to reviewing, approving, and disbursing this loan. Recognizing the need to act quickly while also having policies and procedures in place before executing loans, SIGPR recommended that Treasury develop a contingency plan for financial disasters. Doing so would provide a framework for future direct lending programs and reduce implementation time and the possibility of errors and omissions.
In our prior work, we have emphasized that considering lessons learned can help Congress and Treasury provide financial assistance to businesses in a timely manner, while also ensuring adequate safeguards to minimize the risk to the federal government from a borrower not repaying the loan.[48] We have also identified collecting and sharing information and knowledge gained from positive and negative experiences as a key practice of a lessons learned process.[49]
In April 2024, Treasury officials told us they are compiling resources to prepare for future financial disasters and expect to complete this effort by the end of 2024. Specifically, officials are compiling policies and procedures from the COVID-19 financial assistance programs provided to the aviation industry and lending programs Treasury operated under the Troubled Asset Relief Program.[50] However, in doing so, they have not included lessons we and other auditing entities have identified for emergency financial assistance programs.
Treasury officials told us that they have not endeavored to create a specific plan for financial assistance programs for future crises because each scenario requiring emergency financial assistance is unique. Further, officials told us that Treasury does not have the resources to design plans that would respond to the varied contingencies that may arise. As such, Treasury officials said they are compiling resources that could be useful across sectors and goals for future financial assistance, such as liquidity of funds and employment retention. Including lessons we identified and those identified by other external entities could help Treasury create a broad framework for future financial assistance programs, by not only documenting past procedures but also noting general lessons from implementing the recent assistance programs for the aviation industry. This can help Treasury improve its future relief programs and avoid encountering some of the challenges it faced in the past. Given the need to act quickly in financial disasters, it would be beneficial for Treasury to include lessons learned in this effort to enable decisionmakers to make timely decisions in the future.
Key open recommendations. We have made recommendations to federal agencies to improve their emergency response planning. These included recommendations to HHS to develop plans outlining actions the federal government will take to help mitigate shortages in needed medical supplies; to develop a comprehensive testing strategy to allow for a more coordinated pandemic testing approach; and to systematically assess and respond to known challenges and future risks associated with advanced development and manufacturing of medical countermeasures, such as vaccines.
Agencies across the federal government have taken steps to address some of our recommendations to improve their preparedness for public health emergencies. However, agencies should take additional steps to strengthen their ability to prepare for, respond to, and recover from public health emergencies, including:
· HHS should develop and implement a coordinated, department-wide after‑action program that encourages collaboration among HHS’s component agencies and includes relevant stakeholders involved in each public health response.
· HHS’s ASPR should establish specific goals and performance measures to use for its new hiring office, identify the critical areas that need workforce assessments, develop plans to implement them, and conduct an agency-wide workforce assessment.
· HHS should update emergency repatriation response plans that clarify agency roles and responsibilities, including those for an evacuation and quarantine, during a pandemic. Further, HHS should conduct regular exercises with relevant stakeholders to test plans in response to a pandemic and update them based on lessons learned.
Collaborating with Response Partners
|
|
Lessons Learned on Collaborating with Response Partners Collaborating with response partners—including federal and nonfederal partners—before and during public health emergencies can help agencies efficiently implement response activities and continue operations. To help facilitate this collaboration, federal agencies should · identify partners key to implementing the response and regularly coordinate with them throughout the response, and · ensure their response partners understand their respective roles and related responsibilities in implementing the response. We have made recommendations to federal agencies to improve their coordination with response partners before and during public health emergencies. For example, we recommended that the Department of Health and Human Services share its plans to mitigate shortages in medical supplies with response partners and maintain up-to-date guidance for partners on requesting and receiving assets from the Strategic National Stockpile. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
Identifying and coordinating with partners. Federal agencies can enhance the response to a public health emergency by identifying relevant federal and nonfederal partners and regularly coordinating with them. Public health emergencies may result in wide-ranging challenges that no single agency can address. This requires federal agencies to collaborate with one another and with other partners—such as Tribes, states, U.S. territories, localities, and the private sector—to implement response activities. Our work has highlighted instances during the COVID-19 pandemic where federal agencies and private entities successfully collaborated to achieve response goals, including developing and administering vaccines. For example:
· In January 2022, we reported that collaboration between federal agencies and private sector partners enhanced activities to quickly develop and manufacture COVID-19 vaccines for the public.[51] To help make safe and effective vaccines available as quickly as possible, the federal government announced the creation of a partnership between HHS and DOD in April 2020, which began as Operation Warp Speed and later became the HHS-DOD COVID-19 Countermeasures Acceleration Group. HHS and DOD then made awards to vaccine companies and others to help them make vaccines available.
We found that by making awards to multiple vaccine companies, the agencies mitigated risks to meeting their vaccine goals. For instance, working with multiple companies reduced the risk of failure due to safety, efficacy, or manufacturing issues. We also found that the coordination between agencies and vaccine companies helped alleviate supply chain issues. For instance, HHS and DOD utilized the Defense Production Act to support manufacturing efforts by providing priority access to necessary materials.[52]
· In July 2021, we reported CDC’s coordination with the private sector played a critical role in administering COVID-19 vaccines in nursing homes and other long-term care facilities. CDC established the Pharmacy Partnership for Long-Term Care Program, an agreement with pharmacy partners to conduct COVID-19 vaccination clinics for residents and staff of long-term care facilities, including nursing homes, in October 2020. As part of the program, vaccines were provided at no cost to residents, staff, and the facilities.
Additionally, the pharmacy partners—including CVS, Walgreens, and Managed Health Care Associates Inc.—managed the entire vaccination process at certain facilities. This included storing, handling, and transporting vaccines; administering vaccines; and fulfilling reporting requirements. We reported in March 2021 that many of the vaccinations in nursing homes and other long-term care facilities were administered through these partnerships.[53] Between December 2020 and May 2021, the partnership program administered more than 8.3 million doses of COVID-19 vaccines, according to CDC.[54]
During the COVID-19 pandemic, we found instances where federal agencies did not regularly coordinate with response partners, and important opportunities to enhance response outcomes were missed. For example:
· In September 2020, we found that the Federal Emergency Management Agency (FEMA) could enhance its efforts to distribute COVID-19 supplies—including personal protective equipment, ventilators, and COVID-19 testing supplies—by coordinating with its response partners.[55] During the pandemic, FEMA was responsible for distributing these supplies to its response partners, including tribal, state, local, and territorial governments.
To help it make decisions on how supplies would be allocated throughout the pandemic, FEMA reviewed supply requests submitted by its partners. However, we reported that FEMA’s response partners faced challenges tracking the agency’s fulfillment of supply requests, which made it difficult for them to then determine what additional supply requests they needed to make. For example, an official from one state told us that they were not told when supplies would arrive, and shipments would “just show up” without advance notice. Another state official said that the FEMA regional office did not always specify where the supplies went or to whom they were delivered.
We recommended that FEMA work with its partners on solutions to help states enhance their ability to track the status of supply requests and plan for supply needs for the remainder of the pandemic response. Although the agency disagreed with our recommendation, it took several actions that addressed it. For instance, in 2022, FEMA released an updated distribution management plan guide that, according to FEMA, provided actionable guidance for tribal, state, local, and territorial agencies to effectively and efficiently distribute critical resources in the community.
· In May 2024, we reported that additional coordination with Tribes would help the federal government better prepare for future emergencies that may require Strategic National Stockpile assets.[56] HHS documentation and our interviews with selected Tribes and tribal organizations revealed various concerns Tribes had with requesting and receiving stockpile assets during recent emergencies, including the COVID-19 pandemic and the mpox public health emergency. These concerns included Tribes’ issues with receiving assets due, in part, to infrastructure or geography. For example, officials from one Tribe as well as a former official from another Tribe reported challenges with having the equipment and infrastructure needed to receive and store delivered assets.
While ASPR has made progress in defining pathways for how Tribes can request Strategic National Stockpile assets, it has not assessed how it will address unique tribal challenges related to receiving assets. Engaging with Tribes to assess these issues could help HHS and Tribes be better equipped to deliver and receive assets respectively, and they can collectively strengthen preparedness and response efforts for future incidents. We recommended that ASPR formally designate an entity to regularly engage with Tribes and relevant stakeholders to (1) assess the unique challenges, such as infrastructure and geography, that could affect the delivery of assets in the Strategic National Stockpile to Tribes during future emergencies and (2) develop options for how to address those challenges. The agency agreed with our recommendation.
Coordination between federal and nonfederal partners could also help federal agencies address challenges adopting vaccine development technologies and approaches that may enhance the nation’s ability to respond to infectious diseases. While vaccinations are a key part of individual and community health, vaccine development is complex and costly. In November 2021, we reported that innovative technologies and approaches may enhance the nation’s ability to respond to infectious diseases. For example, reverse vaccinology using computer-based analytics to assess a pathogen’s genetic information to accelerate the understanding of pathogens and their antigens—combined with existing research—helped researchers develop some COVID-19 vaccines more quickly and effectively.
However, key challenges may hinder the adoption of these innovative technologies and approaches. We identified nine policy options for policymakers, including federal agencies, to help address these challenges and economic challenges. For example, policymakers have opportunities to improve preparedness by supporting public-private partnerships that would help identify and respond to disease pathogens with pandemic potential.[57]
Communicating roles and responsibilities to response partners. To effectively coordinate with response partners during a public health emergency, federal agencies should ensure that response partners understand their respective roles and related responsibilities in implementing the response. Federal agencies should ideally define the roles and responsibilities of their partners in response plans and communicate these prior to an emergency. When roles are not established in advance of an emergency, federal agencies should do this early in the response. Our work during the COVID-19 pandemic indicated that when the roles and responsibilities of response partners are not clearly defined and communicated, agencies cannot be assured that their partners take timely actions needed to implement response activities. For example:
· In April 2021, we found that DOD’s depot management did not consistently take actions to ensure continued operations during the COVID-19 pandemic because depot personnel lacked clear guidance from DOD on their roles and responsibilities.[58] Long-term disruptive events like pandemics can diminish military readiness if personnel who repair and maintain complex weapon systems and equipment at DOD’s depots are physically away from the workplace for weeks or months.[59]
DOD issued a memorandum on March 20, 2020, notifying the Defense Industrial Base, which includes DOD depots, that they were identified as a critical infrastructure sector and had a special responsibility to maintain their normal work schedule.[60] However, DOD had not developed guidance or a communication plan to ensure that depot management and personnel were aware of their mission-essential status and the need to support readiness. Further, we reported that the roles and responsibilities of depot personnel as mission-essential personnel were not always clear to depot leadership and personnel. As a result, depot management improvised their operation plans, causing some depots to pause or reduce operations, and others to shift schedules rather than maintaining normal work schedules.
We made two recommendations that DOD take steps to ensure that its depot management and personnel are made aware of their mission-essential status and the need to support readiness during a long-term crisis affecting the depot workforce. DOD concurred with our recommendations and addressed them through various actions, such as establishing a website to communicate guidance to DOD personnel, including depot staff, and publishing a plan detailing the steps it will take to communicate mission-essential status during a pandemic.[61]
· In May 2024, we reported that ASPR could enhance the response to public health emergencies by addressing challenges jurisdictions identified regarding coordination with the federal government around Strategic National Stockpile assets during the COVID-19 pandemic and the mpox public health emergency.[62] We found that jurisdictions lacked up-to-date information from federal agencies on their roles and current processes for requesting and receiving stockpile assets, resulting in confusion among jurisdictions during recent public health emergency responses.
Specifically, there is no formal documented agreement between ASPR and CDC that details each agency’s roles and responsibilities related to stockpile operations, according to Strategic National Stockpile officials. Further, we found ASPR lacked standard operating procedures for updating key guidance based on the most current information. For example, the main guidance for requesting and managing stockpile assets was last updated in 2014.
We recommended that ASPR should work with CDC to clearly define its and CDC’s roles and responsibilities related to the Strategic National Stockpile in a formal document and share that document with jurisdictions. Additionally, we recommended that ASPR develop standard operating procedures outlining how and when guidance documents, such as those for requesting and receiving Strategic National Stockpile assets, are updated. If ASPR develops these standard operating procedures, jurisdictions will be more likely to have access to updated guidance that reflects current processes and, in turn, improve response efforts.
Key open recommendations. We have made recommendations to federal agencies to improve their coordination with response partners before and during public health emergencies. These included recommendations for HHS to provide response partners with the agency’s plans to mitigate shortages in needed medical supplies, and to ensure it maintains up-to-date guidance for response partners on the processes for requesting and receiving vaccines and other assets from the Strategic National Stockpile.
Agencies across the federal government have taken steps to address some of our recommendations to enhance collaboration between federal and nonfederal partners. Yet, agencies could further improve their ability to efficiently implement response activities by taking additional actions to address other recommendations that remain open, including:
· ASPR should develop standard operating procedures outlining how and when guidance documents, including guidance on requesting and receiving assets from the Strategic National Stockpile, are updated. ASPR should also formally designate an entity to regularly engage with Tribes and relevant stakeholders to assess the unique challenges that could affect the delivery of assets from the Strategic National Stockpile to Tribes during future emergencies and to develop options for how to address those challenges.
· SBA should—in coordination with FEMA and the Department of Housing and Urban Development and with input from key recovery partners—develop and implement an interagency plan to help ensure the availability and use of quality information to support federal agencies involved in disaster recovery in identifying access barriers or disparate outcomes.
Providing Clear and Timely Communications
|
|
Lessons Learned on Providing Clear and Timely Communications Federal agencies can enhance their efforts to effectively administer relief funds, vaccines, and other critical resources during a public health emergency by providing clear and timely information to the · applicants and eligible entities of federal relief funds, · recipients of federal relief funds, and · the public. We have made recommendations to federal agencies to improve their communication during public health emergencies. For example, we recommended that the Small Business Administration develop a comprehensive strategy for communicating with potential and actual program applicants in the event of a disaster, and that its strategy should include guidelines for the types of information and timing of information to be provided to program participants throughout a disaster. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
Communications to relief fund applicants and eligible entities. Federal agencies can better ensure that eligible entities have the information they need to seek federal assistance by communicating clear, timely information on federal relief programs, such as program goals, eligibility requirements, and funding time frames. This is especially true when the federal funds are provided through new or expanded programs, as applicants may not have prior experience navigating federal financial assistance programs. However, we found that federal agencies did not always provide clear and timely information to applicants and eligible entities of COVID-19 relief fund programs and recommended that agencies take action to strengthen their communications.
Our body of work on COVID-19 financial assistance programs for the aviation industry showed that federal agencies’ communication with airports and other applicants and eligible entities was inconsistent. The COVID-19 pandemic caused an unprecedented and sudden drop in demand for U.S. passenger airlines. Three COVID-19 relief laws enacted in 2020 and 2021 made $132 billion in assistance available to airlines, aviation and other businesses, and airports across four selected programs—Treasury’s Payroll Support Program and CARES Act loan program and DOT’s Airport Grants Program and Aviation Manufacturing Jobs Protection Program.
· For the Payroll Support Program and CARES Act loan program, we found that Treasury did not communicate eligibility requirements and time frames clearly to applicants. For instance, according to our September 2020 report, industry associations including those representing regional and small aviation companies reported that a lack of clear information on program eligibility and other requirements contributed to challenges navigating the Payroll Support Program application.[63] Similarly, in December 2020, we reported that, for the CARES Act loan program, Treasury did not communicate a time frame for evaluating applications and making loans.[64] As a result, businesses were unsure when Treasury would execute loans, which complicated their decision-making while awaiting loan decisions, according to industry associations and applicants.[65]
According to Treasury officials, the emergency nature of the programs and emphasis on quickly distributing funds limited the amount of time Treasury had to conduct the outreach it typically does when implementing new programs. Previously, we reported that the government should ensure adequate transparency by establishing an effective communication strategy, which could include sharing timelines, to help ensure an understanding of the matters at hand.[66] Ensuring such transparency creates additional tasks for an agency busy establishing a new program. Yet, investing time in such tasks could help avoid problems caused by a lack of communication, such as confusion about the motivations behind program actions and decisions.
· We found that program applicants were more complimentary of DOT’s communication regarding the Airport Grants Program and Aviation Manufacturing Jobs Protection Program. In November 2020, we reported that, for the Airports Grants Program, DOT generally provided timely guidance and assistance to applicants, according to selected airport sponsors and airport association representatives that we spoke with.[67] Further, in October 2021 we reported that industry associations were generally complimentary of DOT’s communication regarding the Aviation Manufacturing Jobs Protection Program, although some industry associations expressed challenges with the clarity of some DOT guidance.[68]
Communications to relief fund recipients. After relief funds have been awarded, federal agencies should continue to provide clear and timely information to help program recipients effectively manage their awards. For instance, agencies should communicate information on topics such as allowable uses of funds, time frames for using funds, and reporting requirements. This information can be provided through guidance or in responses to inquiries from recipients.
In our December 2023 report, we found that Treasury took steps to help state and local recipients manage their COVID-19 relief funds, but further actions could help ensure more timely and helpful assistance.[69] In April 2021, Treasury established the Contact Center to respond to inquiries about programs that it administered, including the Coronavirus State and Local Fiscal Recovery Funds (SLFRF).[70]
However, state and local officials identified a lack of timely and helpful assistance from the Contact Center as a challenge to managing these funds. For example, officials in five of 18 selected states we met with told us that, in some instances, they either received no response from Treasury to a question or received a response to a time-sensitive question after a deadline had elapsed. Treasury officials told us that limited funding available to administer the SLFRF had affected their ability to assist recipients through the Contact Center.[71]
Treasury officials also told us that responding to IT- or SLFRF policy-related questions can result in longer Contact Center response times.[72] This is because the questions were more complex and needed to be referred to staff in other Treasury offices, such as those who manage and administer the SLFRF program. Further, we found that Treasury had assessed the number of staff it needed in its Contact Center, but not the staffing needs in other offices the Contact Center relied on to address IT- or SLFRF policy-related questions. Without a comprehensive assessment of staffing needs, Treasury’s Contact Center was less able to provide the timely and helpful information that states and localities needed to effectively manage their awards. To improve communications, we recommended that Treasury comprehensively assess staffing needs for the Contact Center to ensure that it is able to respond timely to SLFRF recipients’ requests for assistance and with information that meets their needs. Treasury agreed with our recommendation and told us it has begun such an assessment.
Communications to the public. Agencies need to provide clear and timely information to the public because the public’s participation is critical to implementing an effective federal response. We previously reported that administering vaccines to individuals was a key component of the federal response to mitigate the effect of the COVID-19 pandemic on the public’s health. Our work examining federal agency vaccination efforts during the pandemic has highlighted the critical importance of providing clear and timely information to the public to support vaccine use. For example:
· In September 2020, we reported that clarity on the federal government’s plans for distributing and administering vaccine, as well as timely, clear, and consistent communication to stakeholders and the public about those plans, was essential. Representatives of state, local, and territorial health officials, and health care providers we interviewed emphasized the need for the federal government to develop and share plans for the distribution and administration of COVID-19 vaccines before one becomes available.[73]
At that time, we recommended that HHS, with the support of DOD, establish a time frame for documenting and sharing a national plan for distributing and administering COVID-19 vaccines. Further, such a plan should be consistent with best practices for project planning and scheduling, and it should outline an approach for how efforts will be coordinated across federal agencies and nonfederal entities. Due to widespread distribution and administration of COVID-19 vaccines, the time frame for implementation of this recommendation has passed.
However, our past work and the work of others have demonstrated that proper planning—including incorporating best practices for project planning and scheduling and sharing information with stakeholders in a timely manner—is critical to the success of distributing and administering any licensed or authorized vaccine. Thus, we continue to believe it is important for agencies to develop and communicate, including with the public, vaccine distribution plans when implementing the response to future emergencies.
· We found that a lack of clear and timely information from federal agencies contributed to challenges managing public expectations. In January 2021, we reported that early vaccine distribution efforts did not match public expectations, with initial numbers of distributed vaccines falling short of expectations set by HHS and DOD’s Operation Warp Speed partnership.[74] Additionally, we have reported that a lack of clear and timely guidance from agencies on which populations should be prioritized for initial doses made it challenging for health officials and health care providers to manage the public’s expectations about when individuals could get vaccinated.[75] As we found in our prior work examining the federal response to the H1N1 pandemic, the failure to manage public expectations can undermine government credibility and the public’s participation in vaccination efforts.[76]
· In April 2021, we reported that health care providers lacked authoritative, science-based information to combat misinformation and vaccine hesitancy.[77] In our November 2021 report, selected stakeholders told us that while CDC’s education materials helped state and local health officials and health care providers address the public’s concerns about the safety of COVID-19 vaccines, these materials would have been more useful had CDC released them earlier.[78]
· Engaging communities as part of a vaccine communication strategy can help agencies combat factors that decrease receptivity to government response efforts. In our September 2023 report, we found that the U.S. Agency for International Development played a role in vaccinating the world against COVID-19, spending nearly $1 billion to assist 125 countries with their vaccination efforts.[79] To help achieve its goal of vaccinating 70 percent of the population in each country, the agency supported various efforts to combat factors that had decreased vaccine demand. These efforts included a communication strategy for addressing issues related to disinformation and perceived low risk of infection, and working with community leaders and other influential community members, such as well-known athletes and musicians, to generate demand.
Key open recommendations. Our work has highlighted the need for federal agencies to provide clear and timely information to the public to effectively administer relief funds, vaccines, and other critical resources. We have made recommendations to federal agencies to improve the clarity and timeliness of communications around relief program goals and requirements and plans for distributing vaccines during the COVID-19 pandemic.
Agencies have taken steps to address some of our recommendations. Taking additional steps to implement our recommendations that remain open could facilitate federal agencies’ continued efforts to provide support to those affected by the COVID-19 pandemic and improve their response to future public health emergencies. For example:
· Treasury should comprehensively assess staffing needs for the Contact Center to ensure that it is able to provide timely and helpful assistance to recipients of SLFRF awards. Further, Treasury should update and implement the agency’s documented policies and procedures for monitoring recipients’ use of SLFRF awards to reflect lessons learned from reviewing recipients’ project and expenditure reports.
· SBA should develop a comprehensive strategy for communicating with potential and actual program applicants in the event of a disaster. Such a strategy should provide guidelines for the types of information and timing of information to be provided to program participants throughout a disaster. The types of information to be addressed in the strategy could include processing steps and time frames applicants might experience through different stages of the loan process.
Managing Program Integrity Risks
|
|
Lessons Learned on Managing Program Integrity Risks Establishing controls and processes to mitigate and address financial risks can help federal agencies reduce the likelihood of improper payments and fraud when they must disburse emergency relief funds quickly during a public health emergency. · Prepayment controls and processes can help agencies minimize the likelihood of improper payments and fraud. · Postpayment controls and processes can help agencies identify and recover improper and fraudulent payments when the quick disbursement of funds makes prepayments controls difficult to apply fully. We have made recommendations to federal agencies to better manage program integrity risks in emergency assistance programs. For example, we recommended that the Department of Labor design and implement an antifraud strategy for unemployment insurance programs that is consistent with leading practices for preventing, detecting, and responding to fraud outlined in GAO’s Fraud Risk Framework. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
During a public health emergency, it is important that federal agencies get relief funds out quickly to those affected by the emergency while ensuring appropriate controls and processes are in place to reduce the likelihood of improper payments and fraud. Improper payments and fraud are two distinct concepts that are related but not interchangeable. While all fraudulent payments are considered improper, not all improper payments are due to fraud. For example, improper payments can be overpayments or underpayments that result from error or a lack of agency oversight.[80] Fraudulent payments are different from other types of improper payments because they generally involve individuals or entities intentionally or knowingly providing false information, such as incorrect eligibility or identity information, to receive a benefit from the federal government.[81]
While the full extent of fraud associated with COVID-19 relief funds will never be known with certainty, estimated fraud in certain relief fund programs is in the hundreds of billions. For example, in September 2023, we estimated the amount of fraud in DOL’s unemployment insurance programs during the pandemic—from April 2020 through May 2023—was likely between $100 billion and $135 billion.[82] Further, SBA’s Office of Inspector General estimated that, as of June 2023, SBA had disbursed over $200 billion in potentially fraudulent pandemic relief loans, which is approximately 17 percent of SBA’s total COVID-19 spending.[83]
In April 2024, GAO estimated total direct annual financial losses to the government from fraud to be between $233 billion and $521 billion, based on data from fiscal years 2018 through 2022.[84] The data include time periods and programs with and without pandemic-related spending. Therefore, the estimate includes, but is not limited to, pandemic-related spending fraud. While the upper range of the estimate is associated with higher-risk environments like the pandemic, it is not possible to break out a subset of our government-wide estimate to describe pandemic program fraud.
We further reported that the COVID-19 pandemic is a recent example of how factors such as the effectiveness of federal fraud risk management and the nature of new fraud threats can substantially impact the scale of fraud. We have previously reported on the heightened fraud risk environment associated with some pandemic programs.[85] These prior reviews provided observations about varying fraud risk environments by program and across delivery years, as well as the standalone estimate of unemployment insurance fraud during the pandemic.
Additionally, the Department of Justice has brought federal fraud-related charges against individuals or entities in cases involving federal COVID-19 relief programs. We analyzed the department’s public statements and court documentation and found, from March 2020 through March 2024, at least 1,998 individuals or entities facing charges were found guilty or liable.[86] This includes fraud-related charges in cases involving SBA’s small business programs, DOL’s unemployment insurance programs, and Treasury’s economic impact payments, among other programs. Of the individuals found guilty, at least 1,596 had been sentenced as of March 31, 2024, and many have also been ordered to pay restitution and fines.[87]
There were also federal fraud-related charges pending against at least 632 other individuals or entities involving federal COVID-19 relief programs, as of March 31, 2024.[88] The number of individuals or entities facing fraud-related charges from COVID-19 relief programs will likely continue to increase, as these cases take time to develop, and the statute of limitations has been extended to 10 years to prosecute individuals who committed fraud related to the Paycheck Protection Program and the COVID-19 Economic Injury Disaster Loan program. Additionally, there are ongoing legislative efforts in Congress to extend the statute of limitations for various other programs. For example, DOL’s Inspector General has requested that Congress extend the statute of limitations for fraud for the pandemic relief Unemployment Insurance programs.[89]
By applying the leading practices identified in GAO’s Framework for Managing Improper Payments in Emergency Assistance Programs and Framework for Managing Fraud Risks in Federal Programs, agencies can better plan for and take a more strategic approach toward managing improper payments and fraud when implementing the federal response to future public health emergencies.[90] These frameworks instruct agencies to implement internal controls and leading practices that can help them prevent, detect, and recover improper and fraudulent payments.
The need—and requirements—for agencies to take action to address fraud was reiterated in our February 2023 testimony, which identified agencies’ continued lag in implementing fraud risk management activities as a major factor contributing to pandemic programs’ exposure to fraud.[91] In addition, we have suggested that Congress take legislative actions to help address agencies’ shortcomings in their applications of fundamental internal controls and fraud risk management practices. See appendix I for additional information on these legislative actions.
Prepayment controls. When administering federal emergency relief fund programs, federal agencies can implement prepayment controls and processes at the beginning of the program or as soon as possible after program implementation to help prevent improper payments and fraud. We previously reported that agencies did not have appropriate internal controls to prevent, detect, and recover improper and fraudulent payments when administering some COVID-19 relief programs.[92] We also found instances where some agencies that lacked appropriate internal controls at the start of the pandemic strengthened those controls as the programs matured.
For example, SBA quickly set up its pandemic relief programs to rapidly respond to the adverse economic conditions small businesses faced. However, this was done at the expense of appropriate financial and other safeguards, which left SBA’s programs susceptible to improper payments and fraud. Our work examining SBA’s small business programs—particularly the Paycheck Protection Program and the COVID-19 Economic Injury Disaster Loan program—identified funds provided to ineligible businesses and to legitimate business owners who falsely self-certified their eligibility, among other things.
Other fraud controls to mitigate these misrepresentations were either not in place or were not effective. We reported in March 2024 that, as the programs matured and SBA implemented our recommendations, SBA improved its oversight and incorporated lessons learned from the Paycheck Protection Program and the COVID-19 Economic Injury Disaster Loan program into its other relief programs.[93] We estimated that, as of the end of fiscal year 2023, SBA’s use of additional safeguards in the Paycheck Protection Program and other COVID-19 programs had resulted in more than $12 billion in savings.
We also reported that, by examining fraud schemes that emerged during the COVID-19 pandemic, agencies can identify controls that can be implemented to mitigate fraud risks when administering relief programs in response to future emergencies.[94] For example, the COVID-19 pandemic saw an increase in the frequency and volume of identity-related fraud, particularly in the areas of unemployment insurance and small business relief programs.[95] These developments will likely continue to challenge future federal emergency assistance efforts. Therefore, agencies can assume applicant identity information will be compromised and should implement prepayment controls to verify applicant identity when implementing relief programs in response to future emergencies.[96]
Postpayment controls. Agencies should prioritize prepayment controls and avoid relying on the “pay and chase model,” which refers to the practice of waiting to address improper payments and fraud until after payments have been made. However, establishing postpayment controls and processes can help agencies identify and recover improper payments and fraudulent payments when the quick disbursement of funds makes prepayment controls difficult to apply fully. Agencies should act promptly to recover payments—the more time passes, the less likely payments will be recovered.
Accordingly, agencies should establish processes to identify and recover improper and fraudulent payments when they begin administering federal relief fund programs or as soon as possible after program implementation. However, we found that many agencies that administered COVID-19 relief programs lacked controls and processes that would have helped them promptly identify and recover improper and fraudulent payments. For example:
· In September 2022, we reported that limitations in USDA’s process for reviewing payments made through the Coronavirus Food Assistance Program may have undermined USDA’s ability to detect improper payments.[97] In 2020 and 2021, USDA’s Farm Service Agency provided $31 billion in aid to 965,651 producers of agricultural commodities—including crops, dairy, and livestock—through the program to offset losses and increased costs associated with the COVID-19 pandemic. These payments were made based on self-certified claims but were subject to the agency’s postpayment reviews, including spot checks to review producers’ claims and supporting materials.
However, we identified several limitations that may have undermined the agency’s ability to identify improper payments using its spot check reviews. These limitations included the Farm Service Agency’s (1) national office not fully considering risk factors when selecting producers to include in the spot check sample, (2) county offices not consistently adding producers with questionable claims to the spot check sample, and (3) state offices not monitoring the quality of county offices’ spot checks.
We made four recommendations for the Farm Service Agency to conduct more rigorous reviews of Coronavirus Food Assistance Program applications. The agency generally agreed with our recommendations and took steps to address the limitations we identified related to its spot check reviews. Additionally, as of April 2024, the Farm Service Agency’s county offices had completed additional spot checks, but reporting and analysis were ongoing. We will review the agency’s process for these additional spot checks when they are complete and assess whether these actions are responsive to our recommendation.
· We found that the Health Resources and Services Administration (HRSA) did not promptly implement certain postpayment controls and processes in the Provider Relief Fund. The Provider Relief Fund was created in March 2020 to provide COVID-19 relief funds to health care providers and ensure access to essential health care services. The agency conducted a fraud risk assessment in 2021 and 2022 to help it identify fraud risks in the program as well as gaps in its existing controls and processes to address identified risks. In its 2021 assessment, the agency found that it had not documented analytic processes for what types of problematic payments should be flagged for further review and procedures for responding to allegations of potential fraud. To reduce risks, HRSA recommended that it document and standardize such processes and procedures. Despite making this recommendation in 2021, it took the agency until March 2023 to implement new standardized processes to flag problematic payments for review and until June 2023 to finalize procedures for responding to potential fraud.
Additionally, in October 2021, we reported that HRSA was slow to implement processes for recovering improper payments. We recommended that HRSA finalize procedures and seek postpayment recovery of any Provider Relief Fund overpayments, unused payments, and payments not properly used.[98] HRSA finalized its recovery processes in December 2022. In September 2023, we reported that HRSA had addressed our recommendation based on our review of its recovery processes and plan for seeking recovery of all types of payments in need of recovery.[99]
Key open recommendations. Our work has highlighted the importance of establishing controls and processes to manage program integrity risks. Federal agencies can be better positioned to manage improper payments and fraud risks during emergencies by implementing effective processes and controls to manage risks under normal conditions. Agencies can further improve their preparedness for emergencies by promptly implementing our recommendations and recommendations from their inspectors general. For example, in 2018, we recommended that the Internal Revenue Service (IRS) take steps to improve its efforts to authenticate taxpayers. IRS had not fully implemented these recommendations at the onset of the COVID-19 pandemic, and subsequently IRS officials raised concerns that fraudsters could be taking economic impact payments intended for eligible recipients. By taking actions to address the open recommendations prior to the COVID-19 pandemic, IRS might have had better controls and safeguards in place during the emergency to manage improper payment risks and help ensure that eligible individuals in need of economic impact payments received them.
Additionally, we have made recommendations to agencies across the federal government to mitigate program integrity risks in emergency assistance programs. Agencies have taken steps to address some of our recommendations to mitigate program integrity risks. However, additional actions could help federal agencies better manage such risks. For example:
· USDA’s Farm Service Agency should conduct additional reviews of Coronavirus Food Assistance Program payments and use a more risk-based approach to select producers for review.
· The Centers for Medicare & Medicaid Services (CMS) should conduct fingerprint‑based criminal background checks for high-risk provider types who enrolled during the COVID-19 public health emergency, such as when CMS revalidates these providers’ information.
· DOL should design and implement an antifraud strategy for unemployment insurance programs based on a fraud risk profile that is consistent with leading practices as provided in the Fraud Risk Framework.
Collecting and Sharing Data
|
|
Lessons Learned on Collecting and Sharing Data Collecting and sharing data can help federal agencies · effectively manage response activities, evaluate performance in meeting response goals, and make any midcourse adjustments as needed; · target and administer relief fund programs; and · enhance the early detection of public health emergencies. We have made recommendations to federal agencies to enhance their ability to collect and share data before and during public health emergencies. For example, we recommended that the Department of Health and Human Services complete a plan that includes actions for establishing an electronic nationwide public health situational awareness network and identify measurable steps for completing actions to establish the network. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
Managing response activities and evaluating performance. By collecting data, federal agencies can better manage the response and make timely decisions during a public health emergency. Our work examining the federal response to the COVID-19 pandemic found that without collecting necessary data, some agencies faced challenges making decisions to inform response activities and evaluating their performance in meeting response program goals. For example:
· In September 2020, we reported that CDC lacked the data it needed to prioritize the allocation of health resources among populations most affected by the pandemic.[100] As the nation’s health protection agency, CDC collected and reported data on COVID-19 cases, hospitalizations, deaths, and other indicators of the pandemic by race and ethnicity. However, we found that race and ethnicity information in the data reported to CDC by states and other entities was often incomplete. For instance, in March 2021, we found CDC lacked information on patients’ race and ethnicity for almost half of reported COVID-19 cases (47.2 percent) and vaccinations (46.7 percent).[101]
We recommended that CDC take steps to collect more complete data.[102] CDC agreed and took various actions that addressed our recommendation. For instance, in May 2021, agency officials stated it had conducted listening sessions with community health workers serving racial and ethnic communities and rural populations to gather input on the importance of collecting race and ethnicity data. Officials also stated that the agency planned to use this information to inform the development of appropriate messages to educate communities about the importance of providing race and ethnicity data when receiving health care services, among other things. Further, in August 2021, CDC officials stated that monitoring and assessing the completeness of race and ethnicity data in its COVID-19 data systems remains a priority, and that addressing the completeness and quality of demographic data is also part of larger, ongoing initiatives.
· In September 2021, we reported that USDA was unable to fully evaluate the performance of the Farmers to Families Food Box program in meeting the goals USDA established for the program because the agency did not collect needed data.[103] Through the program—which began in May 2020 and ended in May 2021—USDA contracted with distributors to purchase and deliver fresh fruits and vegetables, dairy, and meat products across the country. Its specific program goals included (1) providing food to those in need, (2) helping companies that supply and distribute goods to retain jobs, and (3) supporting domestic producers faced with declining demand. USDA determined that the program met its goal of providing food to those in need.
However, we found that USDA could not determine whether the program had achieved its other two goals—specifically, job retention and supporting domestic producers—because it did not collect necessary data to evaluate the program’s performance in meeting these goals. USDA officials said they did not collect these data because they implemented the program under tight time frames. We recommended that USDA take steps to help ensure it will apply the lesson learned regarding collecting and analyzing data to assess program goals when implementing future emergency food assistance programs. In April 2022, USDA reported that it had plans to apply this lesson learned to future programs.
Administering relief fund programs. By improving data systems, federal agencies can enhance their ability to effectively administer relief fund programs during future emergencies. Federal agencies use data systems to carry out various program responsibilities. However, we found some agencies experienced challenges utilizing data systems to manage COVID-19 relief fund programs. For example, we found that outdated data systems contributed to challenges in the unemployment insurance programs administered by state workforce agencies under the oversight of DOL.[104] State workforce agencies relied extensively on data systems, but many were legacy systems developed in the 1970s and 1980s. In June 2022, we noted that DOL’s Office of Inspector General found legacy systems were one of the causes of states’ inability to detect and recover fraudulent payments.[105] Specifically, state officials reported that their data systems did not have the capability to perform cross-matches—a method used to detect improper payments—for such a large volume of claims. Additionally, security vulnerabilities in legacy systems may pose a privacy risk as claimants’ personally identifiable information could become more easily accessible to criminals.
Enhancing the early detection of public health emergencies. Data systems enable officials across levels of government to share information, thus playing an important role in efforts to enhance the response to future public health emergencies. We previously reported that having a national public health situational awareness capability—that is, a capability for health care providers and public health officials at all levels of government to share real-time information—would help federal agencies detect emerging threats and prepare the response.[106] Figure 4 provides an illustration of the types of entities that have a role in sharing information to support nationwide public health situational awareness.
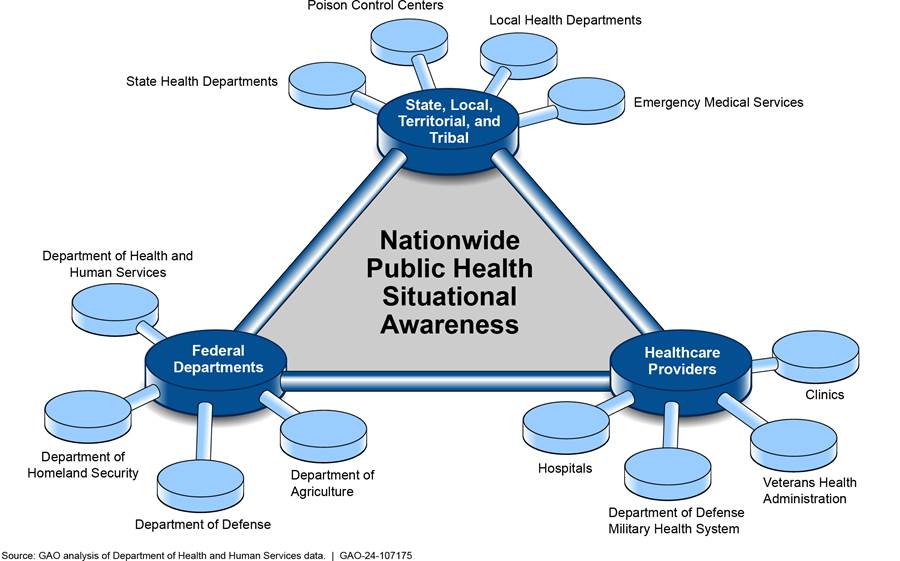
Since 2006, federal laws have required that HHS take steps toward improving the nation’s situational awareness of threats related to public health emergencies.[107] Specifically, HHS was required to establish an electronic nationwide public health situational awareness capability to facilitate sharing data and information to enhance both the early detection of, and rapid response to, infectious disease outbreaks and other public health emergencies.[108]
In 2017, we made three recommendations that HHS take steps toward meeting its mandate to establish a nationwide public health situational awareness capability by creating an integrated project team to conduct all activities required to establish and operate the capability. HHS has not fully addressed these recommendations.[109] While our work during the COVID-19 pandemic indicated HHS had made progress toward meeting its mandate, additional actions are still needed. For example:
· We reported in September 2020 that HHS launched a new data platform—HHS Protect—in April 2020 to help integrate COVID-19 data and other types of health information collected by various federal, state, and local public health and commercial entities.[110] HHS officials told us that they believe this platform has helped the agency in meeting its mandate to establish an electronic system to support public health situational awareness capabilities.
We agreed that HHS has implemented several systems related to public health situational awareness and biosurveillance.[111] However, the law called for a near real-time nationwide public health situational awareness capability consisting of interoperable systems to enable the simultaneous sharing of information needed to enhance situational awareness at the federal, tribal, state, and local levels of public health.[112] This capability does not exist today.[113]
· In June 2022, we reported that states and public health organizations experienced several challenges and identified lessons learned related to managing and sharing information during the pandemic, and that HHS can use these insights to inform its efforts to meet its mandate.[114] For instance, one state reported that because of the lack of interoperability among its health department systems, public health officials and stakeholders had to manually input data into different systems. Public health organizations told us that health-related information sharing was a challenge because states and local jurisdictions had separate vaccination management systems, limited visibility into other states’ data, and no visibility into vaccination data at the federal level.
Additionally, most states that responded to a survey we administered and public health organizations we met with identified lessons learned related to improving public health data reporting. These included standardizing and sharing data among federal entities and states to improve surveillance needs and collaborating with response partners—including states, territories, and local and tribal entities—to reduce reporting duplicative data.
Key open recommendations. We have made recommendations to federal agencies to improve data collection and data sharing capabilities. Federal agencies have taken steps to address some of these recommendations. However, additional actions could help enhance the response to future emergencies. For example:
· HHS should complete a plan that includes actions for establishing an electronic nationwide public health situational awareness network and develop a project management plan that identifies measurable steps for completing actions to establish the network.
· HHS should prioritize the development of the public health situational awareness and biosurveillance network by designating a lead operational division for the implementation of the Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019.
· HHS should ensure that the lead operational division for implementing its mandate request that state, territory, and local public health officials share their lessons learned from the COVID-19 pandemic with HHS, and incorporate lessons learned from the COVID-19 pandemic into its plans for implementing the situational awareness and biosurveillance network.
Leveraging Existing Infrastructure
|
|
Lessons Learned on Leveraging Existing Infrastructure Leveraging the existing infrastructure—including programs, partnerships, and systems—can help federal agencies implement timely activities to respond to a public health emergency and efficiently manage them. Specifically, federal agencies can use existing infrastructure to · facilitate the delivery of services and distribute federal relief funds, and · manage and oversee response programs. We identified instances during the COVID-19 pandemic where federal agencies successfully leveraged the existing infrastructure. For example, the Department of the Interior and the Indian Health Service leveraged existing program mechanisms to efficiently distribute COVID-19 relief funds to tribal recipients during the pandemic. We also made recommendations to federal agencies to seek such opportunities. Further, Congress may wish to consider enacting automatic increases in federal Medicaid spending during economic downturns to increase federal Medicaid support in a more timely and targeted fashion. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
Leveraging infrastructure to deliver services and distribute relief funds. Congress has leveraged the Medicaid program to quickly increase funding to states and ensure that eligible individuals maintained access to essential health care services during the COVID-19 pandemic and other times of crisis.[115] Most of the enhanced federal funding resulted from a 6.2 percent temporary increase in the federal matching rate for state and territorial Medicaid programs provided in the Families First Coronavirus Response Act.[116] To receive the enhanced federal funding during the pandemic, states were required to provide continuous coverage for certain beneficiaries who were enrolled in Medicaid on or after March 18, 2020, through the end of the month in which the public health emergency ended, among other requirements.
Under this policy, enrollment grew by over 30 percent, from about 64 million in February 2020 to about 86 million in February 2023. Spending for the enhanced federal funding totaled about $118 billion from January 2020 through March 2023. Congress ended the continuous enrollment requirement as of March 31, 2023, and the enhanced matching funds as of December 31, 2023.[117] In July 2024, we reported on state and federal efforts to redetermine eligibility and disenroll individuals who are no longer eligible, referred to as “unwinding,” and have ongoing work examining the outcomes of that process on Medicaid enrollment.[118] Further, we have previously recommended that Congress consider automatic increases in federal Medicaid spending during economic recessions based on each state’s increased unemployment and decreased revenues. Implementing an automatic, temporary change would increase federal Medicaid support in a more timely and targeted fashion.[119]
Using existing programs and mechanisms to administer billions of dollars in COVID-19 relief funds helped meet the needs of U.S. territories, Tribes, states, localities, and others and alleviate challenges when distributing funds. For example:
· Throughout the pandemic, we reported on the expansion of CMS’s Accelerated and Advanced Payments Program to provide support to Medicare suppliers and providers during the pandemic. This program provides loans to providers and suppliers during times when there is a disruption in claim submission and processing, including during the COVID-19 pandemic. Under the expanded program, active Medicare providers and suppliers could apply for loans up to 100 percent or 125 percent of the Medicare payments they received for the prior 3-month or 6-month period, depending on provider or supplier type. While no new loans related to the COVID-19 pandemic have been made under this program since January 2021, accelerated and advance payments helped some providers with cash flow issues early in the pandemic.[120]
· In September 2023, we reported that officials in U.S. territories told us they experienced fewer challenges administering and reporting on pre-existing federal programs that received additional money compared with programs that were newly created in COVID-19 relief funding legislation.[121] Similarly, in December 2022, we reported that the Department of the Interior and the Indian Health Services, two federal agencies with substantial experience working with Tribes, leveraged existing program mechanisms to distribute COVID-19 relief funds to tribal recipients during the pandemic. In contrast, agencies that lacked experience working with Tribes faced challenges when administering relief fund programs, which affected the timeliness and equity of relief fund allocations to recipients.[122]
Leveraging infrastructure to manage and oversee response programs. Leveraging existing programs facilitated the administration and oversight of COVID-19 relief funds during the pandemic. The CARES Act appropriated $25 billion to the Federal Transit Authority to support the transit industry through its Urbanized Area and Rural Area formula programs. Using these funds, the federal agency provided grants to state Departments of Transportation, local public transit systems, and Tribes to support and expand transit services, including services provided through buses, subways, and ferries in urban, rural, and tribal areas. Agency officials reported few challenges implementing CARES Act provisions and monitoring CARES Act grants, in part, because the funds were provided for existing programs that have procedures for administration and oversight.[123]
Leveraging existing data systems during the COVID-19 pandemic helped some federal agencies collect data needed to make program decisions and oversee relief funds. For example:
· In March 2023, we reported that CMS leveraged an existing data collection system to gather nursing home data to inform its program decisions. Specifically, CMS began requiring nursing homes to report data at least on a weekly basis—such as COVID-19 cases and deaths, access to personal protective equipment, and staffing shortages—to CDC’s existing national infection surveillance system, the National Healthcare Safety Network, in May 2020. CMS officials said collecting these data were critical to their response in nursing homes.[124]
· Federal agencies can leverage Treasury’s free payment integrity service, as well as existing program or agency data, to detect potential fraud. A leading practice in fraud data analytics is to conduct data mining and matching. For example, as we reported in May 2023, over the course of its COVID-19 pandemic response, SBA increased its use of data analytics to facilitate fraud detection and began using the Department of the Treasury’s Do Not Pay service in 2021 to screen applicants.[125]
We recommended that SBA take steps to further leverage existing data sources. Specifically, we recommended that SBA ensure that it had identified external sources of data that can facilitate the verification of applicant information and the detection of potential fraud across programs. Further, we recommended that SBA develop a plan for obtaining access to those external sources of data. As of May 2024, SBA has taken some steps to identify and develop a plan to access such data sources.
Key open recommendations and congressional consideration. We identified instances during the COVID-19 pandemic where federal agencies successfully leveraged programs, partnerships, and systems that facilitated the implementation and management of a timely response. Federal agencies should continue to seek opportunities to leverage existing infrastructure, particularly when responding to future public health emergencies. For example, SBA should
· ensure it has and utilizes mechanisms to facilitate cross-program data analytics, and
· continue taking steps to identify external data sources that could aid in fraud prevention and detection and develop a plan to obtain access to those data sources.
Further, Congress may wish to consider enacting automatic increases in federal Medicaid spending during economic downturns based on each state’s increased employment and decreased revenues. Implementing this automatic, temporary change would increase federal Medicaid support in a more timely and targeted fashion.
Implementing Program Flexibilities
|
|
Lessons Learned on Implementing Program Flexibilities Implementing flexibilities—such as telehealth and telework—during a public health emergency can help federal agencies · deliver services to program beneficiaries, · maintain activities to support critical operations, and · promote the safety of workers and the public. We have recommended that federal agencies examine the extent to which flexibilities utilized during the COVID-19 pandemic could be incorporated in standard operations or used during future emergencies. For example, we recommended that the Food and Drug Administration fully assess whether and how alternative inspection tools could help meet drug oversight objectives when in-person inspections are not possible in the future. |
Source: GAO (text); Kinder/stock.adobe.com (icons). | GAO‑24‑107175
Implementing program flexibilities. Implementing program flexibilities helped some federal agencies—such as CMS, FDA, and DOD—provide services to program beneficiaries, maintain operations to carry out their missions, and promote the safety of workers and the public during the COVID-19 pandemic. For example:
· Telehealth services played a critical role in maintaining Medicaid beneficiaries’ access to health care during the COVID-19 pandemic. While states had the flexibility to cover telehealth services prior to the pandemic, we reported in March 2022 that, in the five states we reviewed, the number of beneficiaries receiving telehealth services and the number of services provided via telehealth increased exponentially within the first 12 months of the pandemic.[126] Expanding the use of telehealth during the pandemic helped to mitigate pandemic-specific obstacles to receiving care while reducing patients’ risk of exposure to COVID-19, according to Medicaid officials in six states we reviewed. During this time, a variety of modalities were used by state Medicaid programs to deliver health care services via telehealth, as shown in figure 5.
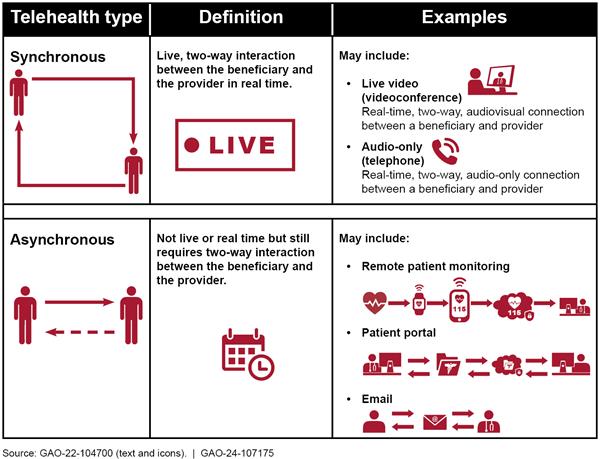
· During the COVID-19 pandemic, FDA largely paused on-site drug inspections and instead relied on alternative tools to help it carry out its mission of ensuring the safety and quality of drugs. Specifically, the agency utilized its various alternative inspection tools, including inspections conducted by foreign regulators, review of records and other information, drug sampling and testing, and remote interactive evaluation involving teleconferences, livestream video, and screen sharing of data and documents.[127] In January 2021, we reported that the agency used its alternative tools to identify and take some regulatory actions against manufacturing establishments with deficiencies.[128]
· DOD utilized and implemented various flexibilities as part of its efforts to promote the health of service members during the COVID-19 pandemic while continuing operations. In our June 2021 report, we found that DOD encouraged maximizing telework to the extent practicable to reduce service members’ risk of exposure.[129] Further, we found that DOD utilized telehealth services to promote safety while ensuring service members’ access to health care services. For instance, in February 2022, we reported that telehealth was a valuable tool in providing mental health care during the COVID-19 pandemic, according to DOD officials and military service officials.[130]
Key open recommendations. Our COVID-19 oversight work found that implementing program flexibilities helped some federal agencies continue providing services and maintain oversight activities during the pandemic. Such flexibilities also enhanced their ability to protect the safety of workers and the public by minimizing their risk of being exposed to COVID-19.
We have recommended that federal agencies examine flexibilities utilized during the pandemic to determine whether they can be incorporated into standard operations or utilized during future emergencies. While agencies have taken steps to address some of these recommendations, additional actions could help agencies better understand flexibilities utilized during the pandemic. For example:
· CMS should comprehensively assess the quality of Medicare services, including audio-only services, delivered using telehealth during the public health emergency. Such an assessment could include leveraging evidence from related efforts led by other HHS agencies.
· FDA should fully assess the agency’s alternative inspection tools and consider whether these tools or others could provide the information needed to supplement regular inspection activities or help meet its drug oversight objectives when inspections are not possible, for instance, during a future public health emergency.
Conclusions
Throughout the COVID-19 pandemic, federal agencies implemented COVID-19 relief programs; partnered with other federal agencies and private entities to develop and administer vaccines; and conducted a range of other actions to help the nation respond to and recover from the pandemic. We have made hundreds of recommendations to federal agencies and over 20 matters for congressional consideration to improve implementation, oversight, and transparency of the federal response. Across the federal government, agencies can help the nation prepare for, respond to, and recovery from future public health emergencies by taking steps to implement our recommendations that remain open.
Reflecting on federal agencies’ emergency response actions and our recommendations can reveal lessons from the COVID-19 pandemic for federal agencies. These lessons can help federal agencies identify actions that successfully facilitated the implementation of the federal response and should be incorporated into future emergency response plans. Other lessons can help federal agencies identify weaknesses in their response to the pandemic and identify areas for improvement. As the nation continues to recover from the pandemic and identifies and responds to new COVID-19 variants, we will continue to identify lessons learned. Incorporating these lessons can further enhance agencies’ preparedness for future emergencies.
Without including lessons learned in response plans, federal agencies could miss opportunities to improve their ability to plan for, respond to, and recover from emergencies. For example, Treasury has begun compiling resources, including the policies and procedures from its COVID-19 aviation assistance programs, to prepare for future financial disasters. However, we found that Treasury has not incorporated lessons from the COVID-19 emergency financial assistance provided to the aviation industry, including lessons we identified and those identified by other auditing entities, into its efforts. By doing so, Treasury can facilitate timely decisions to quickly implement programs, such as direct lending programs, in response to future financial disasters and potentially reduce program risks, such as the possibility of errors and omissions.
Recommendation
The Secretary of the Treasury should include key lessons from the COVID-19 emergency financial assistance provided to the aviation industry, including those lessons identified by GAO and other auditing entities, in the department’s ongoing efforts to compile resources to prepare for future financial disasters. (Recommendation 1)
Agency Comments
We provided the relevant draft sections of this report to Treasury and DOT for review and comment. A senior counsel with the Department of the Treasury stated via email that Treasury agrees with our recommendation and will take steps to implement it. Treasury also provided technical comments, which we incorporated as appropriate. DOT did not have any comments on the relevant draft report sections.
We are sending copies of this report to the appropriate congressional committees, the Office of Management and Budget, and certain executive branch agencies. In addition, this report is available online at no charge on the GAO website at https://www.gao.gov.
If you or your staff have any questions about this report, please contact me at 202-512-7144 or farbj@gao.gov. Contact points for our Offices of Congressional Relations and Public Affairs may be found on the last page of this report. GAO staff who made key contributions to this report are listed in appendix II.
Jessica Farb
Managing Director, Health Care
List of Congressional Committees
The Honorable Patty Murray
Chair
The Honorable Susan Collins
Vice Chair
Committee on Appropriations
United States Senate
The Honorable Ron Wyden
Chairman
The Honorable Mike Crapo
Ranking Member
Committee on Finance
United States Senate
The Honorable Bernard Sanders
Chair
The Honorable Bill Cassidy, M.D.
Ranking Member
Committee on Health, Education, Labor, and Pensions
United States Senate
The Honorable Gary C. Peters
Chairman
The Honorable Rand Paul, M.D.
Ranking Member
Committee on Homeland Security and Governmental Affairs
United States Senate
The Honorable Tom Cole
Chairman
The Honorable Rosa L. DeLauro
Ranking Member
Committee on Appropriations
House of Representatives
The Honorable Cathy McMorris Rodgers
Chair
The Honorable Frank Pallone, Jr.
Ranking Member
Committee on Energy and Commerce
House of Representatives
The Honorable Mark E. Green, M.D.
Chairman
The Honorable Bennie G. Thompson
Ranking Member
Committee on Homeland Security
House of Representatives
The Honorable James Comer
Chairman
The Honorable Jamie Raskin
Ranking Member
Committee on Oversight and Accountability
House of Representatives
The Honorable Jason Smith
Chairman
The Honorable Richard Neal
Ranking Member
Committee on Ways and Means
House of Representatives
Appendix I: Matters for Congressional Consideration to Improve the Transparency and Accountability of Emergency Relief Funds
During emergencies, federal agencies must get relief funds out quickly while ensuring appropriate financial safeguards are in place. We found early in the COVID-19 pandemic that agencies gave priority to swiftly distributing funds and implementing new programs. However, tradeoffs were made that limited progress in achieving transparency and accountability goals. Specifically, we found significant shortcomings in the application of fundamental internal controls and financial and fraud risk management practices. As a result, billions of dollars were at risk for improper payments, including those from fraud, providing limited assurance that programs effectively met their objectives. To help address these shortcomings, we have made the following 10 matters for congressional consideration to enhance the transparency and accountability of federal spending.[131]
· Congress should pass legislation requiring the Office of Management and Budget (OMB) to provide guidance for agencies to develop plans for internal control that would then immediately be ready for use in, or adaptation for, future emergencies or crises and requiring agencies to report these internal control plans to OMB and Congress. (Matter for Congressional Consideration 1)
· Congress should amend the Payment Integrity Information Act of 2019 to designate all new federal programs making more than $100 million in payments in any one fiscal year as “susceptible to significant improper payments” for their initial years of operation. (Matter for Congressional Consideration 2)
· Congress should amend the Payment Integrity Information Act of 2019 to reinstate the requirement that agencies report on their antifraud controls and fraud risk management efforts in their annual financial reports. (Matter for Congressional Consideration 3)
· Congress should establish a permanent analytics center of excellence to aid the oversight community in identifying improper payments and fraud. (Matter for Congressional Consideration 4)
· Congress should clarify that (1) chief financial officers (CFO) at CFO Act agencies have oversight responsibility for internal controls over financial reporting and key financial management information that includes spending data and improper payment information; and (2) executive agency internal control assessment, reporting, and audit requirements for key financial management information, discussed in an existing matter for congressional consideration in our August 2020 report, include internal controls over spending data and improper payment information. (Matter for Congressional Consideration 5)
· Congress should require agency CFOs to (1) submit a statement in agencies’ annual financial reports certifying the reliability of improper payments risk assessments and the validity of improper payment estimates, and describing the actions of the CFO to monitor the development and implementation of any corrective action plans; and (2) approve any methodology that is not designed to produce a statistically valid estimate. (Matter for Congressional Consideration 6)
· Congress should consider legislation to require improper payment information required to be reported under the Payment Integrity Information Act of 2019 to be included in agencies’ annual financial reports. (Matter for Congressional Consideration 7)
· Congress should amend the DATA Act to extend the previous requirement for agency inspectors general to review the completeness, timeliness, quality, and accuracy of their respective agency data submissions on a periodic basis. (Matter for Congressional Consideration 8)
· Congress should amend the DATA Act to clarify the responsibilities and authorities of OMB and Department of the Treasury for ensuring the quality of data available on USAspending.gov. (Matter for Congressional Consideration 9)
· Congress should amend the Social Security Act to accelerate and make permanent the requirement for the Social Security Administration to share its full death data with the Department of the Treasury’s Do Not Pay working system. (Matter for Congressional Consideration 10)
As of April 2024, all 10 of these matters for congressional consideration remain open; however, Congress has taken some steps to address some of them. For example, the Enhancing Improper Payment Accountability Act (H.R. 8343), which was introduced and referred to the House Committees on the Budget and on Oversight and Accountability on May 10, 2024, and reported out of the Committee on the Budget on May 16, 2024, includes provisions that would reinstate the requirement for agencies to report on their antifraud controls and fraud risk management efforts in their annual financial report. However, as of July 2024, a full vote in the House of Representatives has yet to be scheduled.
GAO contact
Jessica Farb, 202-512-7114 or farbj@gao.gov
Staff Acknowledgments:
In addition to the contacts named above, Raymond Sendejas (Assistant Director), Kristin Ekelund (Analyst-in-Charge), Sonia Chakrabarty, Derry Henrick, Ying Hu, and David Jones made key contributions to this report.
Products Related to Planning in Advance
Public Health Preparedness: HHS Should Address Strategic National Stockpile Coordination. Challenges. GAO‑24‑106260. Washington, D.C.: May 2, 2024.
Public Health Preparedness: Mpox Response Highlights Need for HHS to Address Recurring Challenges. GAO‑24‑106276. Washington, D.C.: Apr. 18, 2024.
Commercial Aviation: Key Lessons from COVID-19 Preparedness and Emergency Financial Assistance to the Industry. GAO‑24‑106754. Washington, D.C.: Mar. 18, 2024.
Veterans Affairs: Improvements Needed in Estimating Funding for Potential Future Health Emergencies. GAO‑24‑106359. Washington, D.C.: Feb. 8, 2024.
Public Health Preparedness: HHS Emergency Agency Needs to Strengthen Workforce Planning. GAO‑24‑106108. Washington, D.C.: Jan. 16, 2024.
Public Health Preparedness, HHS Should Plan for Medical Countermeasure Development and Manufacturing Risks. GAO‑23‑105713. Washington, D.C.: Feb. 2, 2023.
Veterans Affairs: Projection, Use, and Oversight of COVID-19 Relief Funding. GAO‑23‑105730. Washington, D.C.: Nov. 29, 2022.
COVID-19: Current and Future Federal Preparedness Requires Fixes to Improve Health Data and Address Improper Payments. GAO‑22‑105397. Washington, D.C.: Apr. 27, 2022.
Household Hazardous Waste Removal: EPA Should Develop a Formal Lessons Learned Process for Its Disaster Response. GAO‑22‑104276. Washington, D.C.: Mar. 17, 2022.
Paycheck Protection Program: Program Changes Increased Lending to the Smallest Businesses and in Underserved Locations. GAO‑21‑601. Washington, D.C.: Sept. 21, 2021.
Biodefense: After-Action Findings and COVID-19 Response Revealed Opportunities to Strengthen Preparedness. GAO‑21‑513. Washington, D.C.: Aug. 4, 2021.
COVID-19 Contracting: Opportunities to Improve Practices to Assess Prospective Vendors and Capture Lessons Learned. GAO‑21‑528. Washington, D.C.: July 29, 2021.
COVID-19: HHS Should Clarify Agency Roles for Emergency Return of U.S. Citizens During a Pandemic. GAO‑21‑334. Washington, D.C.: Apr. 19, 2021
Financial Assistance: Lessons Learned from CARES Act Loan Program for Aviation and Other Eligible Businesses. GAO‑21‑198. Washington, D.C.: Dec. 10, 2020.
COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions. GAO‑20‑701. Washington, D.C.: Sept. 21, 2020.
Air Travel and Communicable Diseases: Status of Research Efforts and Action Still Needed to Develop Federal Preparedness Plan. GAO‑20‑655T. Washington, D.C.: June 23, 2020.
National Biodefense Strategy: Additional Efforts Would Enhance Likelihood of Effective Implementation. GAO‑20‑273. Washington, D.C.: Feb. 19, 2020.
Disaster Response: HHS Should Address Deficiencies Highlighted by Recent Hurricanes in the U.S. Virgin Islands and Puerto Rico. GAO‑19‑592. Washington, D.C.: Sept. 20, 2019.
Air Travel and Communicable Diseases: Comprehensive Federal Plan Needed for U.S. Aviation System’s Preparedness. GAO‑16‑127. Washington, D.C.: Dec.16, 2015.
Products Related to Collaborating with Response Partners
Public Health Preparedness: HHS Should Address Strategic National Stockpile Coordination Challenges. GAO‑24‑106260. Washington, D.C.: May 2, 2024.
COVID-19: HHS and DOD Transitioned Vaccine Responsibilities to HHS, but Need to Address Outstanding Issues. GAO‑22‑104453. Washington, D.C.: Jan. 19, 2022.
Disaster Recovery: Additional Actions Needed to Identify and Address Potential Recovery Barriers. GAO‑22‑104039. Washington, D.C., Dec. 15, 2021.
Vaccine Development: Capabilities and Challenges for Addressing Infectious Diseases, GAO‑22‑104371. Washington, D.C.: Nov. 16, 2021.
COVID-19: Continued Attention Needed to Enhance Federal Preparedness, Response, Service Delivery, and Program Integrity. GAO‑21‑551. Washington: D.C.: July 19, 2021.
Depot Management: DOD Should Improve Pandemic Plans and Publish Working Capital Fund Policy. GAO‑21‑103. Washington, D.C.: Apr. 6, 2021.
COVID-19: Sustained Federal Action Is Crucial as Pandemic Enters Its Second Year. GAO‑21‑387. Washington, D.C.: Mar. 31, 2021.
COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions. GAO‑20‑701. Washington, D.C.: Sept. 21, 2020.
Products Related to Providing Clear and Timely Communications
COVID-19 Relief: Treasury Could Improve Its Administration and Oversight of State and Local Fiscal Recovery Funds. GAO‑24‑106027. Washington, D.C.: Dec. 14, 2023.
COVID-19: USAID Plans to Share Lessons Learned from Efforts to Meet Global Vaccination Goal. GAO‑23‑105579. Washington, D.C., Sept. 27, 2023.
COVID-19: HHS Agencies’ Planned Reviews of Vaccine Distribution and Communication Efforts Should Include Stakeholder Perspectives. GAO‑22‑104457. Washington, D.C.: Nov. 4, 2021.
COVID-19: Additional Actions Needed to Improve Accountability and Program Effectiveness of Federal Response. GAO‑22‑105051. Washington, D.C.: Oct. 27, 2021.
Economic Injury Disaster Loan Program: Additional Actions Needed to Improve Communication with Applicants and Address Fraud Risks. GAO‑21‑589. Washington, D.C.: July 30, 2021.
COVID-19: Efforts to Increase Vaccine Availability and Perspectives on Initial Implementation. GAO‑21‑443. Washington, D.C.: Apr. 14, 2021.
COVID-19: Critical Vaccine Distribution, Supply Chain, Program Integrity, and Other Challenges Require Focused Federal Attention. GAO‑21‑265. Washington, D.C.: Jan. 28, 2021.
Financial Assistance: Lessons Learned from CARES Act Loan Program for Aviation and Other Eligible Businesses. GAO‑21‑198. Washington, D.C.: Dec. 10, 2020.
COVID-19: Urgent Actions Needed to Better Ensure an Effective Federal Response. GAO‑21‑191. Washington, D.C.: Nov. 30, 2020.
COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions. GAO‑20‑701. Washington, D.C.: Sept. 21, 2020.
Influenza Pandemic: Lessons from the H1N1 Pandemic Should Be Incorporated into Future Planning. GAO‑11‑632. Washington, D.C.: June 27, 2011.
Products Related to Managing Program Integrity Risks
Fraud Risk Management: 2018-2022 Data Show Federal Government Loses an Estimated $233 Billion to $521 Billion Annually to Fraud, Based on Various Risk Environments. GAO‑24‑105833. Washington, D.C.: Apr. 16, 2024.
Small Business Administration: Progress and Work Remaining to Implement Key Management Improvements. GAO‑24‑107395. Washington, D.C.: Mar. 6, 2024.
Improper Payments and Fraud: How They Are Related but Different. GAO‑24‑106608. Washington, D.C.: Dec. 7, 2023.
COVID-19: Insights and Actions for Fraud Prevention. GAO‑24‑107157. Washington, D.C.: Nov. 14, 2023.
COVID-19 Provider Relief Fund: HRSA Continues to Recover Remaining Payments Due from Providers. GAO‑23‑106083. Washington, D.C.: Sept. 21, 2023.
Unemployment Insurance: Estimated Amount of Fraud during Pandemic Likely Between $100 Billion and $135 Billion. GAO‑23‑106696. Washington, D.C.: Sept. 12, 2023.
A Framework for Managing Improper Payments in Emergency Assistance Programs. GAO‑23‑105876. Washington, D.C.: July 13, 2023.
COVID Relief: Fraud Schemes and Indicators in SBA Pandemic Programs. GAO‑23‑105331. Washington, D.C.: May 18, 2023.
Emergency Relief Funds: Significant Improvements Are Needed to Address Fraud and Improper Payments. GAO‑23‑106556. Washington, D.C.: Feb. 1, 2023.
Unemployment Insurance: Data Indicate Substantial Levels of Fraud during the Pandemic; DOL Should Implement an Antifraud Strategy. GAO‑23‑105523. Washington, D.C.: Dec. 22, 2022.
Medicare: CMS Needs to Address Risks Posed by Provider Enrollment Waivers and Flexibilities. GAO‑23‑105494. Washington, D.C.: Dec. 19, 2022.
Coronavirus Food Assistance Program: USDA Should Conduct More Rigorous Reviews of Payments to Producers. GAO‑22‑104397. Washington, D.C.: Sept. 8, 2022.
Emergency Relief Funds: Significant Improvements Are Needed to Ensure Transparency and Accountability for COVID-19 and Beyond. GAO‑22‑105715. Washington, D.C.: Mar. 17, 2022.
COVID-19: Additional Actions Needed to Improve Accountability and Program Effectiveness of Federal Response. GAO‑22‑105051. Washington, D.C.: Oct. 27, 2021.
A Framework for Managing Fraud Risks in Federal Programs. GAO‑15‑593SP. Washington, D.C.: July 28, 2015.
Products Related to Collecting and Sharing Data
Unemployment Insurance: DOL Needs to Further Help States Overcome IT Modernization Challenges. GAO‑23‑105478. Washington, D.C.: July 10, 2023.
Public Health Emergencies: Data Management Challenges Impact National Response. GAO‑22‑106175. Washington, D.C.: Sept. 22, 2022.
COVID-19: Pandemic Lessons Highlight Need for Public Health Situational Awareness Network. GAO‑22‑104600. Washington, D.C.: June 23, 2022.
Unemployment Insurance: Transformation Needed to Address Program Design, Infrastructure, and Integrity Risks. GAO‑22‑105162. Washington, D.C.: June 7, 2022.
COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions. GAO‑20‑701. Washington, D.C.: Sept. 21, 2020.
USDA Food Box Program: Key Information and Opportunities to Better Assess Performance. GAO‑21‑353. Washington, D.C.: Sept. 8, 2021.
COVID-19: Sustained Federal Action Is Crucial as Pandemic Enters Its Second Year. GAO‑21‑387. Washington, D.C.: Mar. 31, 2021.
Public Health Information Technology: HHS Has Made Little Progress toward Implementing Enhanced Situational Awareness Network Capabilities. GAO‑17‑377. Washington, D.C.: Sept. 6, 2017.
Products Related to Leveraging Existing Infrastructure
Medicaid: Federal Oversight of State Eligibility Redeterminations Should Reflect Lessons Learned after COVID-19. GAO‑24‑106883. Washington, D.C.: July 18, 2024.
COVID-19: U.S. Territory Experiences Could Inform Future Federal Relief. GAO‑23‑106050. Washington, D.C.: Sept. 19, 2023.
COVID Relief: Fraud Schemes and Indicators in SBA Pandemic Programs. GAO‑23‑105331. Washington, D.C.: May 18, 2023.
COVID-19 in Nursing Homes: Experts Identified Actions Aimed at Improving Infection Prevention and Control. GAO‑23‑105613. Washington, D.C.: Mar. 20, 2023.
COVID-19 Relief Funds: Lessons Learned Could Improve Future Distribution of Federal Emergency Relief to Tribal Recipients. GAO‑23‑105473. Washington, D.C.: Dec. 15, 2022.
COVID-19: Current and Future Federal Preparedness Requires Fixes to Improve Health Data and Address Improper Payments. GAO‑22‑105397. Washington, D.C.: Apr. 27, 2022.
Medicaid in Times of Crisis. GAO‑21‑343SP. Washington, D.C.: Feb. 17, 2021.
COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions. GAO‑20‑701. Washington, D.C.: Sept. 21, 2020.
COVID-19: Opportunities to Improve Federal Response and Recovery Efforts. GAO‑20‑625. Washington, D.C.: June 25, 2020.
Medicaid: Prototype Formula Would Provide Automatic, Targeted Assistance to States during Economic Downturns. GAO‑12‑38. Washington, D.C., Nov. 10, 2011.
Products Related to Implementing Program Flexibilities
Medicare Telehealth: Actions Needed to Strengthen Oversight and Help Providers Educate Patients on Privacy and Security Risks.GAO‑22‑104454. Washington, D.C.: Sept. 26, 2022.
Medicaid: CMS Should Assess Effect of Increased Telehealth Use on Beneficiaries’ Quality of Care.GAO‑22‑104700. Washington, D.C.: Mar. 31, 2022.
Drug Safety: FDA Should Take Additional Steps to Improve Its Foreign Inspection Program. GAO‑22‑103611. Washington, D.C.: Feb. 22, 2022.
Defense Health Care: DOD Expanded Telehealth for Mental Health Care during the COVID-19 Pandemic. GAO‑22‑105149. Washington, D.C.: Feb. 3, 2022.
COVID-19: DOD Has Focused on Strategy and Oversight to Protect Military Servicemember Health. GAO‑21‑321. Washington, D.C.: June 3, 2021.
COVID-19: Critical Vaccine Distribution, Supply Chain, Program Integrity, and Other Challenges Require Focused Federal Attention. GAO‑21‑265. Washington, D.C.: Jan. 28, 2021.
GAO’s Mission
The Government Accountability Office, the audit, evaluation, and investigative arm of Congress, exists to support Congress in meeting its constitutional responsibilities and to help improve the performance and accountability of the federal government for the American people. GAO examines the use of public funds; evaluates federal programs and policies; and provides analyses, recommendations, and other assistance to help Congress make informed oversight, policy, and funding decisions. GAO’s commitment to good government is reflected in its core values of accountability, integrity, and reliability.
Obtaining Copies of GAO Reports and Testimony
The fastest and easiest way to obtain copies of GAO documents at no cost is through our website. Each weekday afternoon, GAO posts on its website newly released reports, testimony, and correspondence. You can also subscribe to GAO’s email updates to receive notification of newly posted products.
Order by Phone
The price of each GAO publication reflects GAO’s actual cost of production and distribution and depends on the number of pages in the publication and whether the publication is printed in color or black and white. Pricing and ordering information is posted on GAO’s website, https://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077,
or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card, MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or Email Updates. Listen to our Podcasts.
Visit GAO on the web at https://www.gao.gov.
To Report Fraud, Waste, and Abuse in Federal Programs
Contact FraudNet:
Website: https://www.gao.gov/about/what‑gao‑does/fraudnet
Automated answering system: (800) 424-5454 or (202) 512-7700
Congressional Relations
A. Nicole Clowers, Managing Director, ClowersA@gao.gov, (202) 512-4400, U.S. Government Accountability Office, 441 G Street NW, Room 7125, Washington, DC 20548
Public Affairs
Sarah Kaczmarek, Acting Managing Director, KaczmarekS@gao.gov, (202) 512-4800, U.S.
Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
Strategic Planning and External Liaison
Stephen J. Sanford, Managing
Director, spel@gao.gov, (202) 512-4707
U.S. Government Accountability Office, 441 G Street NW, Room 7814, Washington,
DC 20548
[1]The death counts from the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics include those with COVID-19, coded to ICD-10 code U07.1, as an underlying or contributing cause of death on the death certificate. Data are provisional and subject to updates. Data for recent periods are incomplete because of the lag in time between when deaths occur and when a death certificate is completed, submitted to the National Center for Health Statistics, and processed for reporting. This delay can range from 1 to 8 weeks or more. See Centers for Disease Control and Prevention, National Center for Health Statistics, “United States COVID-19 Hospitalizations, Deaths, Emergency Department (ED) Visits, and Test Positivity by Geographic Area,” accessed May 6, 2024 https://covid.cdc.gov/covid‑data‑tracker/#maps_percent‑covid‑deaths.
[2]HHS first declared the COVID-19 pandemic a public health emergency under section 319 of the Public Health Service Act on January 30, 2020. In addition, on March 13, 2020, the President declared COVID-19 a national emergency under the National Emergencies Act and a nationwide emergency under section 501(b) of the Robert T. Stafford Disaster Relief and Emergency Assistance Act (Stafford Act). The President also approved major disaster declarations under the Stafford Act for all 50 states, the District of Columbia, five U.S. territories, and certain Tribes. The national emergency declaration terminated on April 10, 2023, and the Stafford Act declaration terminated on May 11, 2023.
[3]For the purpose of our review, the COVID-19 relief laws consist of the six laws providing comprehensive relief across federal agencies and programs that the Department of the Treasury uses to record and track COVID-19 relief spending, in accordance with guidance issued by the Office of Management and Budget (OMB). These six laws are the American Rescue Plan Act of 2021, Pub. L. No. 117-2, 135 Stat. 4; Consolidated Appropriations Act, 2021, Pub. L. No. 116-260, div. M and N, 134 Stat. 1182 (2020); Paycheck Protection Program and Health Care Enhancement Act, Pub. L. No. 116-139, 134 Stat. 620 (2020); CARES Act, Pub. L. No. 116-136, 134 Stat. 281 (2020); Families First Coronavirus Response Act, Pub. L. No. 116-127, 134 Stat. 178 (2020); and the Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, Pub. L. No. 116-123, 134 Stat. 146. Further, the $4.65 trillion total reflects rescissions of COVID-19 relief funding that were enacted in the Fiscal Responsibility Act of 2023, Pub. L. No. 118-5, 137 Stat. 10, 23-30, div. B, tit. I (June 3, 2023), and other laws.
[4]Pub. L. No. 116-136, § 19010, 134 Stat. at 579–81. The American Rescue Plan Act of 2021 also includes a provision for GAO to conduct oversight of the COVID-19 response. Pub. L. No. 117-2, § 4002, 135 Stat. at 78.
[5]Additionally, we closed 10 recommendations as not implemented or as no longer valid. Reasons for closing recommendations as no longer valid include when a law has been amended or repealed; when a program has been terminated, replaced, or changed; when an office is terminated; or when the opportunity for implementation has passed, such as with a pilot project. For example, we made a recommendation in September 2020 related to collecting more complete data on COVID-19 cases and deaths in nursing homes retrospectively back to January 1, 2020, and clarifying the extent to which nursing homes reported data before May 8, 2020. As of October 2023, the recommendation remained unimplemented. We determined that, at this point in time, retrospectively collecting data prior to May 8, 2020, could prove burdensome for both nursing homes and HHS and detract resources that could otherwise be used to support resident care. See https://www.gao.gov/coronavirus/coronavirus‑recommendations for more information on our COVID-19 oversight recommendations.
[6]The High Risk List identifies government operations with vulnerabilities to fraud, waste, abuse, and mismanagement, or in need of transformation. We added HHS’s leadership and coordination of public health emergencies and the Unemployment Insurance system to our High Risk List in 2022. We added emergency loans to small businesses to the High Risk List in 2021. GAO, High-Risk Series: Efforts Made to Achieve Progress Need to Be Maintained and Expanded to Fully Address All Areas, GAO‑23‑106203 (Washington, D.C.: Apr. 20, 2023).
[7]HHS is the federal agency responsible for leading the nation’s preparedness for and response to public health emergencies. GAO, Public Health Preparedness: Mpox Response Highlights Need for HHS to Address Recurring Challenges, GAO‑24‑106276 (Washington, D.C.: Apr. 18, 2024).
[8]GAO, Unemployment Insurance: Data Indicate Substantial Levels of Fraud during the Pandemic; DOL Should Implement an Antifraud Strategy, GAO‑23‑105523 (Washington, D.C.: Dec. 22, 2022).
[9]GAO, COVID Relief: Fraud Schemes and Indicators in SBA Pandemic Programs, GAO‑23‑105331 (Washington, D.C.: May 18, 2023).
[10]We reviewed public statements from the Department of Justice from March 2020 through March 2024 to determine the status and characteristics of federal COVID-19 fraud-related cases. Specifically, we identified cases involving federal COVID-19 relief programs, including the Paycheck Protection Program, the Economic Injury Disaster Loan program, and the Unemployment Insurance program. We identified these cases by searching for relevant Department of Justice press releases and analyzing corresponding court documentation available in the Public Access to Court Electronic Records.
[11]COVID-19-associated deaths are those with COVID-19 listed as an underlying (i.e., primary) or contributing cause of death using the International Classification of Diseases, Tenth Revision (code U07.1). Data are from CDC WONDER as of May 1, 2024. Data for 2020 and 2021 are final. Data from 2022 through April 2024 are provisional and subject to change. Of the COVID-19-associated deaths that occurred between 2020 and 2024, COVID-19 was listed as the underlying cause in about 86 percent of deaths.
[12]Deaths with COVID-19 listed as the underlying (i.e., primary) cause of death were used to determine the ranking in the leading causes of death.
[13]These figures represent the 7-day rolling average of adult and pediatric patient case counts reported by hospitals in U.S. states and territories and included in HHS’s COVID-19 Reported Patient Impact and Hospital Capacity dataset, as of May 3, 2024.
[14]An estimated 17.8 percent (95 percent confidence interval:17.3 – 18.3) of U.S. adults had ever experienced long COVID and 5.3 percent (95 percent confidence interval: 5.0 – 5.6) were currently experiencing long COVID at the time of the survey. Questions to assess the prevalence of long COVID—meaning that there was a presence of symptoms that lasted 3 months or longer—on the Household Pulse Survey are through an ongoing partnership between the Census Bureau and the National Center for Health Statistics. The data are released as part of the Census Bureau’s Experimental Statistical Products Series. For more information, including limitations, see National Center for Health Statistics, U.S. Census Bureau, Household Pulse Survey, 2022–2024. Long COVID, accessed June 3, 2024, https://www.cdc.gov/nchs/covid19/pulse/long‑covid.htm.
[15]Inflation is the increase in the prices of goods and services over time and is typically measured as the percentage change in those prices over a set period, often 1 year or 1 month. For example, an annual inflation rate of 2 percent means that the prices of goods and services, on average, increased 2 percent over the past year. In previous work, we identified a number of indicators of current and expected future inflation to help us monitor households’ experiences with rising prices and assess the extent to which prices are likely to continue to rise over time. See GAO, COVID-19: Additional Actions Needed to Improve Accountability and Program Effectiveness of Federal Response, GAO‑22‑105051 (Washington, D.C.: Oct. 27, 2021).
[16]Annual inflation indicators include the year-over-year changes in the Personal Consumption Expenditures price index, the Consumer Price Index (CPI), the median CPI, and the 16 percent trimmed mean CPI. The median CPI and 16 percent trimmed mean CPI indicators focus on underlying inflation trends by omitting outliers.
[17]The Federal Reserve System’s Federal Open Market Committee determines the direction of monetary policy by directing open market operations. It aims for annual inflation of 2 percent on average over time and aims to achieve rates of inflation that are above 2 percent for some time after periods during which inflation has been persistently below 2 percent. See Federal Reserve, Federal Open Market Committee, “Statement on Longer-Run Goals and Monetary Policy Strategy” (Washington, D.C.: Jan. 30, 2024), accessed July 15, 2024, https://www.federalreserve.gov/monetarypolicy/historical‑statements‑on‑longer‑run‑goals‑and‑monetary‑policy‑strategy.htm.
[18]Measuring annual inflation provides a longer and potentially less volatile perspective on inflation while monthly inflation is more useful for assessing whether recent price pressures are waning or intensifying. Monthly inflation indicators include the month-over-month changes in the Personal Consumption Expenditures price index, CPI, the median CPI, and the 16 percent trimmed mean CPI.
[19]The employment-to-population ratio was 60.3 percent in March 2024, 0.2 percentage points higher than in February 2024 and 0.8 percentage points lower than in February 2020. The labor force participation rate was 62.7 percent in March 2024, 0.2 percentage points higher than in February 2024 and 0.7 percentage points lower than in February 2020. These differences likely reflect a combination of population aging and other pre-pandemic trends, as well as a lasting negative effect of the pandemic.
[20]Treasury records and tracks COVID-19 relief spending, in accordance with OMB guidance. Amounts presented from Treasury’s Governmentwide Treasury Account Symbol Adjusted Trial Balance System are the most recent available at the time of our analysis. Federal agencies use this system to provide proprietary financial reporting and budgetary execution information to Treasury. These amounts can fluctuate from month to month, and they reflect appropriations, as well as transfers, adjustments, recoveries, rescissions, and returns of unused indefinite appropriations. OMB’s guidance for recording and tracking COVID-19 relief spending does not include increases in Medicaid and Medicare spending; otherwise, the cumulative amount of funding as of April 30, 2024—the most recent date for which government-wide information was available at the time of our analysis—would be greater than about $4.65 trillion. Further, the $4.65 trillion total reflects rescissions of COVID-19 relief funding enacted in the Fiscal Responsibility Act of 2023, Pub. L. No. 118-5, 137 Stat. 10, 23-30, div. B, tit. I (2023), and other laws.
[21]The remaining $927.7 billion in COVID-19 relief funding was used for other spending areas. Agencies reported obligations totaling $883.4 billion and expenditures totaling $803.9 billion in these other spending areas.
[22]As defined by the National Biodefense Strategy, biological incidents are: (1) any act of biological warfare or terrorism, (2) a crime involving a biohazard, or (3) any natural or accidental occurrence in which a biohazard harms humans, animals, plants, or the environment.
[23]See GAO, National Biodefense Strategy: Additional Efforts Would Enhance Likelihood of Effective Implementation, GAO‑20‑273 (Washington, D.C.: Feb. 19, 2020).
[24]The biodefense enterprise is the whole combination of systems at every level of government and the private sector that contribute to protecting the nation and its citizens. It is composed of a complex collection of federal, tribal, state, local, territorial, and private resources, programs, and initiatives designed for different purposes and dedicated to mitigating both natural and intentional risk.
[25]GAO, Biodefense: After-Action Findings and COVID-19 Response Revealed Opportunities to Strengthen Preparedness, GAO‑21‑513 (Washington, D.C.: Aug. 4, 2021). In the context of emergency management and related functions, a capability is the combination of leadership and organization, planning, personnel, training, equipment and systems, and assessment needed to successfully execute a particular mission.
[26]GAO, Commercial Aviation: Key Lessons from COVID-19 Preparedness and Emergency Financial Assistance to the Industry, GAO‑24‑106754 (Washington, D.C.: Mar. 18, 2024).
[27]GAO, Air Travel and Communicable Diseases: Status of Research Efforts and Action Still Needed to Develop Federal Preparedness Plan, GAO‑20‑655T (Washington, D.C.: June 23, 2020).
[28]GAO, Air Travel and Communicable Diseases: Comprehensive Federal Plan Needed for U.S. Aviation System’s Preparedness, GAO‑16‑127 (Washington, D.C.: Dec. 16, 2015).
[30]Consolidated Appropriations Act, 2023, Pub. L. No. 117-328, § 105, 136 Stat. 4459, 5253-55 (2022).
[31]The other three HHS component agencies involved with public health emergency responses are the National Institutes of Health, the Indian Health Service, and the Health Resources and Services Administration.
[33]GAO, COVID-19: HHS Should Clarify Agency Roles for Emergency Return of U.S. Citizens During a Pandemic, GAO‑21‑334 (Washington, D.C.: Apr. 19, 2021).
[34]Mpox was formerly known as monkeypox. The World Health Organization recommended the name change in November 2022.
[35]The Strategic National Stockpile is part of the federal medical response infrastructure and can supplement medical countermeasures, such as vaccines and antivirals, needed by Tribes, states, U.S. territories, and localities during public health emergencies. The countermeasures in the stockpile can be used when the supply of these materials may not be available or sufficient. GAO, Public Health Preparedness: HHS Should Address Strategic National Stockpile Coordination Challenges, GAO‑24‑106260 (Washington, D.C.: May 2, 2024).
[38]GAO, Disaster Response: HHS Should Address Deficiencies Highlighted by Recent Hurricanes in the U.S. Virgin Islands and Puerto Rico, GAO‑19‑592 (Washington, D.C.: Sept. 20, 2019). This report included seven recommendations to ASPR, including that ASPR develop agreements with support agencies that include response capability and limitation information. As of May 2024, ASPR had taken steps to close six of these recommendations.
[39]GAO, Public Health Preparedness: HHS Emergency Agency Needs to Strengthen Workforce Planning, GAO‑24‑106108 (Washington, D.C.: Jan. 16, 2024).
[40]GAO, Veterans Affairs: Improvements Needed in Estimating Funding for Potential Future Health Emergencies, GAO‑24‑106359 (Washington, D.C.: Feb. 8, 2024) and Veterans Affairs: Projection, Use, and Oversight of COVID-19 Relief Funding, GAO‑23‑105730 (Washington, D.C.: Nov. 29, 2022).
[41]GAO, COVID-19: Current and Future Federal Preparedness Requires Fixes to Improve Health Data and Address Improper Payments, GAO‑22‑105397 (Washington, D.C.: Apr. 27, 2022); Paycheck Protection Program: Program Changes Increased Lending to the Smallest Businesses and in Underserved Locations, GAO‑21‑601 (Washington, D.C.: Sept. 21, 2021); and COVID-19: Federal Efforts Could Be Strengthened by Timely and Concerted Actions, GAO‑20‑701 (Washington, D.C.: Sept. 21, 2020).
[42]GAO, COVID-19 Contracting: Opportunities to Improve Practices to Assess Prospective Vendors and Capture Lessons Learned, GAO‑21‑528 (Washington, D.C.: July 29, 2021).
[43]GAO, Public Health Preparedness, HHS Should Plan for Medical Countermeasure Development and Manufacturing Risks, GAO‑23‑105713 (Washington, D.C.: Feb. 2, 2023).
[44]GAO, Financial Assistance: Lessons Learned from CARES Act Loan Program for Aviation and Other Eligible Businesses, GAO‑21‑198 (Washington, D.C.: Dec.10, 2020).
[45]GAO‑21‑198 and GAO, Commercial Aviation: Key Lessons from COVID-19 Preparedness and Emergency Financial Assistance to the Industry, GAO‑24‑106754 (Washington, D.C.: Mar. 18, 2024).
[46]Office of the Special Inspector General for Pandemic Recovery, Audit of the U.S. Department of the Treasury’s Process for Its Direct Loan to YRC, Worldwide, Inc. Under Section 4003 of the CARES Act, SIGPR-A-22-005 (Alexandria, Va.: May 11, 2023).
[47]We also reported in December 2020 that Treasury executed the loan in July 2020 before it had finalized procedures for evaluating applications. See GAO‑21‑198. On February 5, 2024, Yellow Corporation announced it had fully repaid its loan, including $700 million in principal and more than $151 million in interest.
[49]GAO, Household Hazardous Waste Removal: EPA Should Develop a Formal Lessons Learned Process for Its Disaster Response, GAO‑22‑104276 (Washington, D.C.: Mar. 17, 2022).
[50]The Emergency Economic Stabilization Act of 2008, designed to restore liquidity and stability to the financial system and to preserve homeownership, authorized Treasury to create the Troubled Asset Relief Program to assist borrowers struggling to make their mortgage payments. Pub. L. No. 110-343, 122 Stat. 3765.
[51]GAO, COVID-19: HHS and DOD Transitioned Vaccine Responsibilities to HHS, but Need to Address Outstanding Issues, GAO‑22‑104453 (Washington, D.C.: Jan. 19, 2022).
[52]Contracts with a priority rating under the Defense Production Act require a contractor to give preference to these contracts over any other unrated contracts if the contractor cannot meet all required delivery date needs for all contracts. See 50 U.S.C. § 4511.
[53]GAO, COVID-19: Sustained Federal Action Is Crucial as Pandemic Enters Its Second Year, GAO‑21‑387 (Washington, D.C.: Mar. 31, 2021).
[54]GAO, COVID-19: Continued Attention Needed to Enhance Federal Preparedness, Response, Service Delivery, and Program Integrity, GAO‑21‑551 (Washington, D.C.: July 19, 2021).
[57]GAO, Vaccine Development: Capabilities and Challenges for Addressing Infectious Diseases, GAO‑22‑104371 (Washington D.C.: Nov. 16, 2021).
[58]GAO, Depot Maintenance: DOD Should Improve Pandemic Plans and Publish Working Capital Fund Policy, GAO‑21‑103 (Washington D.C.: Apr. 6, 2021).
[59]The Army, Marine Corps, Navy, and Air Force operate 21 depots that are crucial to sustaining military readiness. 10 U.S.C. § 2476.
[60]Department of Defense, Undersecretary of Defense (Acquisition and Sustainment), Defense Industrial Base Essential Critical Infrastructure Workforce, Memorandum to the Defense Industrial Base (March 20, 2020).
[61]DOD’s Pandemic Operations Plan states that, at the outbreak of a pandemic, the Office of the Under Secretary of Defense for Acquisitions and Sustainment will notify the Defense Industrial Base and contractor workforce that they are mission-essential personnel who provide essential services required to meet national security commitments to the federal government and U.S. military.
[65]For example, the CARES Act loan program required businesses not to reduce their employee levels by more than 10 percent from March 24, 2020, through September 30, 2020. However, many businesses had substantial drops in revenue—in some cases drops greater than 95 percent—following the onset of the pandemic and had to make tradeoffs related to maintaining employment levels while awaiting loan decisions.
[67]GAO, COVID-19: Urgent Actions Needed to Better Ensure an Effective Federal Response, GAO‑21‑191 (Washington, D.C.: Nov. 30, 2020).
[69]GAO, COVID-19 Relief: Treasury Could Improve Its Administration and Oversight of State and Local Fiscal Recovery Funds, GAO‑24‑106027 (Washington D.C.: Dec. 14, 2023).
[70]In March 2021, the American Rescue Plan Act of 2021 appropriated $350 billion through the SLFRF to help tribal governments, states, localities, the District of Columbia, and U.S. territories cover costs stemming from the negative health and economic effects of the COVID-19 pandemic.
[71]In September 2022, Treasury notified SLFRF recipients of the funding constraints affecting its ability to provide ongoing support to SLFRF and other COVID-19 relief program recipients served by the Contact Center. Treasury reduced and later shut down these activities because it said it had limited funds to support these efforts. Treasury subsequently reopened its phone support and increased the number of Contact Center staff after receiving authority in the Consolidated Appropriations Act, 2023, to use certain unobligated funds to cover administrative expenses necessary to respond to the COVID-19 pandemic.
[72]IT-related inquiries included those related to using Treasury’s online reporting portal to submit required SLFRF reports. SLFRF policy-related inquiries included questions on allowable uses of funds.
[74]GAO, COVID-19: Critical Vaccine Distribution, Supply Chain, Program Integrity, and Other Challenges Require Focused Federal Attention, GAO‑21‑265 (Washington D.C.: Jan. 28, 2021).
[75]GAO, COVID-19: Efforts to Increase Vaccine Availability and Perspectives on Initial Implementation, GAO‑21‑443 (Washington D.C.: Apr. 14, 2021) and COVID-19: HHS Agencies’ Planned Reviews of Vaccine Distribution and Communication Efforts Should Include Stakeholder Perspectives, GAO‑22‑104457 (Washington D.C.: Nov. 4. 2021).
[76]GAO, Influenza Pandemic: Lessons from the H1N1 Pandemic Should Be Incorporated into Future Planning, GAO‑11‑632 (Washington, D.C.: June 27, 2011).
[79]GAO, COVID-19: USAID Plans to Share Lessons Learned from Efforts to Meet Global Vaccination Goal, GAO‑23‑105579 (Washington D.C.: Sept. 27, 2023).
[80]The Payment Integrity Information Act of 2019, codified at 31 U.S.C. §§ 3351-58, defines improper payments as any payments that should not have been made or that were made in an incorrect amount (including overpayments and underpayments) under statutory, contractual, administrative, or other legally applicable requirements. Improper payments include any payment to an ineligible recipient or for an ineligible service, duplicate payments, payments for services not received (except where authorized by law), and any payment for an incorrect amount. 31 U.S.C. § 3351(4). Executive agency estimates of improper payments also treat as improper any payments whose propriety cannot be determined due to lacking or insufficient information. 31 U.S.C. § 3352(c)(2).
[81]GAO, Improper Payments and Fraud: How They Are Related but Different, GAO‑24‑106608 (Washington, D.C.: Dec. 7, 2023).
[82]GAO, Unemployment Insurance: Estimated Amount of Fraud during Pandemic Likely Between $100 Billion and $135 Billion, GAO‑23‑106696 (Washington, D.C.: Sept. 12, 2023).
[83]This estimate includes loans from the Paycheck Protection Program, COVID-19 Economic Injury Disaster Loan program, and Targeted Advances and Supplemental Targeted Advances from the COVID-19 Economic Injury Disaster Loan program. See Small Business Administration, Office of Inspector General, COVID-19 Pandemic EIDL and PPP Loan Fraud Landscape, White Paper Report 23-09 (June 27, 2023).
[84]GAO, Fraud Risk Management: 2018-2022 Data Show Federal Government Loses an Estimated $233 Billion to $521 Billion Annually to Fraud, Based on Various Risk Environments, GAO‑24‑105833 (Washington, D.C.: Apr. 16, 2024).
[85]GAO‑23‑105331; Emergency Relief Funds: Significant Improvements Are Needed to Ensure Transparency and Accountability for COVID-19 and Beyond, GAO‑22‑105715 (Washington, D.C.: Mar. 17, 2022); and GAO‑23‑106696.
[86]The federal government may enforce laws through civil or criminal action. Such action may be resolved through a trial, a permanent injunction, a civil settlement, or a guilty plea. Our analysis is limited to the cases we identified from public sources and may not include all criminal and civil cases charged by the Department of Justice as of March 31, 2024. Additionally, details of fraud cases and schemes presented in court documents may not be complete. Further, cases that reach the prosecution stage in the fraud identification life cycle represent a fraction of the instances of fraud or all possible fraud cases.
[87]The range in length of prison sentencing varies, in part, based on factors such as prior convictions and whether there were other charges in addition to COVID-19-related fraud. Courts refer to the United States Sentencing Commission Guidelines to determine the particular sentence in each individual case. Under 28 U.S.C. § 994, the Guidelines should reflect a variety of factors and considerations to determine an appropriate sentence. The Guidelines set a base offense level and then add or subtract levels due to aggravating or mitigating circumstances, such as the dollar amount of the loss caused by the offense and the defendant’s criminal history, ultimately arriving at a suggested sentencing range. Additionally, many of the defendants we reviewed were convicted on additional charges beyond fraud against COVID-19 relief programs, which would affect the length of their sentences. Sentences ranged from probation to 30 years in prison and court ordered restitution amounts ranged from zero to over $70 million.
[88]A charge is merely an allegation, and all defendants are presumed innocent until proven guilty beyond a reasonable doubt in a court of law.
[89]The Pandemic Unemployment Fraud Recoupment Act (S. 1018) contains provisions that would address this request. As of July 17, 2024, this bill has not been passed by Congress.
[90]GAO, A Framework for Managing Improper Payments in Emergency Assistance Programs, GAO‑23‑105876 (Washington D.C.: July 13, 2023) and A Framework for Managing Fraud Risks in Federal Programs, GAO‑15‑593SP (Washington D.C.: July 28, 2015).
[91]GAO, Emergency Relief Funds: Significant Improvements Are Needed to Address Fraud and Improper Payments, GAO‑23‑106556 (Washington, D.C: Feb. 1, 2023).
[93]GAO, Small Business Administration: Progress and Work Remaining to Implement Key Management Improvements, GAO‑24‑107395 (Washington, D.C.: Mar. 6, 2024).
[94]GAO, COVID-19: Insights and Actions for Fraud Prevention, GAO‑24‑107157 (Washington, D.C.: Nov. 14, 2023).
[97]GAO, Coronavirus Food Assistance Program: USDA Should Conduct More Rigorous Reviews of Payments to Producers, GAO‑22‑104397 (Washington, D.C.: Sept. 8, 2022).
[99]GAO, COVID-19 Provider Relief Fund: HRSA Continues to Recover Remaining Payments Due from Providers, GAO‑23‑106083 (Washington, D.C.: Sept. 21, 2023).
[103]GAO, USDA Food Box Program: Key Information and Opportunities to Better Assess Performance, GAO‑21‑353 (Washington D.C.: Sept. 8, 2021).
[104]GAO, Unemployment Insurance: DOL Needs to Further Help States Overcome IT Modernization Challenges, GAO‑23‑105478 (Washington D.C.: July 10, 2023).
[105]GAO, Unemployment Insurance: Transformation Needed to Address Program Design, Infrastructure, and Integrity Risks, GAO‑22‑105162 (Washington D.C.: June 7, 2022).
[106]GAO, Public Health Emergencies: Data Management Challenges Impact National Response, GAO‑22‑106175 (Washington, D.C.: Sept. 22, 2022).
[107]Pandemic and All-Hazards Preparedness Act, Pub. L. No. 109-417, 120 Stat. 2831 (2006); Pandemic and All-Hazards Preparedness Reauthorization Act of 2013, Pub. L. No. 113-5, 127 Stat. 161 (2013); Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019, Pub. L. No. 116-22, 133 Stat. 905 (2019).
[108]See 42 U.S.C. § 247d-4.
[109]GAO, Public Health Information Technology: HHS Has Made Little Progress toward Implementing Enhanced Situational Awareness Network Capabilities, GAO‑17‑377 (Washington, D.C.: Sept. 6, 2017).
[111]HHS defines biosurveillance as the process of gathering, integrating, interpreting, and communicating essential information related to all-hazards threats or disease activity affecting human, animal, or plant health to achieve early detection and warning, contribute to overall situational awareness of the health aspects of an incident, and enable better decision-making at all levels.
[112]See 42 U.S.C. § 247d-4(c).
[113]GAO, COVID-19: Pandemic Lessons Highlight Need for Public Health Situational Awareness Network, GAO‑22‑104600 (Washington, D.C.: June 23, 2022).
[115]GAO‑22‑105397 and GAO, Medicaid in Times of Crisis, GAO‑21‑343SP (Washington, D.C.: Feb. 17, 2021).
[116]Pub. L. No. 116-127, div. F, § 6008, 134 Stat. 178, 208 (2020).
[117]Consolidated Appropriations Act, 2023, Pub. L. No. 117-328, § 5131, 136 Stat. 4459, 5949 (2022).
[118]GAO, Medicaid: Federal Oversight of State Eligibility Redeterminations Should Reflect Lessons Learned after COVID-19, GAO‑24‑106883, (Washington, D.C.: July 18, 2024).
[119]GAO, COVID-19: Opportunities to Improve Federal Response and Recovery Efforts, GAO‑20‑625 (Washington, D.C.: June 25, 2020) and Medicaid: Prototype Formula Would Provide Automatic Targeted Assistance to States during Economic Downturns, GAO‑12‑38 (Washington, D.C.: Nov. 10, 2011).
[120]For example, see GAO‑22‑105397 and GAO‑20‑625.
[121]GAO, COVID-19: U.S Territory Experiences Could Inform Future Federal Relief, GAO‑23‑106050 (Washington, D.C.: Sept. 19, 2023).
[122]GAO, COVID-19 Relief Funds: Lessons Learned Could Improve Future Distribution of Federal Emergency Relief to Tribal Recipients, GAO‑23‑105473 (Washington, D.C.: Dec. 15, 2022).
[124]GAO, COVID-19 in Nursing Homes: Experts Identified Actions Aimed at Improving Infection Prevention and Control, GAO‑23‑105613 (Washington, D.C.: Mar. 20, 2023).
[126]GAO, Medicaid: CMS Should Assess Effect of Increased Telehealth Use on Beneficiaries’ Quality of Care, GAO‑22‑104700 (Washington, D.C.: Mar. 31, 2022).
[127]GAO, Drug Safety: FDA Should Take Additional Steps to Improve Its Foreign Inspection Program, GAO‑22‑103611 (Washington, D.C.: Jan. 7, 2022).
[129]GAO, COVID-19: DOD Has Focused on Strategy and Oversight to Protect Military Servicemember Health, GAO‑21‑321 (Washington, D.C.: June 3, 2021).
[130]GAO, Defense Health Care: DOD Expanded Telehealth for Mental Health Care during the COVID-19 Pandemic, GAO‑22‑105149 (Washington, D.C.: Feb. 3, 2022).